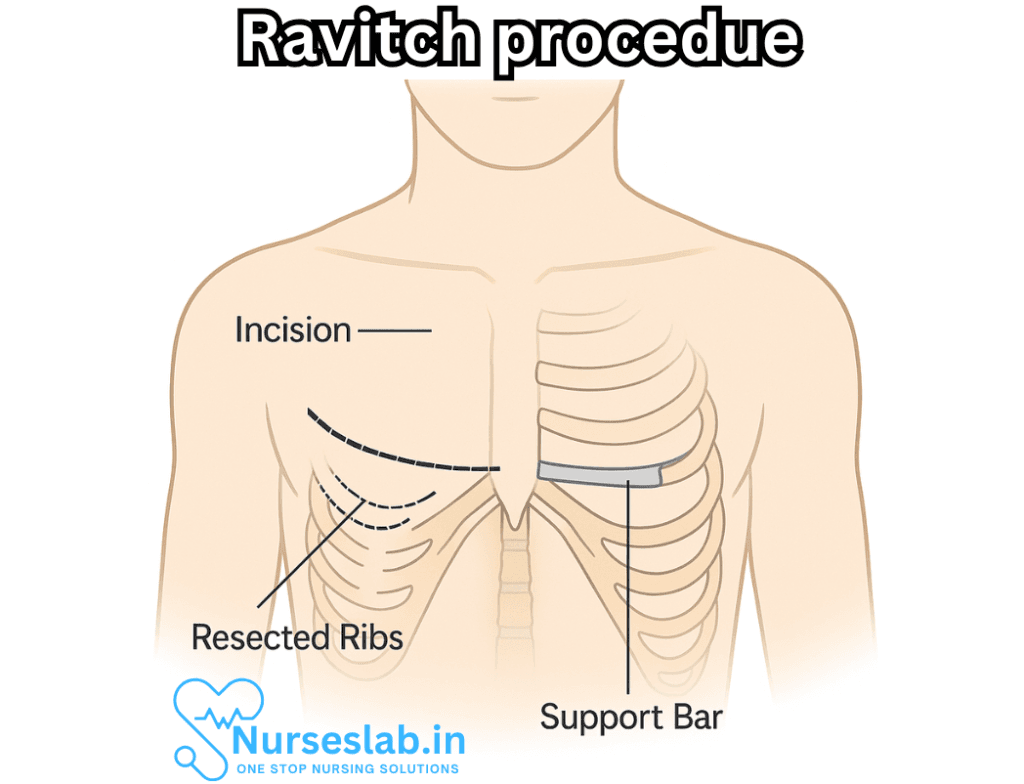
The Ravitch procedure is an open surgical correction of chest wall deformities. It involves:
- Making a horizontal incision across the chest
- Removing abnormal costal cartilage that causes the deformity
- Repositioning the sternum (breastbone) into a normal anatomical position
- Inserting a metal bar or plate beneath the sternum to maintain its new shape (typically removed after 6–12 months)
It’s often performed on adolescents and young adults (ages 13–22) when the deformity is severe or when less invasive options like the Nuss procedure aren’t suitable.
This document provides a comprehensive review of the Ravitch procedure, including its historical development, indications, surgical technique, expected outcomes, potential complications, and post-operative care.
Historical Context
The Ravitch procedure is named after Dr. Mark M. Ravitch, an American surgeon who described this surgical method in the 1940s and 1950s. At that time, surgery for pectus deformities was in its infancy, and Dr. Ravitch’s approach set a new standard for anatomical correction of the chest wall, vastly improving both functional and cosmetic results for affected patients.
Indications for the Ravitch Procedure
The Ravitch procedure is primarily indicated for:
- Pectus excavatum (depressed sternum)
- Pectus carinatum (protruding sternum)
- Complex or asymmetric chest wall deformities
- Recurrent deformity after failed minimally invasive repair (such as the Nuss procedure)
- Severe deformity with rigid or calcified costal cartilages, often found in adults
Candidates for the Ravitch procedure often include adolescents and adults, particularly when the chest wall has become less malleable and when non-surgical or minimally invasive treatments are unlikely to succeed.
