Transforaminal Lumbar Interbody Fusion (TLIF) stands as a significant advancement in the field of spinal surgery, offering relief for patients suffering from a range of degenerative and structural spinal disorders. As a technique designed to address lumbar spine instability and nerve compression, TLIF has gained prominence for its blend of effectiveness, safety, and the potential for rapid recovery compared to more traditional surgical approaches. This document explores TLIF in detail, encompassing its history, indications, surgical technique, advantages, complications, and the patient experience from diagnosis through recovery.
Introduction to TLIF
Transforaminal Lumbar Interbody Fusion, abbreviated as TLIF, is a type of spinal fusion surgery performed on the lower (lumbar) spine. Its primary goal is to stabilize the vertebral bones by fusing them together, often addressing conditions that have not responded to conservative treatments such as physical therapy, medication, or less invasive procedures.
Historical Context
The concept of spinal fusion dates back to the early twentieth century, with the first documented lumbar fusions occurring in the 1910s. Over the decades, surgical techniques have evolved to minimize tissue disruption, improve spinal stability, and enhance patient outcomes. TLIF was first described in the late 1990s as a modification of the Posterior Lumbar Interbody Fusion (PLIF). The key advancement with TLIF was its approach, using a more lateral (transforaminal) route to access the disc space, thereby reducing nerve and spinal cord manipulation and lowering the risk of complications.
Indications for TLIF
TLIF is generally recommended for patients with chronic and debilitating lumbar spine conditions that have not improved with non-surgical interventions. The typical indications include:
- Degenerative Disc Disease: Breakdown of intervertebral discs causing pain and instability.
- Spondylolisthesis: One vertebra slipping forward relative to another, leading to nerve impingement or mechanical pain.
- Recurrent Disc Herniation: Repeat herniation after previous surgeries.
- Spinal Stenosis: Narrowing of the spinal canal causing nerve compression, resulting in pain, numbness, or weakness in the legs.
- Spinal Instability: Abnormal movement or alignment between vertebrae.
- Traumatic Injuries: Fractures or dislocations requiring stabilization.
- Infections or Tumors: Rare cases where stabilization is necessary after removal of infected or tumorous tissue.
The TLIF Surgical Technique
TLIF is typically performed under general anesthesia and can be conducted as an open surgery or using minimally invasive surgical (MIS) approaches. The procedure involves several critical steps:
1. Patient Positioning and Incision
The patient is placed under anesthesia and positioned face-down (prone) on the operating table. The surgeon makes a small incision in the lower back, usually on one side of the spine, to access the affected vertebral segment.
2. Exposure of the Spine
Muscles and soft tissues are carefully retracted to reveal the vertebrae and the affected intervertebral disc. In minimally invasive TLIF, tubular retractors and specialized instruments reduce tissue damage and blood loss.
3. Removal of the Intervertebral Disc
The surgeon removes part of the lamina (laminectomy or laminotomy) and occasionally the facet joint to gain access to the disc space. The herniated or degenerated disc material is carefully evacuated, providing more room for the nerves and preparing the space for fusion.
4. Preparation of the Disc Space
Once the disc is removed, the surgeon prepares the surfaces of the adjacent vertebrae to accept a bone graft. The disc space is distracted (gently separated) to restore normal disc height and alignment.
