Kyphoplasty Procedure: A Comprehensive Overview
Introduction
Kyphoplasty is a minimally invasive surgical procedure aimed at treating painful vertebral compression fractures (VCFs) of the spine, most commonly caused by osteoporosis, trauma, or, less frequently, malignancy. The primary goals of kyphoplasty are to alleviate pain, restore vertebral body height, and stabilize the fracture, ultimately improving patient mobility and quality of life. Over the past two decades, kyphoplasty—alongside vertebroplasty—has revolutionized the management of osteoporotic spinal fractures, providing an effective alternative to prolonged conservative management and its associated limitations.
Background and Rationale
VCFs are a significant source of morbidity in older adults, particularly those with osteoporosis. Such fractures may result in debilitating pain, impaired mobility, progressive spinal deformity (kyphosis), and adverse effects on pulmonary function and overall quality of life. Traditional management includes bed rest, analgesics, bracing, and physical therapy. However, these approaches often provide incomplete relief and may lead to complications related to immobility, such as deep vein thrombosis, pneumonia, and muscle wasting.
Percutaneous vertebral augmentation techniques—namely vertebroplasty and kyphoplasty—were developed to address these concerns. While both techniques involve the injection of bone cement (usually polymethylmethacrylate, or PMMA) into the fractured vertebral body, kyphoplasty introduces the additional step of cavity creation and vertebral height restoration using a balloon tamp, thus potentially reducing kyphosis and spinal deformity.
Indications for Kyphoplasty
Kyphoplasty is indicated for patients with:
- Acute or subacute vertebral compression fractures, particularly those less than 3 months old, with persistent, localized back pain refractory to conservative therapy.
- Evidence of vertebral body collapse due to osteoporosis or, in selected cases, metastatic lesions and multiple myeloma.
- Significant decline in functional status, mobility, or quality of life due to the fracture.
Contraindications include asymptomatic fractures, fractures with significant retropulsion of bone fragments into the spinal canal causing neurological compromise, spinal infection, coagulopathy, and allergies to materials used during the procedure.
Preoperative Evaluation
Prior to kyphoplasty, a thorough assessment is essential. This includes a detailed history and physical examination focused on the onset, location, and characteristics of the pain. Imaging studies are critical in establishing the diagnosis and planning the procedure:
- Plain Radiographs: Used to visualize vertebral collapse and assess spinal alignment.
- Magnetic Resonance Imaging (MRI): Gold standard for confirming acute fractures, edema, and ruling out other causes of pain. MRI also helps differentiate between old and new fractures.
- Computed Tomography (CT): Useful for assessing fracture morphology and guiding procedural planning.
Laboratory work-up may include coagulation profile and infection markers if indicated.
Procedure Technique
Kyphoplasty is typically performed under local anesthesia with conscious sedation or, in select cases, general anesthesia. The steps are as follows:
1. Patient Positioning
The patient is placed in a prone position on a radiolucent operating table. Padding is applied to relieve abdominal pressure and maintain spinal alignment.
2. Image Guidance
Continuous fluoroscopic guidance is utilized throughout the procedure to ensure accurate needle placement and monitor cement injection.
3. Needle Insertion
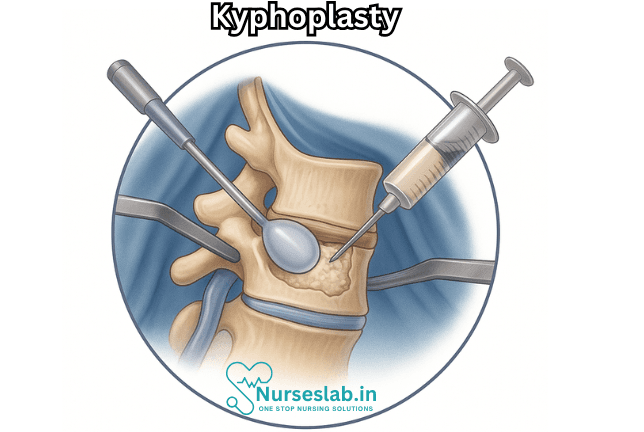
After sterile preparation and draping, a small skin incision is made over the affected vertebra. Under fluoroscopy, a trocar needle is advanced through the pedicle into the anterior third of the vertebral body.
