Introduction
The Whipple procedure, medically known as pancreaticoduodenectomy, is a complex and highly specialized surgical operation. It remains one of the most challenging yet lifesaving procedures in the realm of abdominal surgery. Primarily performed to treat cancers and other serious conditions of the pancreas, duodenum, and surrounding structures, the Whipple procedure is named after Dr. Allen Oldfather Whipple, the American surgeon who refined and popularized it in the 1930s.
This document aims to offer a thorough understanding of the Whipple procedure, including its historical origins, indications, surgical steps, risks, benefits, and postoperative considerations.
Historical Background
The first successful Whipple procedure was performed by Dr. Whipple in 1935. Over the decades, advances in surgical techniques, anesthesia, and postoperative care have significantly improved patient outcomes. Despite its complexity, the operation is now regularly performed in major medical centers globally, mainly as a treatment modality for pancreatic and periampullary cancers.
Anatomy
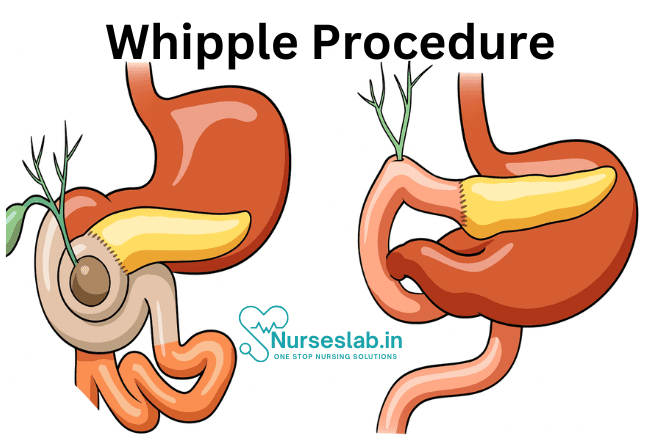
The Whipple procedure involves the surgical removal of several interconnected structures within the upper abdomen. These include:
- The head of the pancreas
- The duodenum (first part of the small intestine)
- A portion of the bile duct
- The gallbladder
- Sometimes, a portion of the stomach (pylorus)
The remaining pancreas, bile duct, and stomach (if preserved) are then reconnected to the small intestine to allow for normal digestion.
Indications for the Whipple Procedure
The most common indication for the Whipple procedure is pancreatic cancer, specifically tumors located in the head of the pancreas. Other conditions that may require this surgery include:
- Ampullary carcinoma
- Cholangiocarcinoma (cancer of the bile duct)
- Duodenal cancer
- Neuroendocrine tumors of the pancreas
- Chronic pancreatitis (in select cases)
- Benign tumors or cysts obstructing the bile duct or duodenum
Types of Whipple Procedures
There are two main variations of the Whipple procedure:
- Classic Whipple (Conventional): Involves the removal of the lower part of the stomach (antrectomy).
- Pylorus-Preserving Whipple: The pylorus (the valve controlling food passage from the stomach to the intestine) is left intact.
The choice between these depends on the tumor location, size, and the need to achieve clear surgical margins.
Preoperative Preparation
Patients considered for a Whipple procedure undergo comprehensive evaluation, including:
- Detailed imaging (CT scan, MRI, or endoscopic ultrasound) to assess tumor size, location, and spread
- Blood tests to check organ function and overall health
- Nutritional assessments, as many patients are malnourished due to their illness
- Consultations with anesthesiologists, oncologists, and sometimes nutritionists or gastroenterologists
Preparation may involve treatments such as stenting of the bile duct if jaundice is present, as well as optimization of blood sugar and nutritional status.
Surgical Procedure: Step-by-Step
The Whipple procedure typically lasts 4 to 8 hours and is performed under general anesthesia. The operation involves several critical steps:
- Open or minimally invasive incision to access the pancreas and surrounding structures
- Assessment for spread of cancer; if found to be widespread, the operation may be aborted
- Resection (removal) of the head of the pancreas, duodenum, gallbladder, and part of the bile duct, with or without a portion of the stomach
- Careful preservation of blood vessels supplying the liver and remaining intestine
- Reconstruction, which involves connecting (anastomosing) the remaining pancreas, bile duct, and stomach or duodenum to the small intestine (jejunal limb)
- Insertion of drains to prevent fluid accumulation
Attention to meticulous surgical technique is crucial to reduce the risk of complications.
Postoperative Recovery
Recovery from a Whipple procedure is gradual and can be challenging. Key aspects include:
- Initial hospitalization of 1 to 2 weeks, often in an intensive care setting
- Management of pain, fluid/electrolyte balance, and prevention of infections
- Early mobilization and breathing exercises to reduce the risk of blood clots and pneumonia
- Slow reintroduction of oral intake, starting with clear liquids and advancing to solid foods
- Monitoring for complications such as leaks, bleeding, or delayed gastric emptying
- Nutritional support, as digestive enzyme supplementation may be required
Most patients need several weeks to months for full recovery.