Surgical Technique
The Ravitch procedure is an open surgical technique performed under general anesthesia. The main steps are as follows:
1. Incision and Exposure
A transverse (horizontal) incision is made across the chest, typically just above the sternum. The pectoral (chest) muscles are carefully divided or elevated to expose the underlying costal cartilages and sternum.
2. Resection of Abnormal Cartilage
The deformed costal cartilages (the cartilage portions of the ribs connecting to the sternum) are identified. These cartilages are carefully resected (removed) while preserving the inner lining (perichondrium), which allows for potential regrowth of healthy cartilage.
3. Sternal Manipulation and Osteotomy
The sternum is then mobilized. In many cases, a wedge-shaped piece of bone is removed (sternal osteotomy) to allow the sternum to be repositioned in a more natural, anatomically correct position. The sternum may be secured in place with temporary support, such as a metal or absorbable strut, to maintain the correction during healing.
4. Chest Wall Stabilization
To prevent recurrence of the deformity, stabilizing devices (struts or bars) are sometimes placed and fixed to the ribs or sternum. These supports are generally removed several months after surgery, once the chest wall has healed.
5. Closure
The pectoral muscles are reattached, and the incision is closed in layers. Surgical drains may be placed to prevent fluid accumulation.
Post-Operative Care
After surgery, patients are typically monitored in the hospital for several days. Pain management is crucial, often involving a combination of intravenous and oral medications. Early mobilization is encouraged to reduce the risk of complications such as pneumonia or blood clots.
Key aspects of post-operative care include:
- Pain control
- Wound care and monitoring for infection
- Chest physiotherapy and breathing exercises
- Gradual return to normal activity, avoiding heavy lifting for several weeks
- Regular follow-up visits with the surgical team
Expected Outcomes
The Ravitch procedure has been shown to provide excellent cosmetic and symptomatic improvement in most patients. The chest wall is recontoured to a more typical appearance, and symptoms related to compression of the heart and lungs (such as shortness of breath or exercise intolerance) are often alleviated.
Psychological benefits are notable, with many patients reporting improved self-esteem and body image following successful correction.
Potential Complications
As with any major surgery, the Ravitch procedure carries certain risks. Potential complications include:
- Infection at the surgical site
- Bleeding or hematoma formation
- Pneumothorax (collapsed lung)
- Bar or strut displacement
- Persistent pain or discomfort
- Scarring and keloid formation
- Recurrence of chest wall deformity
- Reaction to anesthesia
Most complications are rare, and careful surgical technique, along with diligent post-operative care, minimizes their occurrence.
Comparison with Other Procedures
The Ravitch procedure is considered a more invasive alternative to the Nuss procedure, which involves the insertion of a curved metal bar beneath the sternum to correct pectus excavatum without cartilage resection. While the Nuss technique is often favored in pediatric and adolescent patients due to its minimally invasive nature, the Ravitch procedure remains the treatment of choice for adults, patients with very rigid or complex deformities, or those for whom the Nuss procedure has failed.
Long-Term Follow-Up
Patients who undergo the Ravitch procedure require long-term follow-up to assess chest wall development, function, and cosmetic outcome. Most patients enjoy lasting correction, but recurrence can occur, particularly if the procedure is done at a very young age or if post-operative instructions are not followed.
Patient Selection and Counseling
Adequate patient selection is crucial for optimal outcomes. Discussion with the patient (and family, if appropriate) should cover the risks, benefits, expected recovery, and the possibility of needing additional procedures. Setting realistic expectations helps ensure satisfaction with the results.
Nursing Care of a Patient Undergoing the Ravitch Procedure
Unlike the minimally invasive Nuss procedure, the Ravitch procedure is an open surgery that involves removing abnormal cartilaginous structures and repositioning the sternum. Given the invasive nature of the operation, meticulous nursing care is essential across all perioperative phases to ensure optimal recovery, prevent complications, and provide holistic support to both patients and their families.