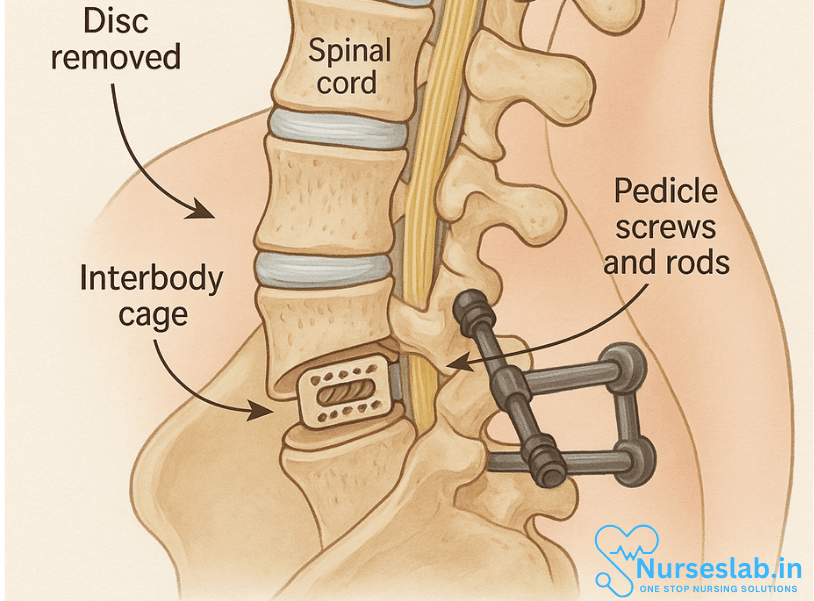
5. Placement of Bone Graft and Interbody Cage
A bone graft—often a combination of the patient’s own bone (autograft) and/or synthetic materials—is packed into the disc space. A special interbody cage (made of titanium, PEEK, or carbon fiber) is inserted to maintain space, support the graft, and promote fusion between the vertebral bodies.
6. Posterior Instrumentation
Pedicle screws and rods are placed through the vertebrae from the back of the spine. These hardware components provide immediate stability and compress the cage and bone graft, encouraging fusion as the patient heals.
7. Closure and Recovery
The surgical instruments are removed, and the incision is closed with sutures or staples. Sterile dressings are applied, and the patient is transferred to recovery.
Advantages of TLIF
The TLIF approach offers several advantages over other types of lumbar fusion:
- Reduced Nerve Retraction: Accessing the disc space from the side minimizes manipulation of the nerve roots and spinal cord, lowering the risk of nerve damage.
- Single-sided Approach: Only one side of the spine is disturbed, causing less muscle and tissue trauma.
- Stability: The use of an interbody cage and posterior instrumentation provides strong mechanical support.
- Minimally Invasive Options: MIS TLIF procedures can shorten hospital stays, reduce blood loss, and speed up recovery times.
Risks and Complications
Like all surgeries, TLIF carries inherent risks. Complications are relatively uncommon but can include:
- Infection: At the surgical site or deeper within the spine.
- Nerve Injury: Damage to nerve roots can result in numbness, weakness, or pain.
- Nonunion (Pseudoarthrosis): Failure of the bone graft to fuse the vertebrae over time.
- Hardware Failure: Loosening or breakage of screws, rods, or cages.
- Bleeding: Significant blood loss during or after surgery.
- Adjacent Segment Disease: Increased stress on the spinal segments above or below the fusion may lead to degeneration.
Patient Selection and Preoperative Assessment
Not every patient with lower back pain or lumbar spine problems is a candidate for TLIF. Careful assessment by a spine specialist is vital. Factors considered include:
- Severity and duration of symptoms
- Response to previous treatments
- Imaging studies (MRI, CT, X-rays) to assess spinal instability or nerve compression
- Overall health and comorbidities (such as diabetes or osteoporosis)
A multidisciplinary approach—incorporating input from neurologists, pain specialists, physiotherapists, and surgeons—often yields the best outcome for the patient.
Postoperative Care and Rehabilitation
Recovery from TLIF varies depending on the patient’s age, health status, and the complexity of the surgery. Key aspects of postoperative care include:
- Pain Management: Initially, patients may require opioid or non-opioid pain medications, transitioning to over-the-counter medications as healing progresses.
- Early Mobilization: Patients are typically encouraged to sit, stand, and walk with assistance on the first day after surgery to reduce the risk of complications such as blood clots or pneumonia.
- Physical Therapy: A structured rehabilitation program is crucial to restore spine mobility, strength, and function. Therapy may begin in the hospital and continue for several months after discharge.
- Activity Modifications: Patients should avoid heavy lifting, bending, and twisting for the first few months. Gradual return to normal activities is planned based on healing and physician guidance.
