Introduction
Transfemoral Carotid Artery Stenting (TFCAS) represents a significant innovation in the management of carotid artery disease, offering a minimally invasive alternative to traditional surgical procedures such as carotid endarterectomy (CEA). As the prevalence of atherosclerotic carotid artery disease rises with an aging population, the need for less invasive, yet equally effective, treatments has become increasingly apparent. TFCAS has evolved over the last three decades, underpinned by advances in endovascular technology, imaging, and perioperative care.
Anatomy and Pathophysiology
The carotid arteries, located on each side of the neck, are responsible for delivering oxygen-rich blood from the heart to the brain. Atherosclerosis can lead to the development of carotid artery stenosis, a condition in which plaque narrows the vessel lumen, increasing the risk of ischemic stroke due to embolization or reduced cerebral perfusion.
Pathogenesis
The core pathophysiological process involves:
- Lipid accumulation within the arterial wall
- Chronic inflammation
- Plaque formation and progression
- Potential plaque rupture and thromboembolism
Indications for TFCAS
TFCAS is primarily indicated for patients with clinically significant carotid artery stenosis, especially when traditional surgery is associated with higher risk. The main indications include:
- Symptomatic carotid artery stenosis of ≥50% as measured by angiography, or ≥70% as measured by non-invasive imaging (e.g., Doppler ultrasound, CT angiography)
- Asymptomatic carotid stenosis of ≥60%, particularly in patients at high surgical risk
- Restenosis after prior carotid endarterectomy
- Hostile neck anatomy (e.g., prior neck radiation, tracheostomy, high carotid bifurcation)
- Severe cardiac or pulmonary comorbidities increasing surgical risk
Patient selection should always be individualized, taking into account factors such as age, comorbidities, anatomical considerations, and patient preferences.
Contraindications
Not all patients are candidates for TFCAS. Contraindications include:
- Severe tortuosity of the aortic arch or carotid arteries that prevents safe catheter navigation
- Active intracranial hemorrhage
- Recent major stroke with significant residual neurological deficit
- Allergy to contrast agents or antiplatelet medications that cannot be managed
- Life expectancy less than one year due to other comorbid conditions
Pre-Procedure Evaluation
A thorough evaluation is critical before proceeding with TFCAS. This includes:
- Detailed medical and neurological history
- Physical examination with emphasis on cardiovascular and neurological systems
- Imaging studies (carotid duplex ultrasound, CT angiography, MR angiography, digital subtraction angiography)
- Assessment of aortic arch anatomy and femoral artery access
- Pre-procedural laboratory testing (renal function, coagulation profile, etc.)
- Initiation of dual antiplatelet therapy, typically aspirin and clopidogrel, at least several days prior to the procedure
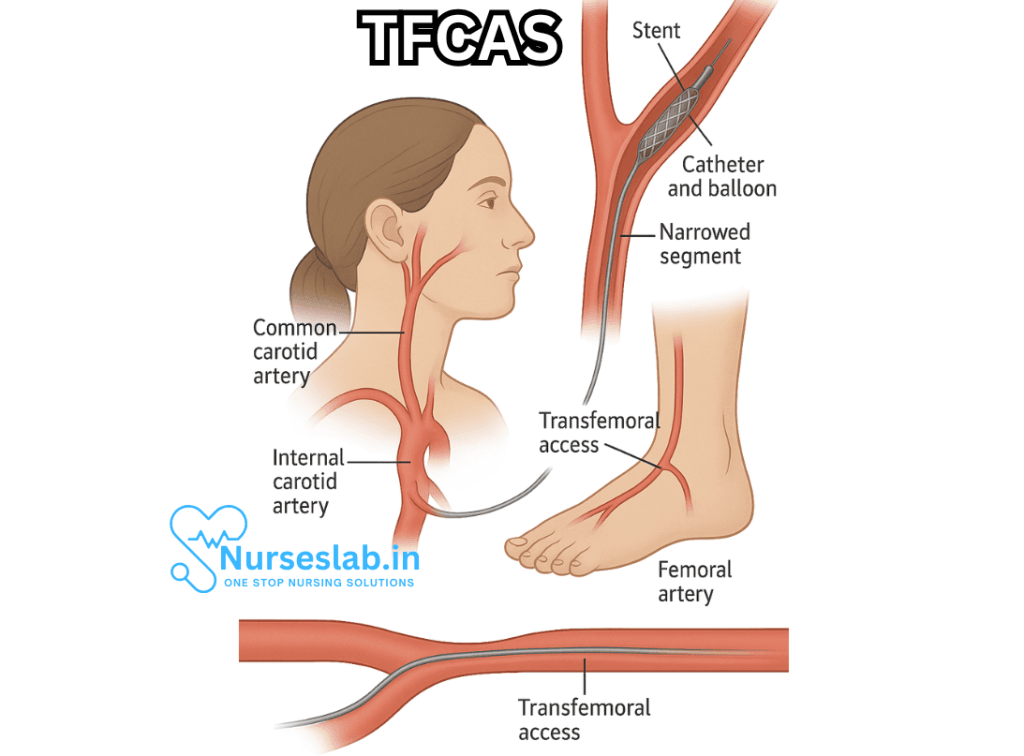
Technique of TFCAS
The transfemoral approach remains the most widely practiced method for carotid artery stenting. The key procedural steps are:
