Understanding PRK, Its Procedure, Benefits, Risks, and Evolution in Vision Correction
Introduction
Photorefractive keratectomy (PRK) is a type of refractive eye surgery designed to correct vision problems such as myopia (nearsightedness), hyperopia (farsightedness), and astigmatism. As one of the earliest forms of laser vision correction, PRK paved the way for modern procedures like LASIK and LASEK.
Historical Background
PRK was first performed in the late 1980s and received FDA approval in the United States in 1995. Its development represented a significant advance in ophthalmology, offering an alternative to eyeglasses and contact lenses for millions of people. The innovation of excimer lasers, which could precisely reshape the cornea, was key to PRK’s emergence. Although newer techniques have since evolved, PRK remains a respected and widely used procedure.
Understanding Vision and the Cornea
To appreciate the impact of PRK, it’s important to understand the basics of human vision. The cornea is the transparent, dome-shaped front part of the eye that helps focus light onto the retina. Imperfections in the cornea’s shape can cause refractive errors:
- Myopia (Nearsightedness): Distant objects appear blurry because the cornea is too steep, focusing light in front of the retina.
- Hyperopia (Farsightedness): Near objects are blurry because the cornea is too flat, focusing light behind the retina.
- Astigmatism: Irregular corneal curvature causes distorted or blurred vision at all distances.
PRK seeks to correct these errors by reshaping the cornea with laser precision.
The PRK Procedure
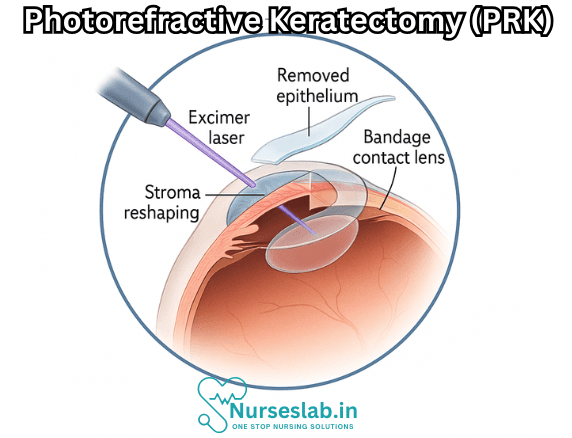
PRK is performed by an ophthalmologist in a clinical setting and typically takes less than 30 minutes per eye. The surgery involves several steps:
- Preparation: The patient receives numbing eye drops. A mild sedative may be given, but general anesthesia is not required.
- Removing the Epithelium: The outermost layer of the cornea (epithelium) is gently removed using a surgical instrument, brush, or alcohol solution. Unlike LASIK, no corneal flap is created.
- Laser Reshaping: An excimer laser is used to ablate (remove) microscopic amounts of corneal tissue, reshaping it to correct the refractive error. The laser is computer-guided and highly precise.
- Post-Laser Care: A soft contact lens is placed over the cornea to protect it and aid healing. The lens remains in place for several days while the epithelium regenerates.
Who is a Candidate for PRK?
PRK is suitable for adults with stable vision prescriptions who desire freedom from glasses or contact lenses. Ideal candidates typically:
- Have mild to moderate myopia, hyperopia, or astigmatism
- Have healthy corneas with adequate thickness
- Do not have eye diseases like glaucoma or cataracts
- Are not pregnant or nursing
- Do not have autoimmune disorders or conditions that impair healing
PRK may be preferred over LASIK for individuals with thin corneas, dry eyes, or those at risk for corneal trauma (e.g., athletes, military personnel).
Advantages of PRK
PRK offers several benefits:
- No Corneal Flap: Unlike LASIK, PRK does not require cutting a flap in the cornea, reducing the risk of flap complications.
- Suitable for Thin Corneas: PRK is ideal for patients whose corneas are too thin for LASIK.
- Lower Risk of Dry Eyes: The procedure affects fewer corneal nerves, lowering the risk of postoperative dry eye syndrome.
- Long-Term Stability: PRK outcomes are stable over time, with a low risk of regression or late complications.
- Effective for Active Lifestyles: Those involved in contact sports or high-risk activities often opt for PRK due to the absence of a flap that could be displaced.
Disadvantages and Risks
While PRK is safe and effective, it has some downsides:
- Longer Recovery: Vision recovery with PRK is slower than LASIK. It can take several days to weeks for clear vision to return as the epithelium heals.
- Discomfort: Patients may experience eye pain, tearing, and sensitivity to light for several days post-surgery.
- Risk of Haze: Some patients develop corneal haze, a cloudiness that may temporarily affect vision. Modern medications can minimize this risk.
- Infection or Delayed Healing: Though rare, infection or delayed epithelial healing can occur.
- Potential for Over- or Under-correction: As with all refractive surgeries, there is a small chance of not achieving the desired vision correction.