- Follow-Up Imaging: X-rays or CT scans monitor bone fusion and hardware placement over time.
Expected Outcomes and Long-Term Prognosis
Studies suggest that the majority of patients undergoing TLIF experience significant improvements in pain, mobility, and quality of life. Fusion rates are generally high, often exceeding 90% in appropriate candidates. Nonetheless, some patients may have persistent symptoms, and a small percentage may require revision surgery.
Innovations and Future Directions
Advancements in surgical techniques, instrumentation, and biological materials continue to refine TLIF outcomes. Minimally invasive approaches are increasingly favored for their smaller incisions, reduced scarring, and shorter recovery periods. Research into bone graft substitutes and growth factors aims to enhance fusion rates and healing.
Robotics and navigation systems allow for greater precision in screw placement and cage positioning, reducing operative risk and improving safety. As technology advances, TLIF is expected to become even safer, more effective, and accessible to a broader range of patients.ies, TLIF complications may include a risk of infection and excessive blood loss. Other potential complications include nerve damage.
Nursing Care of Patient with TLIF (Transforaminal Lumbar Interbody Fusion)
This document explores the key elements of support systems, long-term rehabilitation, and the comprehensive nursing care necessary to optimize outcomes for TLIF patients.
Support Systems: Family and Caregiver Involvement
A strong foundation of support is essential for recovery following TLIF surgery. Patients often face limitations in mobility, pain, and the need for assistance in performing activities of daily living (ADLs) during the initial postoperative period.
- Family as Partners in Care: Involving family members or caregivers in the patient’s rehabilitation journey is crucial. They provide emotional reassurance, help manage the patient’s daily routine, and serve as observers for subtle changes in health status that may warrant medical attention.
- Caregiver Education: Nurses and allied health professionals should offer practical training to caregivers on safe mobility techniques, medication administration, wound care, and monitoring for complications such as infection or nerve impairment.
- Home Environment Modification: Assessing and adapting the home environment—installing grab bars, removing trip hazards, and arranging daily essentials within reach—enhances safety and independence, reducing the risk of falls or setbacks.
- Communication Channels: Establishing clear lines of communication between the healthcare team, patient, and family ensures that concerns are addressed promptly and instructions are understood, fostering a sense of empowerment and partnership in the healing process.
Long-Term Rehabilitation and Outcomes
A strategic, multidisciplinary approach to rehabilitation is pivotal in maximizing functional recovery, minimizing the risk of complications, and supporting the patient’s reintegration into daily life.
Physical Therapy
Physical therapy forms the cornerstone of post-TLIF rehabilitation. Its primary objectives are to restore strength, flexibility, balance, and endurance while teaching safe movement techniques to protect the healing spine.
- Individualized Exercise Programs: Therapists develop customized protocols that consider surgical level, patient age, comorbidities, and preoperative function. Early exercises focus on gentle range-of-motion and isometric strengthening, gradually progressing to more intensive resistance and aerobic activities.
- Spinal Mechanics and Posture: Education on proper body mechanics and postural alignment reduces undue stress on the spine. Patients learn how to stand, sit, lift, and transition between positions safely.
- Functional Mobility: Training includes stair negotiation, transfers, and ambulation, with or without assistive devices, promoting independence in ADLs and community participation.
- Ongoing Assessment: Periodic reassessment allows the therapy team to track progress, address setbacks, and adjust goals and interventions as needed to maintain motivation and ensure optimal outcomes.
Occupational Therapy
Occupational therapy complements physical therapy by targeting activities necessary for self-care, work, and leisure.
- ADL Adaptation: Occupational therapists recommend adaptive equipment—such as reachers, dressing sticks, and shower chairs—to facilitate independence in bathing, dressing, grooming, and meal preparation.
- Energy Conservation: Techniques to pace activities, plan rest breaks, and prioritize essential tasks help manage fatigue and prevent overexertion during the recovery phase.