Preoperative Nursing Care
Patient Assessment
- Perform a thorough physical assessment, focusing on respiratory and cardiovascular function.
- Obtain a comprehensive medical history, including any history of respiratory illnesses, cardiac conditions, allergies, and previous surgeries.
- Document baseline vital signs, oxygen saturation, and pain levels.
- Assess psychological readiness and address any anxiety regarding surgery by providing education and emotional support.
Preoperative Education
- Explain the nature and purpose of the Ravitch procedure using age-appropriate language.
- Discuss perioperative routines, such as fasting, skin preparation, and possible insertion of intravenous lines or catheters.
- Describe the expected course of recovery, including pain management strategies, activity restrictions, and breathing exercises.
- Inform the patient and their family about the potential need for chest tubes and the presence of surgical drains.
Preparation for Surgery
- Ensure all required preoperative laboratory and imaging investigations are completed and reviewed.
- Confirm informed consent has been obtained.
- Perform skin preparation as per protocol.
- Administer preoperative medications as prescribed (e.g., antibiotics, anxiolytics).
- Encourage the patient to practice deep breathing and coughing exercises to facilitate postoperative respiratory care.
Intraoperative Nursing Care
Operating Room Preparation
- Confirm patient identity, operative site, and surgical procedure as part of the surgical safety checklist.
- Assist with positioning the patient supine on the operating table and ensure pressure points are padded to prevent injury.
- Apply monitoring devices for continuous assessment of vital signs, ECG, and oxygen saturation.
Assistance During Surgery
- Support the surgical team by providing sterile instruments and supplies as needed.
- Monitor the patient’s hemodynamic status and promptly report any changes to the surgical team.
- Document intraoperative events, medications administered, and fluid balance accurately.
Postoperative Nursing Care
Immediate Postoperative Care
- Transfer the patient to the post-anesthesia care unit (PACU) for close monitoring.
- Continuously monitor airway patency, respiratory rate, oxygen saturation, and depth of respiration.
- Monitor cardiovascular status: blood pressure, heart rate, and rhythm.
- Assess for signs of bleeding, shock, or cardiac complications.
- Monitor the surgical site for bleeding, swelling, or drainage.
- Check chest tubes and drains for patency, output, and signs of infection.
- Monitor pain levels and administer analgesia as prescribed using validated pain assessment tools.
- Encourage gentle deep breathing and coughing exercises to prevent atelectasis and pneumonia.
- Observe for complications such as pneumothorax, hemothorax, or wound infection.
Pain Management
- Anticipate significant postoperative pain due to the invasiveness of the procedure.
- Administer prescribed analgesics, which may include opioids, NSAIDs, and adjunctive medications.
- Assess pain frequently and titrate medications accordingly.
- Encourage non-pharmacological pain relief methods such as relaxation techniques, guided imagery, and the use of pillows for support.
- Educate the patient on the importance of pain control for effective mobilization and respiratory exercises.
Respiratory Care
- Promote effective airway clearance by encouraging deep breathing, incentive spirometry, and controlled coughing.
- Monitor for respiratory distress, diminished breath sounds, or abnormal chest movements.
- Assist with chest physiotherapy as ordered.
- Keep the head of the bed elevated to facilitate lung expansion and reduce the risk of aspiration.
- Ensure chest tubes are functioning properly and document output characteristics.
Wound and Drain Care
- Monitor surgical incisions for redness, swelling, increased pain, or purulent discharge.
- Change dressings according to sterile technique and protocol.
- Assess and document the output from surgical drains and notify the surgeon of any abrupt changes.
- Secure chest tubes and drainage systems to prevent accidental dislodgement.
Mobility and Activity
- Encourage early, gradual ambulation as tolerated to promote circulation and prevent thromboembolic events.
- Assist the patient with movement to avoid excessive strain on the chest wall.
- Educate the patient and family on activity restrictions, including avoidance of contact sports or heavy lifting until cleared by the surgeon.
- Ensure proper body mechanics and use of assistive devices as needed.
Monitoring for Complications
- Be vigilant for signs of infection (fever, increased wound redness, purulent drainage).