Comparison with LASIK and Other Procedures
LASIK (Laser-Assisted In Situ Keratomileusis) is the most widely known laser vision correction technique. Compared to PRK:
- LASIK: Involves creating a corneal flap, faster visual recovery, less initial discomfort, but carries a risk of flap-related complications.
- LASEK: Similar to PRK, but the epithelium is preserved and repositioned after laser treatment.
- SMILE: A newer technique, Small Incision Lenticule Extraction, uses a femtosecond laser to correct vision through a tiny incision.
PRK remains a preferred option when corneal thickness or eye health makes LASIK unsuitable.
Recovery Process
Recovery from PRK typically involves:
- First Few Days: The protective contact lens stays in place while the epithelium regenerates. Patients may experience discomfort, blurred vision, tearing, and sensitivity to light.
- Medications: Prescribed antibiotic and anti-inflammatory eye drops prevent infection and reduce inflammation.
- Follow-up Visits: A series of checkups ensures proper healing and monitors for complications.
- Visual Improvement: Most patients notice significant vision improvement within one to two weeks, although optimal clarity may take a month or more.
- Activity Restrictions: Patients should avoid swimming, contact sports, and eye makeup until cleared by their doctor.
Long-term results are typically excellent, with patients achieving 20/20 vision or better.
Potential Complications
Although serious complications are rare, potential risks include:
- Infection
- Corneal haze or scarring
- Chronic dry eye
- Glare, halos, or night vision problems
- Regression of refractive correction
- Under- or over-correction
The risk of complications can be minimized by choosing an experienced surgeon and adhering closely to postoperative care instructions.
Long-Term Outcomes
Studies show that PRK delivers stable and lasting results. Most patients enjoy decades of improved vision. The removal of the epithelium does not weaken the cornea long-term, and the risk of late complications is minimal. In rare cases, enhancement procedures may be needed to fine-tune vision correction.
Cost Considerations
PRK is generally comparable in cost to LASIK, although prices vary by location, surgeon experience, and the technology used. Insurance plans typically do not cover refractive surgery unless medically necessary, so patients must pay out of pocket. Many clinics offer financing options to make the procedure accessible.
Advances and Innovations in PRK
Recent advances in laser technology have improved the safety, precision, and comfort of PRK. Custom wavefront-guided lasers allow for more personalized treatments, potentially enhancing visual outcomes and reducing side effects. Improved postoperative medications further reduce discomfort and the risk of haze.
PRK in Special Populations
PRK is often recommended for individuals who cannot undergo LASIK due to thin corneas, high risk of trauma, or dry eye issues. It is also preferred for certain professions, such as athletes or military personnel, where flap-related complications could affect job performance.
Nursing Care of Patients Undergoing Photorefractive Keratectomy (PRK)
The recovery from PRK is generally longer and slightly more uncomfortable due to the removal of the epithelium, which needs days to regenerate. Proper nursing care is essential to manage pain, monitor for infection, educate patients, and foster a supportive environment during the recovery process.
Preoperative Nursing Care
1. Patient Assessment and Education
- Assess the patient’s visual acuity, medical history, allergies, and medications.
- Explain the PRK procedure, expected outcomes, and the differences from other refractive surgeries.
- Review preoperative instructions, including discontinuation of contact lenses (usually 1-2 weeks before surgery), avoidance of makeup, lotions, and perfumes, and arranging for transportation home post-procedure.
2. Psychological Preparation
- Address patient anxiety by providing reassurance, detailed explanations, and answering questions.
- Assess patient expectations and clarify realistic outcomes to prevent dissatisfaction.
Immediate Postoperative Nursing Care
1. Pain Management
- PRK is associated with moderate discomfort and photophobia (light sensitivity) for several days post-surgery.
- Administer prescribed analgesics, such as oral pain relievers or topical nonsteroidal anti-inflammatory drugs (NSAIDs), as ordered.
- Advise use of cold compresses and keeping the eyes closed or in a dim environment to relieve discomfort.
- Reinforce the importance of not rubbing the eyes, as the corneal epithelium is healing.
2. Application and Care of Bandage Contact Lens
- A bandage contact lens is typically placed over the cornea to promote healing and reduce pain.
- Educate the patient on the purpose of the lens and the importance of not removing or dislodging it.
- Monitor for signs of lens displacement, intolerance, or infection.
3. Administration of Eye Medications
- Instill prescribed antibiotic and anti-inflammatory eye drops to prevent infection and control inflammation.
- Demonstrate the correct technique for eye drop instillation, emphasizing hand hygiene and avoiding contamination of the bottle tip.
- Schedule medication administration at prescribed intervals and document compliance.
4. Monitoring for Complications
- Observe for signs of infection: increased pain, redness, discharge, or vision changes.
