Introduction
A splenectomy is a surgical procedure involving the removal of the spleen, an organ located in the upper left quadrant of the abdomen, just beneath the ribcage. The spleen is an integral part of the lymphatic system and plays a vital role in immune function and blood filtration. While not essential for survival, its removal has significant implications for a person’s health, necessitating adjustments in lifestyle and medical care.
Anatomy and Function of the Spleen
The spleen is a fist-sized, soft, and highly vascular organ. It is responsible for several key functions:
- Blood Filtration: The spleen filters old or damaged red blood cells from the bloodstream and recycles iron.
- Immunological Role: It produces lymphocytes (white blood cells), aids in mounting immune responses, and stores immune cells that respond to pathogens.
- Blood Storage: The spleen acts as a reservoir for blood and platelets, releasing them into circulation as needed, such as during hemorrhage.
- Removal of Blood-Borne Pathogens: Macrophages in the spleen engulf bacteria, viruses, and other foreign particles.
Indications for Splenectomy
Splenectomy may be indicated for a variety of medical reasons, broadly categorized as follows:
1. Trauma
Trauma is the most common cause for emergency splenectomy. Blunt abdominal injuries such as those from car accidents, falls, or sports injuries can cause splenic rupture and life-threatening internal bleeding.
2. Haematological Disorders
Several blood diseases require splenectomy:
- Hereditary Spherocytosis: A condition where abnormal red blood cells are destroyed in the spleen, leading to anemia.
- Idiopathic Thrombocytopenic Purpura (ITP): The spleen destroys platelets, causing a risk of bleeding. If medications fail, splenectomy is considered.
- Thalassemia and Sickle Cell Disease: These disorders may lead to an enlarged or overactive spleen, contributing to anemia and other complications.
3. Malignancy
Cancers such as lymphoma, leukemia, or metastatic disease can infiltrate the spleen. Sometimes, the organ is removed during staging or treatment.
4. Hypersplenism
This refers to an overactive spleen that destroys blood cells excessively, causing cytopenias (low blood cell counts).
5. Other Indications
- Cysts or Abscesses: Non-cancerous growths or infections unresponsive to treatment.
- Autoimmune Diseases: For example, in certain cases of systemic lupus erythematosus or rheumatoid arthritis.
- Diagnostic Purposes: Rarely, when the cause of splenic enlargement or dysfunction is unclear.
Types of Splenectomy
There are two main approaches:
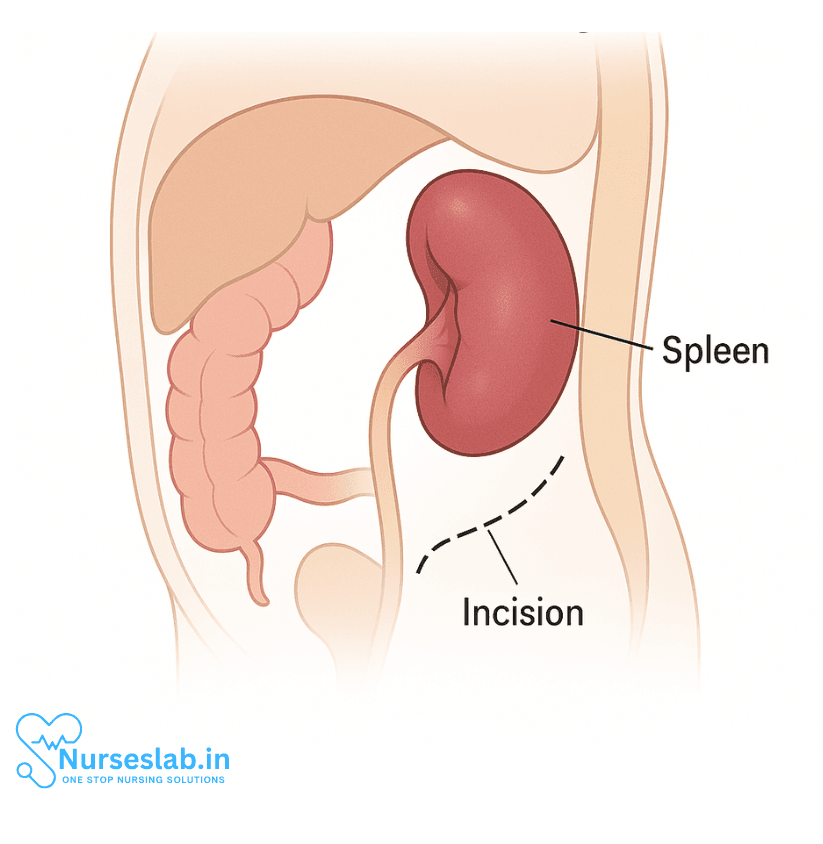
- Open Splenectomy: The traditional technique, involving a large incision in the abdomen to access and remove the spleen. Used in trauma or when the spleen is greatly enlarged.
- Laparoscopic Splenectomy: A minimally invasive procedure utilizing small incisions and specialized instruments with a camera. It offers faster recovery, less pain, and smaller scars. However, it may not be suitable in emergency situations or with massive spleens.
