Introduction
Vertebroplasty is a minimally invasive medical procedure designed to treat painful vertebral compression fractures (VCFs) in the spinal column. Since its introduction in the 1980s, vertebroplasty has gained popularity as a method for providing rapid pain relief, stabilizing fractured vertebrae, and improving quality of life for patients suffering from conditions such as osteoporosis, metastatic cancer, and traumatic injury.
Historical Background
Vertebroplasty was first performed in 1984 in France by Dr. Hervé Deramond on a patient with a malignant vertebral hemangioma. The technique rapidly gained traction due to its effectiveness and minimally invasive nature. In the decades since, it has been refined and adopted worldwide, with numerous studies examining its efficacy and safety. The development of vertebroplasty paved the way for related procedures, such as kyphoplasty, which further expanded treatment options for vertebral compression fractures.
Anatomy and Pathophysiology
The human spinal column consists of 33 vertebrae, with each vertebra separated by intervertebral discs. Vertebral compression fractures occur when a vertebral body collapses or compresses, typically due to weakened bone from conditions such as osteoporosis, metastatic lesions, or trauma. These fractures can result in severe pain, reduced mobility, deformity, and in some cases, neurological compromise. The most commonly affected regions are the thoracic and lumbar spine.
Indications
Vertebroplasty is most commonly indicated for:
- Osteoporotic Vertebral Compression Fractures: Patients with painful, acute or subacute VCFs that do not respond to conservative management such as bed rest, bracing, or analgesics.
- Malignant Vertebral Lesions: Vertebral fractures resulting from primary or metastatic tumors, particularly when associated with intractable pain or spinal instability.
- Vertebral Hemangiomas: Symptomatic benign vascular tumors of the spine, when they cause pain or risk of collapse.
- Traumatic Fractures: Select cases where traditional surgical intervention is not feasible or is contraindicated due to patient comorbidities.
Proper patient selection is critical. Vertebroplasty is generally reserved for individuals who have persistent, localized vertebral pain correlating with imaging evidence of a compression fracture.
Contraindications
Absolute contraindications include:
- Asymptomatic vertebral fractures
- Active systemic or local infection
- Uncorrectable coagulopathy
- Allergy to bone cement or its components
Relative contraindications may include fractures causing significant spinal canal compromise with neurological deficits, or patients with extremely poor general health unable to tolerate the procedure.
The Vertebroplasty Procedure
Pre-procedure Evaluation
Prior to vertebroplasty, patients undergo thorough clinical and imaging evaluation. Magnetic Resonance Imaging (MRI) is the gold standard for identifying acute fractures, edema, and ruling out other causes of pain. A comprehensive medical history and assessment of comorbidities is essential.
Technique
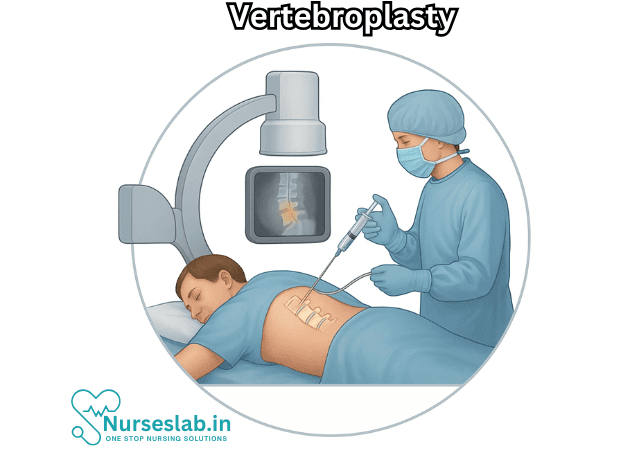
Vertebroplasty is typically performed in an interventional radiology suite or operating room under sterile conditions. The procedure involves the following steps:
- Patient Positioning: The patient lies prone (face-down) on the procedure table.
- Anesthesia: Local anesthesia and conscious sedation are common; general anesthesia is rarely required.
- Imaging Guidance: Real-time fluoroscopy or CT guidance is used to visualize the vertebral body and guide needle placement.
- Needle Insertion: A specialized needle (trocar) is introduced through the pedicle or lateral vertebral body into the affected vertebra.
- Cement Injection: Polymethylmethacrylate (PMMA) bone cement is prepared and injected into the vertebral body. The cement hardens within minutes, stabilizing the fracture.
- Post-procedure Monitoring: Patients are observed for several hours and typically discharged the same day or after overnight observation.
Benefits of Vertebroplasty
- Pain Relief: Many patients experience significant or complete pain relief within 24 to 48 hours after the procedure.
- Improved Function and Mobility: By stabilizing the fractured vertebra, vertebroplasty can restore mobility and allow a quicker return to daily activities.