Risks and Complications
The Whipple procedure is associated with significant risks, which are higher than for many other abdominal surgeries. These include:
- Infection (wound, intra-abdominal abscesses)
- Pancreatic fistula (leakage of pancreatic fluid)
- Delayed gastric emptying
- Bleeding
- Pulmonary complications (such as pneumonia)
- Blood clots (deep vein thrombosis or pulmonary embolism)
- Death (mortality rates in high-volume centers are generally below 5%)
Long-term, some patients experience weight loss, malabsorption, and require lifelong pancreatic enzyme replacement.
Prognosis and Outcomes
Outcomes following the Whipple procedure largely depend on the underlying disease, patient’s overall health, and the expertise of the surgical team. In the case of pancreatic cancer, the procedure offers the only potential for cure, especially when diagnosed early and the tumor is fully resectable.
Advancements in surgical technique, better perioperative care, and improved patient selection have enhanced survival rates and reduced complications. Five-year survival for pancreatic head cancer after Whipple ranges from 20-25% in select patients, although this remains a challenging disease.
Quality of Life After the Whipple Procedure
Although recovery can be arduous, many patients regain a good quality of life after the initial period of adjustment. Close follow-up with the medical team is crucial, as is attention to nutrition, management of diabetes (if it develops), and surveillance for cancer recurrence if the surgery was performed for malignancy.
Support from dietitians, physical therapists, and support groups can significantly aid in the rehabilitation process.
Recent Advances
There have been several developments aimed at improving outcomes for patients undergoing the Whipple procedure:
- Minimally Invasive Approaches: Laparoscopic and robotic-assisted Whipple procedures are being performed in select centers, offering reduced incision size and faster recovery for some patients.
- Enhanced Recovery Pathways: Protocols to optimize pain management, fluid balance, and early nutrition have been shown to speed recovery and decrease complications.
- Personalized Medicine: Advances in genetics and tumor biology are allowing for more tailored treatments alongside surgery, such as targeted therapies and immunotherapy.
Nursing Care of the Patient Undergoing Whipple Procedure
It involves the removal of the pancreatic head, duodenum, a portion of the bile duct, gallbladder, and sometimes part of the stomach. Owing to its complexity, nursing care for patients who undergo the Whipple procedure is critical for promoting recovery, preventing complications, and enhancing quality of life.
Preoperative Nursing Care
Before surgery, patients often experience anxiety and require comprehensive education and support.
Patient Education
- Explanation of the Procedure: Provide clear, jargon-free information about the surgical steps, possible outcomes, and expectations for recovery.
- Informed Consent: Confirm that the patient understands the risks, benefits, and alternatives, and that all questions are addressed.
- Preparation for Lifestyle Changes: Discuss potential changes in digestion, nutrition, and if relevant, the onset of diabetes.
Physical Preparation
- Nutritional Assessment: Optimise nutrition to support wound healing and recovery, potentially in collaboration with a dietitian.
- Laboratory Testing: Ensure baseline blood work, including complete blood count, electrolytes, coagulation profile, and blood glucose.
- Preoperative Fasting: Follow fasting guidelines to reduce aspiration risk during anaesthesia.
- Management of Comorbidities: Optimise control of hypertension, diabetes, or other chronic conditions.
- Physical Assessment: Document baseline respiratory, cardiovascular, and neurological status.
Psychological Support
- Emotional Support: Address fears and anxieties, provide reassurance, and refer to counselling or support groups as needed.
- Family Involvement: Encourage family participation in education and support activities.
Immediate Postoperative Nursing Care
After the Whipple procedure, patients are typically admitted to a high-dependency unit or intensive care for close monitoring.
Airway, Breathing, and Circulation
- Airway Management: Monitor airway patency, especially after extubation. Encourage deep breathing and coughing to prevent atelectasis and pneumonia.
- Respiratory Support: Use incentive spirometry and physiotherapy to maintain optimal lung function.
- Haemodynamic Monitoring: Regularly assess blood pressure, heart rate, and peripheral perfusion. Watch for signs of bleeding or shock.
Fluid and Electrolyte Balance
- Intravenous Fluids: Administer fluids as prescribed, and closely monitor input and output.
- Electrolyte Monitoring: Assess for disturbances, particularly in potassium, sodium, calcium, and magnesium.
- Early Detection of Dehydration: Observe for dry mucous membranes, decreased urine output, and postural hypotension.
Pain Management
- Pain Assessment: Use a validated pain scale to assess pain regularly.
- Analgesia: Administer analgesics via epidural, PCA pump, or IV opioids as prescribed, and monitor for side effects such as respiratory depression or constipation.
- Non-Pharmacological Methods: Encourage relaxation techniques, positioning, and cold/heat therapy as appropriate.