1. Patient Preparation
The patient is positioned supine and sedated (conscious sedation or general anesthesia, depending on clinical judgment). Standard monitoring is established, including blood pressure, ECG, and oxygen saturation. The groin area is prepped and draped for femoral artery access.
2. Vascular Access
A puncture is made in the common femoral artery, usually under ultrasound guidance, to minimize complications. A vascular sheath is introduced, through which guidewires and catheters will be advanced.
3. Navigation to the Carotid Artery
Using fluoroscopic guidance, a diagnostic catheter is advanced via the aorta into the common carotid artery. Digital subtraction angiography is performed to delineate the extent and nature of the stenosis.
4. Embolic Protection
To reduce the risk of periprocedural stroke caused by embolic debris, an embolic protection device (EPD) is deployed distal to the stenosis. EPDs can be distal filters or proximal occlusion devices, each with unique advantages and limitations.
5. Lesion Preparation
In some cases, pre-dilation of the stenosis with a small balloon may be performed to facilitate stent placement.
6. Stent Deployment
A self-expanding or balloon-expandable stent is carefully positioned across the stenotic segment under fluoroscopy and deployed. The stent scaffolds the vessel open, restoring blood flow.
7. Post-Dilation and Completion Angiography
Post-dilation with a balloon may be performed to optimize stent apposition and luminal gain. A final angiogram is obtained to confirm satisfactory result and exclude complications (e.g., dissection, residual stenosis).
8. Device Removal and Hemostasis
The embolic protection device is retrieved, and careful hemostasis is achieved at the femoral access site, often using a vascular closure device.
Post-Procedure Care
Following TFCAS, patients are monitored for several hours or overnight for complications. Key aspects of care include:
- Neurological status monitoring for signs of stroke or transient ischemic attack (TIA)
- Hemodynamic stability assessment
- Groin site evaluation for bleeding or hematoma
- Continuation of dual antiplatelet therapy, typically for at least 1-3 months, followed by lifelong single antiplatelet therapy
- Imaging follow-up (carotid duplex ultrasound) to assess stent patency and rule out restenosis
Risks and Complications
While TFCAS is less invasive than open surgery, it is not without risk. Potential complications include:
- Stroke or TIA (perioperative embolization is a major concern)
- Access site complications (hematoma, pseudoaneurysm, arterial dissection)
- Restenosis of the stented segment
- Allergic reaction to contrast agents
- Renal impairment due to contrast nephropathy
- Bradycardia or hypotension during stent deployment due to carotid sinus stimulation
- Rarely, vessel perforation or death
Outcomes and Efficacy
Multiple randomized controlled trials and registries have assessed the safety and efficacy of TFCAS as compared to carotid endarterectomy (CEA). Key findings include:
- TFCAS is associated with a slightly higher risk of minor perioperative stroke but a lower risk of myocardial infarction compared to CEA.