- Return to Work or School: OT professionals collaborate with employers and educators to identify necessary accommodations, such as modified workstations, flexible schedules, and gradual re-entry plans, supporting a seamless transition back to productivity.
Psychological Support
TLIF surgery and chronic pain can exert a considerable psychological burden, manifesting as anxiety, depression, frustration, or fear of re-injury.
- Assessment and Early Intervention: Nurses and physicians should proactively assess psychosocial well-being, using validated screening tools and open dialogue to identify those at risk.
- Counseling and Support Groups: Referral to mental health services, pain management clinics, or support groups provides patients and families with strategies for coping, stress reduction, and social connection, reducing isolation and improving outlook.
- Holistic Wellness: Encouraging mindfulness, relaxation techniques, and engagement in meaningful activities supports emotional resilience and overall satisfaction with the rehabilitation process.
Lifestyle Modifications for Long-Term Spinal Health
Sustained lifestyle changes are vital to prevent recurrence, promote healing, and improve long-term outcomes.
- Weight Management: Maintaining a healthy body weight minimizes stress on the lumbar spine, decreasing the risk of adjacent segment degeneration or hardware failure.
- Smoking Cessation: Smoking impairs bone healing and increases the risk of postoperative complications. Structured cessation programs offer education, counseling, and pharmacologic support to promote abstinence.
- General Wellness: Emphasizing the importance of balanced nutrition, regular physical activity, adequate sleep, and routine health screenings fosters overall well-being and maximizes recovery potential.
Return to Work or School
Resuming vocational, educational, or social roles is a significant milestone in the recovery continuum.
- Collaborative Planning: The multidisciplinary team—including the patient, family, therapists, and employer—works together to determine when it is safe to return to work or school. The process may involve a graded return, job modifications, or temporary restrictions based on physical capacity and job demands.
- Patient Advocacy: Nurses play an important role in advocating for appropriate accommodations and ensuring that the patient’s rights and needs are met during the reintegration process.
- Ongoing Support: Continued monitoring and communication allow for timely adjustments to the plan based on patient response and evolving needs.
REFERENCES
- Lee N, Kim KN, Yi S, Ha Y, Shin DA, Yoon DH, Kim KS. Comparison of Outcomes of Anterior, Posterior, and Transforaminal Lumbar Interbody Fusion Surgery at a Single Lumbar Level with Degenerative Spinal Disease. https://pubmed.ncbi.nlm.nih.gov/28189865/ World Neurosurg. 2017 May; 101:216-226.
- Hammad, Ahmed, Wirries, André, Ardeshiri, Ardavan, Nikiforov, Olexandr, Geiger, Florian. Open versus minimally invasive TLIF: literature review and meta-analysis. (2019) Journal of Orthopaedic Surgery and Research. 14 (1): 1. doi:10.1186/s13018-019-1266-y
- Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. https://pubmed.ncbi.nlm.nih.gov/27683674/ J Spine Surg. 2015 Dec;1(1):2-18.
- Rutherford EE, Tarplett LJ, Davies EM, Harley JM, King LJ. Lumbar spine fusion and stabilization: hardware, techniques, and imaging appearances. (2007) Radiographics : a review publication of the Radiological Society of North America, Inc. 27 (6): 1737-49. doi:10.1148/rg.276065205
- Reid PC, Morr S, Kaiser MG. State of the union: a review of lumbar fusion indications and techniques for degenerative spine disease. https://pubmed.ncbi.nlm.nih.gov/31261133/. J Neurosurg Spine. 2019 Jul 1;31(1):1-14.
- Virk S, Qureshi S, Sandhu H. History of Spinal Fusion: Where We Came from and Where We Are Going. https://pubmed.ncbi.nlm.nih.gov/32523481/ HSS J. 2020;16(2):137-142.
- Buchholz AL, Quinn JC, Buell TJ, Yen CP, Haid RW, Shaffrey CI, Smith JS. TLIF: A Review of Techniques and Advances. Contemporary Neurosurgery. 2019 Feb 15;41(2):1-8.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