Wound Care
- Incision Monitoring: Examine the surgical site for signs of infection, dehiscence, or bleeding.
- Dressing Changes: Maintain a sterile environment during dressing changes and educate the patient about wound care.
- Drain Management: Monitor surgical drains for quantity, colour, and consistency of output. Document findings and report abnormalities promptly.
Gastrointestinal Care
- Nasogastric Tube: Maintain patency and monitor for output, which should decrease as bowel function resumes.
- Delayed Gastric Emptying: Watch for nausea, vomiting, abdominal distension, and adjust feeding regimens accordingly.
- Early Feeding: When appropriate, initiate enteral nutrition to support recovery, under dietary guidance.
Prevention of Complications
- Infection: Monitor for fever, tachycardia, and wound erythema. Employ aseptic techniques and encourage hand hygiene.
- Pancreatic Fistula: Observe for increased drain output, changes in the nature of drainage, or signs of peritonitis.
- Delayed Gastric Emptying: Assess for persistent nausea and vomiting; report to medical team for intervention.
- Deep Vein Thrombosis (DVT): Implement prophylactic measures such as compression stockings, early mobilisation, and anticoagulants as prescribed.
- Pulmonary Complications: Encourage mobilisation, use of incentive spirometry, and chest physiotherapy.
Ongoing Postoperative Nursing Care
Nutrition Support
- Diet Advancement: Follow a gradual progression from clear liquids to solid foods based on tolerance and return of bowel function.
- Supplementation: Administer pancreatic enzyme supplements if indicated to aid digestion.
- Blood Glucose Monitoring: Monitor for hyperglycaemia or hypoglycaemia, as some patients may develop diabetes post-surgery.
- Patient Education: Instruct on dietary modifications, need for frequent small meals, and the importance of high-protein, low-fat foods.
Mobility and Physical Rehabilitation
- Early Mobilisation: Encourage the patient to sit up and begin walking as soon as possible to reduce the risk of complications.
- Physiotherapy: Collaborate with physiotherapists to develop a tailored exercise plan that enhances strength and prevents deconditioning.
Psychosocial Support
- Emotional Wellbeing: Provide ongoing support to address anxiety, depression, or adjustment issues related to changes in body image or lifestyle.
- Support Groups: Encourage participation in patient support groups for those undergoing similar procedures.
- Family Involvement: Involve family members in care and education to foster a strong support system at home.
Education for Self-Management
- Wound and Drain Care: Teach proper techniques for care at home, signs of infection, and when to seek medical help.
- Signs of Complications: Educate on symptoms that require immediate attention, such as fever, sudden abdominal pain, jaundice, or excessive drainage.
- Medication Management: Instruct about the purpose, administration, and side effects of medications, including enzyme supplements, insulin, and pain relievers.
Long-term Follow-up Care
- Surveillance for Recurrence: Arrange regular follow-up visits with the surgical and oncology teams. Monitor for signs of cancer recurrence through imaging and laboratory tests if the surgery was cancer-related.
- Chronic Disease Management: Monitor for and manage late complications such as diabetes, malabsorption, or nutritional deficiencies.
- Health Maintenance: Encourage ongoing preventive care, age-appropriate screenings, and immunisations.
REFERENCES
- American Cancer Society. Surgery for Pancreatic Cancer. https://www.cancer.org/cancer/pancreatic-cancer/treating/surgery.html. Last revised 2/25/2024.
- Townsend CM Jr, et al. Exocrine pancreas. In: Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 21st ed. Elsevier; 2022. https://www.clinicalkey.com.
- Mantzavinou A, et al. Robotic versus open pancreaticoduodenectomy, comparing therapeutic indexes; a systematic review. International Journal of Surgery. 2022; doi:10.1016/j.ijsu.2022.106633.
- Simon R. Complications after pancreaticoduodenectomy. Surgical Clinics of North America. 2021; doi:10.1016/j.suc.2021.06.011.
- Cancer Patients Alliance. Pancreatic Cancer Surgery and Whipple Procedure. https://pancreatica.org/pancreatic-cancer/pancreatic-cancer-surgical-treatment/
- Cancer Patients Alliance. What is Pancreatic Cancer?https://pancreatica.org/pancreatic-cancer/pancreatic-cancer-surgical-treatment/.
- Hirshberg Foundation for Pancreatic Cancer Research. Surgery. https://pancreatic.org/pancreatic-cancer/treatment-options/surgery/
- National Cancer Institute: Division of Cancer Treatment & Diagnosis (U.S.). Pancreatic SPOREs. https://trp.cancer.gov/spores/pancreatic.htm. Last updated 9/21/23.
- Pancreatic Cancer Action Network. Whipple procedure. https://www.pancan.org/facing-pancreatic-cancer/treatment/treatment-types/surgery/whipple-procedure-pancreaticoduodenectomy/
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