- Monitor for corneal haze, delayed epithelial healing, or significant vision loss.
- Ensure prompt notification to the ophthalmologist if complications are suspected.
Ongoing Postoperative Nursing Care
1. Patient Education and Support
- Instruct on the importance of adhering to the prescribed medication regimen, including duration and frequency.
- Discuss the expected course of recovery, including fluctuating vision, photophobia, and gradual return of clarity over several weeks.
- Advise on activity restrictions: avoid swimming, hot tubs, contact sports, and environments with dust or fumes until cleared by the surgeon.
- Reinforce the need to wear sunglasses for UV protection and comfort in bright environments.
2. Personal Hygiene and Eye Protection
- Encourage meticulous hand hygiene before touching the face or administering drops.
- Advise against eye makeup, facial creams, or lotions near the eyes until complete healing is confirmed.
- Teach patients to avoid getting water or soap in the eyes during bathing.
3. Follow-up Care
- Schedule and emphasize the importance of timely follow-up visits for monitoring healing and early detection of complications.
- During follow-up assessments, check for epithelial regrowth, corneal clarity, and refractive outcome.
- Assist with documentation and communication between the patient and healthcare team.
Emotional and Psychosocial Support
- Recognize that visual recovery may take several weeks, which can be stressful for patients accustomed to instant results from other types of surgeries.
- Provide emotional reassurance about the expected temporary vision fluctuations and discomfort.
- Foster a supportive atmosphere for patients to express their concerns and ask questions.
- Refer patients to support groups or counseling services if anxiety or frustration is significant.
Potential Complications and Nursing Interventions
1. Corneal Haze
- Educate patients about the risk of corneal haze (cloudiness) during healing, which may transiently affect vision.
- Encourage compliance with steroid eye drops, which help minimize haze formation.
- Monitor for persistent vision changes and report these to the provider promptly.
2. Delayed Epithelial Healing
- Monitor the healing process and educate patients about the importance of resting the eyes and avoiding trauma.
- Notify the ophthalmologist if healing is not progressing as expected.
3. Infection
- Reinforce aseptic technique for all eye care procedures.
- Educate on the signs and symptoms of infection: severe pain, redness, swelling, discharge, and sudden vision loss.
- Arrange immediate medical attention if infection is suspected.
4. Dry Eye Syndrome
- Inform patients about the likelihood of temporary dry eye and the use of preservative-free lubricating drops.
- Assess for symptoms of dryness, grittiness, and discomfort during follow-up visits.
- Monitor for long-term dry eye and refer for additional management if symptoms persist beyond the usual healing period.
Special Considerations
- Consider patients with co-morbidities (such as diabetes or autoimmune disorders) as potentially at higher risk for delayed healing or complications.
- Coordinate care with the wider healthcare team to address systemic issues that may affect ocular healing.
- Advocate for patient safety and well-being throughout the perioperative period.
Discharge Planning and Home Care Instructions
- Provide written and verbal instructions for home care, emphasizing medication schedules, signs of complications, and activity restrictions.
- Supply emergency contact information and clearly state when to seek urgent medical attention.
- Arrange for timely follow-up appointments and ensure the patient understands the importance of attending.
- Assess the patient’s ability to self-administer eye drops or coordinate with family members or caregivers as needed.
REFERENCES
- American Academy of Ophthalmology EyeSmart. What is Photorefractive Keratectomy?. https://www.aao.org/eye-health/treatments/photorefractive-keratectomy-prk Published 4/25/2023.
- American Academy of Ophthalmology EyeWiki. Photorefractive Keratectomy. https://eyewiki.aao.org/Photorefractive_Keratectomy. Updated 3/4/2024.
- Somani SN, Moshirfar M, Patel BC. Photorefractive Keratectomy. [Updated 2023 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK549887/
- Joffe SN. The 25th Anniversary of Laser Vision Correction in the United States. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7982707/. Clin Ophthalmol. 2021;15:1163-1172.
- McHugh J, Pringle E. Lasers in Ophthalmology. In: Riordan-Eva P, Augsburger JJ, eds. Vaughan & Asbury’s General Ophthalmology, 19th ed. McGraw Hill; 2017.
- Somani SN, Moshirfar M, Patel BC. Photorefractive Keratectomy. https://www.ncbi.nlm.nih.gov/books/NBK549887/. 2023 Jul 18. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan.
- Tomás-Juan J, Murueta-Goyena Larrañaga A, Hanneken L. Corneal Regeneration After Photorefractive Keratectomy: A Review. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4502084/. J Optom. 2015 Jul-Sep;8(3):149-169.
- Boyd K. (2023). What is photorefractive keratectomy (PRK)?
https://www.aao.org/eye-health/treatments/photorefractive-keratectomy-prk
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





