Liver transplantation stands as one of the greatest achievements in modern medicine—a remarkable feat of scientific ingenuity and compassionate care. It is a beacon of hope for individuals afflicted with end-stage liver disease, acute liver failure, and certain complex metabolic conditions. With the steady evolution of surgical technique, immunosuppressive therapy, and organ preservation, liver transplantation has not only extended life, but has also greatly improved its quality for countless patients across the globe.
The Liver: Function and Significance
The liver, the largest solid organ in the human body, performs an astounding array of functions. It is central to metabolism, processing nutrients from food, detoxifying harmful substances, producing vital proteins such as albumin, and generating bile for fat digestion. When the liver fails—due to chronic diseases like cirrhosis, viral hepatitis, autoimmune disorders, genetic metabolic diseases, or acute toxic injuries—the body is thrown into turmoil. Symptoms can range from jaundice and confusion to bleeding disorders and multi-organ failure.
Indications for Liver Transplantation
The decision to pursue liver transplantation is never taken lightly. It is reserved for patients whose liver function declines to the point that survival is threatened, and where no effective medical treatment exists. Common indications include:
- Chronic liver diseases: Cirrhosis due to hepatitis B or C, alcohol-related liver disease, non-alcoholic fatty liver disease, and autoimmune hepatitis.
- Acute liver failure: Rapid loss of liver function, often due to drug toxicity (such as acetaminophen overdose), viral hepatitis, or unknown causes.
- Inherited metabolic conditions: Disorders like Wilson’s disease, alpha-1 antitrypsin deficiency, and familial amyloidosis.
- Pediatric diseases: Biliary atresia and other congenital malformations.
Evaluation and Listing
Transplant centers utilize a comprehensive multidisciplinary approach to determine candidacy for transplantation. Patients undergo extensive assessment, including laboratory tests, imaging studies, cardiac and pulmonary evaluation, psychosocial screening, nutritional consults, and education on post-transplant care.
A key tool in prioritizing patients is the Model for End-Stage Liver Disease (MELD) score, which predicts the risk of death in liver disease and helps allocate organs fairly. The higher the MELD score, the greater the urgency for transplant.
The Gift of Organ Donation
The liver’s regenerative ability allows transplantation from both deceased and living donors. Deceased donation occurs when a person with healthy organs passes away, and their liver is donated, often split to serve more than one recipient. Living donor transplantation involves removing a segment of the liver from a healthy volunteer—often a relative or close friend. The donor’s liver regenerates, and both recipients recover with fully functioning organs.
Organ donation, whether living or deceased, is a profound act of generosity and altruism. Education, public awareness, and cultural sensitivity are vital in encouraging donation and addressing misconceptions.
Transplant Surgery: Science and Skill Intertwined
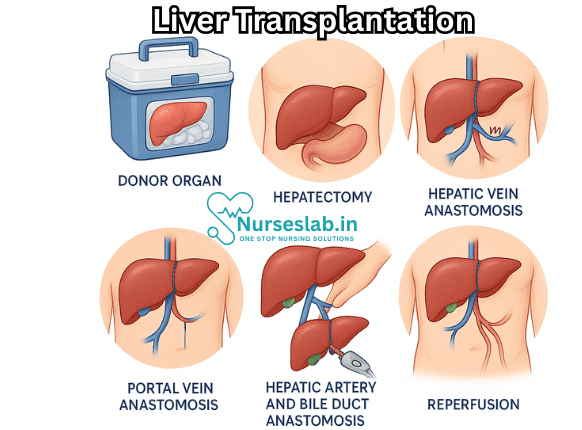
Liver transplantation is a complex, multi-stage operation. It involves removal of the diseased liver and meticulous implantation of the new organ. Key steps include:
- Recipient hepatectomy: The diseased liver is carefully dissected from the surrounding structures, including the blood vessels and bile ducts.
- Implantation: The donor liver is connected to the recipient’s major blood vessels and bile duct, restoring circulation and biliary drainage.
- Reperfusion: Blood flow is restored and the new liver begins to function, often immediately.
This intricate procedure demands skill, precision, and teamwork—a symphony orchestrated by surgeons, anesthesiologists, nurses, and transplant coordinators.
Immunosuppression: Balancing Rejection and Infection
After surgery, the recipient’s immune system may recognize the new liver as foreign and attack it—a process called rejection. To prevent this, patients must take immunosuppressive medications lifelong. Common drugs include tacrolimus, cyclosporine, mycophenolate mofetil, and corticosteroids.
Immunosuppression brings risks, particularly infections and increased susceptibility to certain cancers. The medical team must strike a delicate balance, tailoring medication regimens to each patient’s needs.