- Long-term stroke prevention rates are similar between TFCAS and CEA in appropriately selected patients.
- Technological advances, operator experience, and improved pre- and post-procedural care have contributed to better outcomes over time.
- TFCAS offers a valuable alternative for patients at elevated surgical risk or with anatomical considerations precluding open surgery.
Recent Advances and Future Directions
Ongoing research continues to refine and improve TFCAS. Areas of interest include:
- Development of next-generation embolic protection devices
- Emergence of alternative access routes, such as transcarotid artery revascularization (TCAR), which may offer lower stroke rates in certain populations
- Refinement in patient selection using advanced imaging and risk stratification tools
- Application of drug-eluting stents to reduce restenosis rates
As data matures and technology evolves, the role of TFCAS is expected to expand, particularly as part of a multidisciplinary, patient-centered approach to stroke prevention.
Nursing Care of Patients Undergoing Transfemoral Carotid Artery Stenting (TFCAS)
Nurses play a vital role in every stage of the stenting process, from patient education and preparation to monitoring for complications and facilitating recovery.
Pre-Procedural Nursing Care
Patient Assessment
- Medical History: Collect detailed history including symptoms of transient ischemic attacks (TIA), prior strokes, cardiovascular conditions, allergies, and medication use (especially anticoagulants and antiplatelet agents).
- Physical Examination: Assess neurological status, baseline vital signs, peripheral pulses, and evaluate for signs of carotid artery disease.
- Laboratory Investigations: Review recent blood work, including complete blood count, coagulation profile, renal function, and electrolytes.
Patient Education
- Explain the purpose, benefits, risks, and expected outcomes of TFCAS.
- Discuss perioperative instructions, including fasting guidelines and medication adjustments.
- Inform about the need for post-procedure monitoring and possible complications.
Preparation for Procedure
- Confirm that all necessary imaging (duplex ultrasonography, CT/MR angiography) is completed.
- Ensure consent is obtained and documented.
- Establish intravenous access for medication and fluids.
- Administer pre-procedure medications as prescribed (antiplatelet agents, sedatives, antibiotics if indicated).
- Prepare the groin area using aseptic technique for femoral artery access.
- Verify patient identification, allergies, and procedure details with the team.
Intra-Procedural Nursing Care
Patient Monitoring
- Monitor vital signs continuously (blood pressure, heart rate, respiratory rate, oxygen saturation).
- Assess neurological status via frequent checks for any new deficits or changes.
- Observe for signs of allergic reaction or adverse medication effects.
- Maintain aseptic technique throughout the procedure.
Assisting the Interventional Team
- Pass and manage sterile equipment and supplies as needed.
- Document procedural details, medications administered, and any intraoperative events.
- Communicate patient status and changes promptly to the proceduralist.
Managing Complications During Procedure
- Be vigilant for signs of hemodynamic instability, arrhythmias, or neurological changes.
- Prepare for emergency interventions, such as administration of reversal agents or code response.
- Monitor for access site bleeding, hematoma, or pseudoaneurysm formation.
Post-Procedural Nursing Care
Immediate Post-Procedure Monitoring
- Transfer the patient to a recovery area or intensive care setting.
- Monitor vital signs at frequent intervals (every 15 minutes initially, then as per protocol).
- Assess the groin access site for bleeding, swelling, or hematoma formation; apply pressure if indicated.
- Monitor neurological status closely for signs of stroke, TIA, or new deficits.
- Evaluate peripheral pulses and limb movement distal to the access site.
- Ensure bed rest for prescribed period to prevent complications at the femoral site.
Pain and Comfort Management
- Assess pain level and administer analgesics as prescribed.
- Support patient comfort through positioning and reassurance.
- Address anxiety and provide emotional support.
Medication Management
- Continue antiplatelet therapy as ordered to prevent stent thrombosis (commonly aspirin and clopidogrel).
- Monitor for adverse effects of medications, including bleeding or allergic reactions.