- Minimally Invasive: The procedure is performed through a small skin incision, minimizing tissue damage, blood loss, and recovery time compared to open surgery.
Risks and Complications
Although vertebroplasty is generally safe, potential risks and complications include:
- Cement Leakage: PMMA may extravasate into surrounding tissues, veins, or the spinal canal, potentially causing nerve or spinal cord compression.
- Infection: Risk of discitis, osteomyelitis, or epidural abscess.
- Bleeding or Hematoma Formation
- Allergic Reaction: Rare hypersensitivity to cement components.
- New Adjacent Fractures: Some studies suggest an increased risk of fractures in vertebrae adjacent to the treated level, possibly due to altered biomechanics.
Complication rates are generally low when the procedure is performed by experienced practitioners with appropriate patient selection.
Evidence and Controversies
Several randomized controlled trials and meta-analyses have evaluated the effectiveness of vertebroplasty. Early observational studies suggested dramatic improvements in pain and function. However, two pivotal sham-controlled trials published in 2009 questioned whether vertebroplasty was superior to placebo. These studies found no significant difference in outcomes between vertebroplasty and sham procedures in some patients with osteoporotic VCFs.
Subsequent research, however, has indicated that selected patients—particularly those with acute, severe pain and clear imaging evidence of recent fracture—may benefit significantly from vertebroplasty. The optimal timing and patient selection remain subjects of ongoing debate.
Vertebroplasty vs. Kyphoplasty
Kyphoplasty is a related minimally invasive procedure that involves the insertion of a balloon into the collapsed vertebra to create a cavity and restore height before injecting cement. Kyphoplasty may be preferred in cases with severe vertebral height loss or spinal deformity, though both procedures share similar indications and outcomes.
Recovery and Prognosis
Most patients can resume light activities within 24 hours after vertebroplasty. Pain relief is often rapid and sustained, although ongoing management of underlying osteoporosis or malignancy is critical to prevent future fractures. Long-term outcomes depend on the underlying cause of fracture, patient health, and adherence to preventive care.
Nursing Care of Patients Undergoing Vertebroplasty
The procedure involves the percutaneous injection of bone cement (usually polymethyl methacrylate, PMMA) into the fractured vertebral body, offering rapid pain relief and improved functional mobility. Nursing care for patients undergoing vertebroplasty is crucial for ensuring optimal outcomes, preventing complications, and promoting recovery.
Pre-procedural Nursing Care
Before vertebroplasty, nurses play a vital role in patient preparation, education, and safety.
Patient Assessment
- Medical History: Assess for underlying conditions such as osteoporosis, malignancy, or coagulopathy. Review current medications, especially anticoagulants and antiplatelets, which may need to be withheld.
- Physical Examination: Evaluate the extent of pain, neurological deficits, and mobility limitations. Note any signs of infection or concurrent illness.
- Imaging: Confirm recent X-rays, CT, or MRI to identify the vertebral level(s) and the nature of the fracture.
Patient Education
- Procedure Explanation: Inform the patient and family about the vertebroplasty technique, its benefits, limitations, potential risks, and alternatives.
- Preoperative Instructions: Advise the patient regarding fasting requirements, medication adjustments, and what to expect on the day of the procedure.
Preparation
- Consent: Ensure informed consent has been obtained and documented.
- Laboratory Investigations: Check baseline blood counts, coagulation profile, renal function, and other necessary labs.
- IV Access: Establish intravenous access for medications and fluids.
- Pre-medication: Administer analgesics, sedatives, or prophylactic antibiotics as ordered.
- Skin Preparation: Prepare the skin over the procedure site, maintaining strict aseptic techniques.
Intra-procedural Nursing Care
During vertebroplasty, nurses support the patient and assist the medical team to maintain safety and comfort.
Patient Positioning
- Position: The patient is typically placed in the prone position. Ensure proper alignment and padding to prevent pressure injuries and discomfort.
Monitoring
- Vital Signs: Continuously monitor blood pressure, heart rate, respiratory rate, oxygen saturation, and pain level.
- Consciousness: Observe the patient’s response to sedation or analgesia, monitoring for over-sedation or adverse reactions.
Assisting with Procedure
- Maintain sterile field and provide necessary instruments to the physician.
- Monitor for any signs of distress, allergic reaction, or procedural complications, such as sudden pain or changes in vital signs.
Post-procedural Nursing Care
The period following vertebroplasty is critical for early detection of complications, pain management, and rehabilitation.
Immediate Post-procedure Care
- Recovery Monitoring: Transfer the patient to the recovery area and monitor vital signs every 15 minutes for the first hour, then at regular intervals as per protocol.