4. Balloon Tam Inflation
A specialized balloon tamp is inserted through the needle into the vertebral body. The balloon is then slowly inflated, creating a cavity, compacting the spongy bone, and often partially restoring vertebral body height. This step may reduce spinal deformity and kyphosis caused by the fracture.
5. Cement Preparation and Injection
Once the cavity is created, the balloon is deflated and removed. The space is then filled with a viscous bone cement (PMMA), injected under careful fluoroscopic monitoring. Cement hardens rapidly, stabilizing the fracture and maintaining the restored height.
6. Completion and Recovery
The needle is withdrawn, and the small incision is closed with a sterile dressing. Patients are typically observed for a few hours post-procedure and may be discharged the same day or the following morning, depending on their clinical status.
Outcomes and Effectiveness
Numerous studies have demonstrated the benefits of kyphoplasty in appropriately selected patients:
- Pain Relief: Most patients report immediate and significant reduction in pain—often within hours to days of the procedure.
- Functional Improvement: Enhanced mobility and independence are commonly observed, facilitating faster return to daily activities.
- Vertebral Height Restoration: Kyphoplasty can partially restore lost vertebral height and decrease local kyphosis, though complete correction is uncommon.
- Quality of Life: Improvements in pain and function often translate into better overall quality of life scores.
Risks and Complications
Kyphoplasty is generally considered safe, with complication rates lower than many open surgical procedures. However, potential risks include:
- Cement Leakage: Extravasation of cement outside the vertebral body can occur but is usually asymptomatic. Rarely, it may cause nerve or spinal cord compression or pulmonary embolism.
- Infection: As with any invasive procedure, infection at the site or deep within the vertebra can occur.
- Bleeding: Uncommon but possible, particularly in patients with bleeding disorders.
- Increased Risk of Adjacent Fractures: Some evidence suggests that adjacent vertebrae may be at higher risk for future fractures due to altered biomechanics.
- Anesthetic Complications: Minimal, but present, especially in medically complex patients.
Postoperative Care and Rehabilitation
Following kyphoplasty, most patients experience rapid relief and can resume daily activities within days. Post-procedure recommendations may include:
- Short-term use of a brace, if needed, for comfort.
- Gradual return to activity as tolerated.
- Physical therapy to strengthen core and back muscles, improve posture, and prevent further fractures.
- Evaluation and management of underlying osteoporosis, including medication, nutrition, and fall prevention strategies.
Comparisons with Vertebroplasty
- While both kyphoplasty and vertebroplasty use bone cement to stabilize fractures, key differences include:
- Cost and Complexity: Kyphoplasty is generally more expensive and technically demanding than vertebroplasty.
- Balloon Inflation: Unique to kyphoplasty, aiming to restore vertebral height and reduce deformity.
- Cement Leakage: Kyphoplasty tends to have lower cement leakage rates due to cavity creation before cement injection.
Nursing Care of a Patient Undergoing Kyphoplasty Procedure
As with any surgical intervention, the role of nursing care is crucial in ensuring patient safety, promoting healing, and preventing complications. This document provides a comprehensive overview of the nursing care required for patients undergoing kyphoplasty.
Preoperative Nursing Care
Patient Assessment and Preparation
- Medical History Review: Conduct a thorough assessment of the patient’s medical, surgical, and medication history. Pay special attention to bleeding disorders, allergies (especially to contrast media or anesthetic agents), and chronic illnesses such as diabetes or cardiac disease.
- Physical Assessment: Evaluate baseline neurological status, including motor strength, sensation, and reflexes in the lower extremities. Assess pain level using standardized pain scales and document findings for post-procedure comparison.