- Administer other prescribed medications, such as antihypertensives or statins.
Monitoring for Complications
- Neurological Complications: Watch for symptoms of stroke, TIA, confusion, or weakness. Conduct frequent neurological assessments using standardized scales (e.g., NIH Stroke Scale).
- Vascular Access Site Complications: Observe for bleeding, hematoma, infection, or limb ischemia at the femoral site.
- Cardiovascular Complications: Monitor for arrhythmias, blood pressure fluctuations, and chest pain. Have protocols in place for managing acute cardiac events.
- Allergic Reactions: Be alert for signs of contrast-induced reactions or allergic responses to medications and intervene promptly.
- Renal Complications: Monitor urine output and renal function, especially in patients with pre-existing kidney disease due to contrast exposure.
Promoting Recovery and Rehabilitation
- Encourage gradual resumption of activities as tolerated, according to physician guidance.
- Promote early mobilization to prevent deep vein thrombosis, following bed rest protocol for femoral access.
- Educate patient and family on signs of post-procedural complications and when to seek help.
- Coordinate with physiotherapists and occupational therapists for rehabilitation as needed.
Patient Education and Discharge Planning
Discharge Instructions
- Provide clear guidance on medication regimen, including the importance of adherence to antiplatelet therapy.
- Instruct on care of the access site, including recognition of bleeding, swelling, or infection.
- Advise on activity restrictions, such as avoiding heavy lifting or strenuous exercise until cleared by the healthcare provider.
- Discuss the need for follow-up appointments for clinical review and imaging to assess stent patency.
- Educate about lifestyle modifications to reduce cardiovascular risk: healthy diet, smoking cessation, regular exercise, and blood pressure control.
- Offer resources for psychological support and stroke prevention programs.
Emergency Symptoms to Report
- Sudden weakness, numbness, or difficulty speaking
- Severe headache or loss of consciousness
- Chest pain or palpitations
- Bleeding or swelling at the groin access site
- Fever, redness, or discharge from the access site
- Decreased urine output or signs of kidney dysfunction
Interdisciplinary Collaboration
Optimal outcomes for patients undergoing TFCAS depend on close collaboration among nurses, physicians, interventional radiologists, pharmacists, physiotherapists, and other members of the healthcare team. Nurses serve as advocates for patient safety, ensure effective communication, and facilitate smooth transitions of care.
REFERENCES
- Chang H, Rockman CB, Veith FJ, et al. Outcomes of transfemoral carotid artery stenting and transcarotid artery revascularization for restenosis after prior ipsilateral carotid endarterectomy. https://pubmed.ncbi.nlm.nih.gov/34506900/. J Vasc Surg. 2022 Feb;75(2):561-571.
- Liang P, Soden P, Wyers MC, et al. The role of transfemoral carotid artery stenting with proximal balloon occlusion embolic protection in the contemporary endovascular management of carotid artery stenosis. https://pubmed.ncbi.nlm.nih.gov/32251772/. J Vasc Surg. 2020 Nov;72(5):1701-1710.
- Rodriguez-Calienes A, Chavez-Ecos F, Espinosa-Martinez D, et al. Transradial Access Versus Transfemoral Approach for Carotid Artery Stenting: A Systematic Review and Meta‐Analysis. https://www.ahajournals.org/doi/10.1161/SVIN.123.001156. Stroke: Vascular and Interventional Neurology. 2023 Dec 27;4(2).
- Saleem T, Baril DT. Carotid Artery Stenting. https://www.ncbi.nlm.nih.gov/books/NBK470541/. 2023 Jul 24. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan.
- Stonko DP, Goldsborough E, Kibrik P, et al. Use of Transcarotid Artery Revascularization, Transfemoral Carotid Artery Stenting, and Carotid Endarterectomy in the US From 2015 to 2019 . https://pmc.ncbi.nlm.nih.gov/articles/PMC9482062/. JAMA Network Open. 2022 Sep 16;5(9);e2231944.
- Saleem T, Baril DT. Carotid Artery Stenting. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/sites/books/NBK470541/
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