- Neurovascular Assessment: Assess for new neurological deficits, such as numbness, weakness, or loss of bladder/bowel control, which may indicate nerve injury or cement leakage.
- Pain Assessment: Evaluate pain levels regularly. Most patients experience significant reduction in pain, but persistent or worsening pain may signal complications.
- Site Inspection: Observe the puncture site for signs of bleeding, hematoma, swelling, or infection.
- Mobilization: Encourage early mobilization as tolerated, usually within hours of the procedure. Assist the patient with gentle movements and transfers to prevent falls or injury.
Pain Management
- Administer analgesics as needed, adjusting based on the patient’s pain level and response.
- Use non-pharmacological measures such as repositioning, relaxation techniques, or cold packs if appropriate.
Complication Surveillance
- Infection: Monitor for fever, chills, increased pain, redness, or discharge at the procedure site.
- Cement Leakage: Watch for signs of spinal cord compression, radiculopathy, or pulmonary embolism, which may arise from cement migration.
- Bleeding: Inspect site for hematoma and monitor hemoglobin and hematocrit if clinically indicated.
- Allergic Reaction: Be vigilant for symptoms such as rash, itching, or anaphylaxis.
Patient Education and Discharge Planning
- Activity: Instruct the patient on restrictions and safe movements post-procedure. Avoid heavy lifting, strenuous activity, or high-impact sports until cleared by the physician.
- Wound Care: Teach proper site care, signs of infection, and when to seek medical help.
- Follow-up: Schedule outpatient visits for clinical evaluation, imaging, and rehabilitation as needed.
- Medications: Review prescribed medications, including pain relievers, anticoagulants, or supplements for bone health.
Rehabilitation and Long-term Care
- Refer to physiotherapy for guided exercises to improve mobility, strength, and balance.
- Assess for fall risk and provide preventive measures, such as home modifications and assistive devices.
- Encourage a balanced diet rich in calcium and vitamin D, and advocate for ongoing management of osteoporosis or bone disease.
Special Considerations in Nursing Care
Older Adults
- Geriatric patients often require additional attention to mobility, skin integrity, and cognitive status. Adjust care plans to address comorbidities and frailty.
Patients with Malignancy
- Coordinate care with oncology, monitor for disease progression, and address unique palliative care needs.
Psychosocial Support
- Provide emotional support to alleviate anxiety related to the procedure and recovery. Involve family members and caregivers in education and planning.
- Assess for depression or social isolation, especially in those with limited mobility or chronic pain.
Documentation
- Record all assessments, interventions, education, and patient responses in detail.
- Monitor and note progress toward recovery goals, complications, and communication with the healthcare team.
REFERENCES
- Boss S, Srivastava V, Anitescu M. Vertebroplasty and Kyphoplasty. https://pubmed.ncbi.nlm.nih.gov/35526978/. Phys Med Rehabil Clin N Am. 2022 May; 33(2), 425–453.
- Browner BD, et al. Osteoporotic spinal fractures. In: Skeletal Trauma: Basic Science, Management, and Reconstruction. 6th ed. Elsevier; 2020. https://www.clinicalkey.com.
- Laratta JL, Shillingford JN, Lombardi JM, et al. Utilization of Vertebroplasty and Kyphoplasty Procedures Throughout The United States Over A Recent Decade: An Analysis of The Nationwide Inpatient Sample. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5637187/. J Spine Surg, 2017 Sep; 3(3), 364–370.
- Margetis K, Patel A, Petrone B, et al. Percutaneous Vertebroplasty and Kyphoplasty. [Updated 2025 Apr 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525963/
- Patel A, Petrone B, Carter KR. Percutaneous Vertebroplasty and Kyphoplasty. https://www.ncbi.nlm.nih.gov/books/NBK525963/. 2023 May 30. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
- Radiological Society of North America, Inc. Vertebroplasty & Kyphoplasty. https://www.radiologyinfo.org/en/info/vertebro. Last reviewed 5/1/2023.
- Society of Interventional Radiology. Vertebral Compression Fractures. https://www.sirweb.org/patient-center/conditions-and-treatments/vertebral-compression-fractures/.
- Cerny J, Soukup J, Petrosian K, Loukotova L, Novotny T. Efficacy and complication rates of percutaneous vertebroplasty and kyphoplasty in the treatment of vertebral compression fractures: a retrospective analysis of 280 patients. JCM. 2024;13(5):1495. doi:10.3390/jcm13051495
- Wang Q,Liu J, Ji Q, et al. Percutaneous vertebroplasty versus percutaneous kyphoplasty in elderly patients with osteoporotic vertebral compression fractures: prospective controlled study. BJS Open. 2024;8(1):zrad162. doi:10.1093/bjsopen/zrad162
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