- Laboratory and Diagnostic Review: Ensure recent blood work, particularly coagulation profiles and renal function tests, are available and within acceptable ranges. Confirm diagnostic imaging (MRI, CT, X-rays) correlates with the clinical diagnosis.
- Patient Education: Explain the kyphoplasty procedure, including the rationale, steps involved, expected outcomes, and potential risks or complications. Discuss postoperative expectations such as activity restrictions, pain management, and wound care. Encourage questions to alleviate anxiety.
- Fasting and Medication Instructions: Instruct the patient to fast for the recommended period prior to the procedure, usually 6–8 hours. Review and clarify which medications should be held or continued, particularly anticoagulants and antiplatelet agents.
- Informed Consent: Ensure the patient (or legal representative) has signed the informed consent form after all questions have been addressed by the healthcare provider.
Preparation for Procedure
- IV Access: Establish and secure reliable intravenous access for administration of sedation, fluids, and emergency medications if needed.
- Preoperative Checklist: Complete a surgical safety checklist, confirming patient identification, procedure site, allergies, and other safety protocols.
- Psychological Support: Provide reassurance and support to alleviate anxiety. Offer comfort measures such as a warm blanket and a calm environment.
Intraoperative Nursing Care
- Monitoring: Continuously monitor the patient’s vital signs, oxygen saturation, cardiac rhythm, and level of consciousness. Document baseline and intraoperative changes.
- Assisting the Physician: Assist with patient positioning, usually in prone or lateral decubitus position, ensuring comfort, safety, and protection of pressure points. Maintain a sterile field and assist with equipment as needed.
- Medication Administration: Administer prescribed sedation, analgesics, or antibiotics as directed by the anesthesiologist or physician.
- Communication: Serve as a liaison between the surgical team and the patient’s family, providing updates on progress as appropriate.
Postoperative Nursing Care
Immediate Postoperative Phase
- Vital Signs Monitoring: Monitor vital signs (blood pressure, pulse, respiration, and temperature) at regular intervals according to institutional protocol. Watch for signs of hypotension, bradycardia, or respiratory depression, which may indicate complications from sedation or blood loss.
- Neurological Assessment: Perform frequent neurological checks to detect any changes in motor or sensory function, especially in the lower extremities. Promptly report any deterioration to the physician.
- Pain Management: Assess pain using a standardized scale. Administer prescribed analgesics and evaluate the effectiveness. Encourage the use of non-pharmacological pain management techniques such as relaxation or distraction.
- Wound Care: Inspect the puncture site for bleeding, swelling, drainage, or signs of infection. Keep the area clean and covered with a sterile dressing. Reinforce dressing as needed and document observations.
- Mobility and Activity: Advise bed rest for a few hours postprocedure, as directed by the physician. Encourage gradual resumption of activity, starting with gentle movements and progressing to sitting and walking as tolerated. Implement fall prevention strategies and assist with mobility as needed.
- Hydration and Nutrition: Once fully awake, encourage oral fluids unless contraindicated. Resume diet as tolerated, monitoring for nausea or vomiting.
- Monitoring for Complications:
- Bleeding or Hematoma: Observe for excessive bleeding at the puncture site or development of a hematoma.
- Cement Leakage: Watch for new or worsening neurological symptoms, sudden severe back pain, or signs of pulmonary embolism, which could indicate leakage of bone cement.
- Infection: Monitor for fever, increased pain, redness, swelling, or drainage at the site.
- Allergic Reactions: Be alert for signs of allergic reaction (rash, pruritis, difficulty breathing) due to contrast agents or medications.
Ongoing Postoperative Care
- Patient Education: Instruct the patient on signs of complications requiring immediate medical attention, such as sudden onset of leg weakness, loss of bowel or bladder control, severe headache, or difficulty breathing.