Preoperative Considerations
Before the operation, thorough evaluation and preparation are necessary:
- Vaccinations: The spleen plays a crucial role in fighting infections, especially from encapsulated bacteria. Patients are vaccinated against Streptococcus pneumoniae, Haemophilus influenzae type b, and Neisseria meningitidis before elective splenectomy.
- Blood Tests: To assess blood counts and overall health.
- Imaging: Ultrasound or CT scans to visualize the spleen and plan the surgery.
- Discussion of Risks and Benefits: Patients must understand the implications, possible complications, and life after splenectomy.
The Surgical Procedure
The procedure typically involves the following steps:
- Anesthesia: General anesthesia renders the patient unconscious.
- Incision: Depending on the approach (open or laparoscopic), the surgeon makes an incision in the abdomen.
- Mobilization: The ligaments anchoring the spleen are carefully divided, and blood vessels supplying the organ are ligated.
- Removal: The spleen is removed. In laparoscopic cases, it may be placed in a retrieval bag and morcellated (cut into pieces) for extraction through small incisions.
- Hemostasis and Closure: Bleeding is controlled, and the incision(s) are closed.
Surgery duration can range from one to several hours, depending on complexity.
Postoperative Care and Recovery
After splenectomy, care focuses on recovery and infection prevention.
- Hospital Stay: Patients typically remain hospitalized for 2–7 days, depending on their condition and surgery type.
- Pain Management: Analgesics are used as needed.
- Early Mobilization: Walking and light activity are encouraged to prevent complications like blood clots.
- Wound Care: Incisions are monitored for signs of infection.
- Monitoring for Complications: Such as bleeding, infection, or injury to surrounding organs.
Risks and Complications
While splenectomy can be life-saving, it entails certain risks:
- Infection: Without the spleen, the risk of severe bacterial infections (overwhelming post-splenectomy infection, OPSI) significantly increases. Prompt medical attention for fevers is essential.
- Bleeding: The spleen is highly vascular, so bleeding during and after surgery is a concern.
- Thrombosis: There is an increased risk of blood clots, including deep vein thrombosis and pulmonary embolism.
- Injury to Surrounding Organs: Such as the stomach, pancreas, or colon.
- Hernia at the Incision Site: Particularly with open surgery.
Long-Term Considerations After Splenectomy
Losing the spleen has permanent effects, particularly on the immune system.
- Vaccination: Continued updates for pneumococcal, meningococcal, and Haemophilus influenzae vaccines are required. Annual influenza vaccination is strongly recommended.
- Antibiotic Prophylaxis: Some individuals, especially children, may be advised to take daily antibiotics long-term or at least for the first few years after surgery.
- Infection Awareness: Patients are taught to seek medical attention immediately if they develop fever or signs of infection.
- Medical Identification: Wearing a medical alert bracelet indicating asplenia (absence of spleen) can help in emergencies.
- Travel Precautions: Special care is needed when traveling, particularly to areas with malaria or other infectious risks. Prophylactic medications may be necessary.
Life Without a Spleen
Most people live full, active lives after splenectomy. However, lifelong vigilance regarding infection is crucial. Children, the elderly, and immunocompromised individuals are at highest risk for severe infection.
Diet and Lifestyle
There are no strict dietary restrictions, but maintaining a healthy, balanced diet supports overall immune function. Regular exercise and proper wound care are encouraged.
Follow-Up Care
Routine medical follow-ups ensure vaccinations are up to date, blood counts are monitored, and any long-term complications are managed proactively.
Special Considerations in Pediatric Patients
Children are particularly vulnerable to infections after splenectomy. Preventive strategies vaccination, prophylactic antibiotics, and parental education are especially emphasized in this group.
Recent Advances and Alternatives
Partial Splenectomy
In select cases, only part of the spleen may be removed, preserving some immunological function.
Non-Operative Management
For certain injuries or conditions, conservative treatment (observation, embolization) might avoid the need for surgery, preserving the spleen’s function.
Nursing Care of Patients with Splenectomy
The role of the nurse in caring for a patient who has undergone splenectomy is critical in both the immediate post-operative period and for long-term health maintenance.
Preoperative Considerations
- Patient Education: Prepare the patient and family by explaining the procedure, expected outcomes, and potential complications.
- Immunization: Ensure the patient has received appropriate immunizations (e.g., pneumococcal, meningococcal, and Haemophilus influenzae type b vaccines) at least two weeks prior to elective splenectomy, as the risk for infections increases after spleen removal.
- Baseline Assessment: Conduct a thorough assessment including vital signs, laboratory investigations (CBC, coagulation profile), and identification of infection risk factors.
Immediate Postoperative Nursing Care
Pain Management
- Monitor pain levels regularly using a standardized pain scale.
- Administer prescribed analgesics on schedule, adjusting dosage as necessary for comfort.
- Encourage non-pharmacological pain relief measures, such as deep breathing exercises and repositioning.
Monitoring Vital Signs and Hemodynamic Status
- Monitor the patient’s vital signs frequently, particularly during the first 24-48 hours post-operation.