- Monitor for respiratory or cardiac complications, such as arrhythmias, pneumothorax, or pleural effusion.
- Assess for deep vein thrombosis (DVT) by checking for calf pain, swelling, and redness.
- Observe for signs of psychosocial distress or postoperative depression.
Patient and Family Education
- Provide clear instructions on wound care, drain management, and signs of complications to report.
- Teach the importance of medication adherence, including pain management and antibiotics.
- Encourage continuation of prescribed respiratory exercises and gradual resumption of activities.
- Discuss the importance of follow-up appointments for assessment of healing and possible removal of stabilizing hardware.
- Offer resources for psychological support and counseling if needed.
Discharge Planning and Long-Term Care
Criteria for Discharge
- Pain is well-controlled with oral medications.
- The patient is able to breathe effectively with clear lung sounds and no respiratory compromise.
- Wounds are healing appropriately, and drain output is minimal or within expected range.
- The patient and family demonstrate understanding and ability to manage care at home.
Home Care Instructions
- Continue regular wound checks and keep incisions clean and dry.
- Monitor for signs of infection or complications and seek prompt medical attention if they arise.
- Adhere to prescribed activity restrictions and gradually resume daily activities as tolerated.
- Follow up with the surgical team for ongoing assessment, imaging, and hardware removal if indicated.
- Engage in continued respiratory exercises to maintain optimal pulmonary function.
Long-Term Considerations
- Monitor for late complications, including chest wall instability, recurrence of deformity, or hardware displacement.
- Provide psychological support and counseling for body image concerns, especially in pediatric and adolescent patients.
- Reinforce the importance of maintaining a healthy lifestyle, including physical activity within prescribed limits.
Psychosocial Support
- Acknowledge the emotional impact of chest wall surgery, particularly for children and adolescents.
- Facilitate open communication between the patient, family, and healthcare team.
- Offer support groups, counseling services, and educational materials to aid in coping and adjustment.
- Monitor for and address symptoms of anxiety, depression, or altered self-image throughout the recovery process.
REFERENCES
- Fenikowski D, Tomaszek L. Factors Related to Anxiety in Paediatric Patients and Their Parents before and after a Modified Ravitch Procedure-A Single-Centre Cohort Study. https://pubmed.ncbi.nlm.nih.gov/36554581/. Int J Environ Res Public Health. 2022 Dec 12;19(24):16701.
- Kanagaratnam A, Phan S, Tchantchaleishvili V, Phan K. Ravitch versus Nuss procedure for pectus excavatum: systematic review and meta-analysis. https://pubmed.ncbi.nlm.nih.gov/27747174/ [published correction appears in Ann Cardiothorac Surg. 2016 Nov;5(6):593]. Ann Cardiothorac Surg. 2016 Sep;5(5):409-421.
- Rettig RL, Yang CJ, Ashfaq A, Sydorak RM. Cryoablation is associated with shorter length-of-stay and reduced opioid use after the Ravitch procedure. https://pubmed.ncbi.nlm.nih.gov/35379492/. J Pediatr Surg. 2022 Jul;57(7):1258-1263.
- Jones J, Hacking C, Iqbal S, et al. Ravitch procedure. Reference article, Radiopaedia.org (Accessed on 19 Feb 2025) https://doi.org/10.53347/rID-13665
- Sharma G, Carter YM. Pectus Excavatum. https://pubmed.ncbi.nlm.nih.gov/28613668/. 2023 Jul 17. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan.
- Sollie ZW, Gleason F, Donahue JM, Wei B. Evolution of technique and results after permanent open repair for pectus deformities. https://pubmed.ncbi.nlm.nih.gov/35403047/. JTCVS Tech. 2022 Jan 19;12:212-219.
- Sultan I, Yang SC. Congenital Chest Wall Anomalies. In: Yuh DD, Vricella LA, Yang SC, Doty JR, eds. Johns Hopkins Textbook of Cardiothoracic Surgery. 2nd ed. McGraw-Hill Education; 2014.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