- Activity Recommendations: Advise on gradual resumption of activities, avoiding heavy lifting, strenuous exercise, or twisting motions until cleared by the physician. Reinforce proper body mechanics and provide information about assistive devices if needed.
- Pain and Medication Management: Educate about the correct use of prescribed analgesics, possible side effects, and the importance of adhering to the medication schedule. Discuss alternative strategies for pain relief, including physical therapy, heat/cold therapy, and gentle exercises as recommended.
- Follow-Up Appointments: Stress the importance of attending scheduled follow-up visits for assessment of vertebral healing and evaluation of pain control.
- Support Systems: Encourage the involvement of family members or caregivers in the recovery process. Provide information about community resources and support groups for osteoporosis or spinal health, if appropriate.
Potential Complications and Their Management
Complications
- Cement Extravasation: Leakage of bone cement during the procedure can cause nerve compression or embolism. Nurses should be vigilant for sudden neurological changes or respiratory symptoms and notify the physician immediately.
- Infection: Although rare, infection at the puncture site or vertebral body is possible. Proper aseptic technique and wound care are essential. Any signs of infection require prompt evaluation and intervention.
- Bleeding: Monitor for excessive bleeding postprocedure, particularly in patients with coagulopathies or on anticoagulants. Apply pressure dressings as appropriate and notify the healthcare provider of significant findings.
- Allergic Reaction: Reactions to contrast media or medications should be promptly recognized and treated with appropriate interventions, such as antihistamines or epinephrine as prescribed.
- Adjacent Vertebral Fractures: The altered biomechanics of the spine after kyphoplasty may predispose adjacent vertebrae to fracture. Educate the patient on bone health maintenance and the importance of osteoporosis management.
Management Strategies
- Immediate reporting of abnormal findings to the healthcare team.
- Provision of emotional support to the patient and family.
- Coordination with interdisciplinary teams, including pain management specialists, physical therapists, and case managers.
Documentation
Accurate and thorough documentation is a cornerstone of effective nursing care. Essential elements to document include:
- Preoperative teaching and patient understanding
- Intraoperative observations and interventions
- Postoperative vital signs, neurological status, pain assessments, and wound care findings
- Patient’s response to analgesics and other medications
- Education provided regarding activity, medication, wound care, and signs of complications
- Communication with other healthcare professionals and family members
Discharge Planning and Patient Education
Discharge planning should begin early in the postoperative period and include:
- Clear instructions on wound care, signs of infection, and when to seek medical attention
- Guidance regarding activity modification and gradual return to daily activities
- Information about prescribed medications, including dosage, timing, and potential side effects
- Resources for physical therapy or rehabilitation if necessary
- Contact information for follow-up appointments and emergency care
REFERENCES
- Boss S, Srivastava V, Anitescu M. Vertebroplasty and Kyphoplasty., https://pubmed.ncbi.nlm.nih.gov/35526978/. Phys Med Rehabil Clin N Am. 2022 May; 33(2):425–453.
- Cite this Page
- Margetis K, Patel A, Petrone B, et al. Percutaneous Vertebroplasty and Kyphoplasty. [Updated 2025 Apr 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525963/
- Laratta JL, Shillingford JN, Lombardi JM, et al. Utilization of Vertebroplasty and Kyphoplasty Procedures Throughout The United States Over A Recent Decade: An Analysis of The Nationwide Inpatient Sample., https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5637187/. J Spine Surg. 2017 Sep; 3(3):364–370.
- Patel A, Petrone B, Carter KR. Percutaneous Vertebroplasty and Kyphoplasty https://www.ncbi.nlm.nih.gov/books/NBK525963/. 2023 May 30. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan.
- Radiological Society of North America, Inc. Vertebroplasty & Kyphoplasty (https://www.radiologyinfo.org/en/info/vertebro). Last reviewed 5/1/2023.
- Society of Interventional Radiology. Vertebral Compression Fractures https://www.sirweb.org/patient-center/conditions-and-treatments/vertebral-compression-fractures/.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