- Watch for signs of shock, bleeding, or infection (tachycardia, hypotension, decreased urine output, pallor, or altered mental status).
- Assess the surgical wound for excessive bleeding, swelling, or signs of infection.
Respiratory Care
- Encourage deep breathing exercises and coughing to prevent atelectasis and pneumonia.
- Assist with early mobilization, as tolerated, to reduce the risk of respiratory complications and deep vein thrombosis.
Prevention of Infection
- Observe strict aseptic technique during all procedures and wound care.
- Monitor temperature and other signs of infection closely.
- Educate the patient and family about the importance of reporting fever or signs of infection immediately, as post-splenectomy patients are at increased risk for life-threatening infections.
Fluid and Electrolyte Balance
- Monitor input and output closely, ensuring adequate hydration.
- Assess laboratory values regularly for any imbalances and report abnormal findings promptly.
Wound Care
- Inspect the surgical site for bleeding, hematoma, or infection.
- Change dressings per protocol and keep the area clean and dry.
Early Mobilization
- Encourage gradual movement as soon as the patient is able, starting with sitting up in bed and progressing to walking.
- Use anti-embolism stockings or compression devices as prescribed to reduce the risk of deep vein thrombosis.
Long-Term Nursing Care and Health Maintenance
Infection Prevention and Management
- Immunization: Reinforce the need for regular booster vaccines (pneumococcal, meningococcal, Hib), annual influenza vaccination, and any additional vaccines as recommended by the physician.
- Antibiotic Prophylaxis: Some patients, especially children, may require long-term prophylactic antibiotics. Ensure the patient understands the regimen and the importance of adherence.
- Education: Instruct the patient on recognizing early signs of infection (fever, chills, sore throat, cough, malaise) and seeking immediate medical attention if these occur.
- Medical Alert: Encourage the use of a medical alert bracelet or card indicating asplenic status for emergencies.
Blood Clot Prevention
- Monitor for signs and symptoms of thrombosis, such as leg swelling, redness, and pain.
- Encourage regular movement and, where appropriate, use anticoagulant therapy as ordered.
Patient and Family Education
- Travel Precautions: Advise patients to consult their healthcare provider before traveling to areas where certain infections (e.g., malaria, babesiosis) are more common. Prophylactic antibiotics or vaccinations may be necessary.
- Animal Bites: Advise immediate medical attention for animal or human bites, as these can lead to severe infections in asplenic individuals.
- Routine Health Maintenance: Emphasize the importance of regular follow-up visits and health screenings.
Lifestyle and Psychosocial Considerations
- Address concerns about susceptibility to infections and provide emotional support.
- Encourage healthy habits, such as proper nutrition, adequate rest, and stress management, to strengthen the immune system.
- Help patients build a support system to address any anxiety or uncertainties regarding their health status.
Potential Complications Post-Splenectomy
- Overwhelming Post-Splenectomy Infection (OPSI): This is a rapid, severe infection that can be fatal. Patients must be taught to recognize its signs and seek help immediately.
- Thromboembolic Events: Increased risk of blood clots due to alterations in blood cell counts following splenectomy.
- Hematological Changes: Persistent increase in platelet count (thrombocytosis) may occur, requiring monitoring.
- Other Infections: Higher susceptibility to encapsulated bacterial infections (e.g., Streptococcus pneumoniae, Neisseria meningitidis, Haemophilus influenzae).
Coordination with the Healthcare Team
- Collaborate with physicians, pharmacists, and other healthcare professionals to tailor a comprehensive care plan.
- Ensure all team members are aware of the patient’s asplenic status to optimize infection prevention strategies.
- Communicate changes in the patient’s condition promptly to the appropriate team members.
Discharge Planning and Community Care
- Ensure the patient receives clear instructions regarding wound care, signs of complications, and when to seek help.
- Arrange for home health nursing follow-up if needed, especially in patients at higher risk for complications.
- Provide written materials for patient and caregiver reference.
REFERENCES
- Bonanni P, Grazzini M, Niccolai G, et al. Recommended vaccinations for asplenic and hyposplenic adult patients. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5328222/. Hum Vaccin Immunother. 2017;13(2):359-368.
- Camejo L, Nandeesha N, Phan K, et al. Infectious outcomes after splenectomy for trauma, splenectomy for disease and splenectomy with distal pancreatectomy. https://pubmed.ncbi.nlm.nih.gov/35075620/. Langenbecks Arch Surg. 2022;407(4):1685-1691.
- Society of American Gastrointestinal and Endoscopic Surgeons. Spleen Removal (Splenectomy). http://www.sages.org/publications/patient-information/patient-information-for-laparoscopic-spleen-removal-splenectomy-from-sages.
- Tahir F, Ahmed J, Malik F. Post-splenectomy Sepsis: A Review of the Literature. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7059871/. Cureus. 2020;12(2):e6898. Published 2020 Feb 6.
- Yi SL, Lopez JL. Splenectomy. https://www.ncbi.nlm.nih.gov/books/NBK560824/. 2023 Jul 4. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