Postoperative Care and Complications
Recovery after liver transplantation involves intensive monitoring in the hospital, followed by regular outpatient visits. Patients are watched for signs of rejection, infection, bile duct problems, blood clots, and organ failure. Early intervention is crucial for managing complications.
Long-term care includes routine laboratory tests, imaging, medication adjustments, and lifestyle counseling. Adherence to medical advice, healthy diet, exercise, and avoidance of alcohol are essential for graft longevity.
Outcomes and Quality of Life
Advancements in surgical technique, immunosuppression, and postoperative care have dramatically improved outcomes. Five-year survival rates for liver transplant recipients now exceed 75% in many centers. For many, transplantation offers not only longer life, but also restoration of energy, productivity, and participation in family and community.
Challenges and Ethical Considerations
Despite progress, liver transplantation faces significant obstacles:
- Organ shortage: The demand far exceeds the supply, resulting in waiting lists and, tragically, patients dying before an organ becomes available.
- Allocation fairness: Ethical dilemmas arise in deciding who receives scarce organs. Criteria must balance urgency, likelihood of success, and social equity.
- Financial and logistical barriers: Access to transplantation depends on resources, insurance, geography, and health system infrastructure.
- Psychosocial impact: Both recipients and donors require ongoing emotional support to navigate fear, anxiety, and adjustment to new realities.
Nursing Care of Patients After Liver Transplantation
Successful outcomes depend not only on surgical expertise but also on vigilant, coordinated nursing care throughout the perioperative and postoperative periods. Nurses play an essential role in monitoring, preventing complications, supporting recovery, and educating patients and families.
Preoperative Nursing Care
Patient Assessment and Preparation
- Comprehensive assessment of physical, psychological, and social health status.
- Review of laboratory studies, imaging results, and cardiac, pulmonary, and renal function.
- Education about the procedure, potential risks, immunosuppression, and lifestyle changes post-transplant.
- Emotional support, addressing anxieties and expectations.
- Nutritional support to optimize patient’s status before surgery.
Preoperative Teaching
- Discussion about the surgical process, length of hospital stay, and recovery stages.
- Instructions on infection prevention measures (e.g., hand hygiene, avoiding sick contacts).
- Guidance on medication management, including discontinuation of drugs that may interfere with transplantation.
Immediate Postoperative Nursing Care
Monitoring and Assessment
- Frequent assessment of vital signs, including temperature, pulse, blood pressure, and respiratory rate.
- Continuous monitoring for signs of bleeding, shock, and hemodynamic instability.
- Observing for early signs of graft dysfunction, such as jaundice, coagulopathy, and altered mental status.
- Assessing fluid and electrolyte balance, blood glucose, and renal function.
- Monitoring central venous pressure (CVP) and pulmonary artery pressures if indicated.
Pain Management
- Evaluation of pain levels using standardized scales.
- Administration of prescribed analgesics, considering altered metabolism in liver transplant patients.
- Non-pharmacological approaches, such as relaxation techniques and positioning.
Infection Prevention
- Strict aseptic technique during all procedures, including dressing changes and intravenous line care.
- Early identification and intervention for fever or local infections.
- Prophylactic antibiotics as per protocol.
- Monitoring white blood cell count and other markers of infection.
Long-Term Postoperative Nursing Care
Immunosuppression Management
- Understanding and administering immunosuppressive medications (e.g., tacrolimus, cyclosporine, mycophenolate mofetil, corticosteroids).
- Monitoring for side effects such as nephrotoxicity, hypertension, diabetes, and increased infection risk.
- Educating patient and family about lifelong medication adherence and scheduled laboratory monitoring.
Complication Surveillance
- Early detection of acute or chronic graft rejection (e.g., fever, malaise, abnormal liver function tests, jaundice).
- Assessment for vascular complications (e.g., hepatic artery thrombosis, portal vein thrombosis).
- Recognition of biliary complications (e.g., bile leak, biliary strictures).
- Prevention and prompt management of infection, including opportunistic pathogens.
- Monitoring for post-transplant lymphoproliferative disorder (PTLD) and other malignancies.
Nutritional Support
- Assessment and planning of individualized dietary needs to prevent malnutrition and support healing.
- Managing restrictions (e.g., sodium, fluids) as indicated for comorbid conditions like renal dysfunction.
- Education on food safety to minimize infection risk, such as avoiding raw or undercooked foods.
Psychosocial Support
- Providing emotional support to address anxiety, depression, and adjustment issues.
- Facilitating access to social workers, psychologists, and support groups.
- Encouraging family involvement and communication.
Rehabilitation and Activity
- Guidance on early ambulation and gradual increase in physical activity to prevent complications such as deep vein thrombosis and promote healing.
- Education regarding restrictions on heavy lifting and strenuous activities until cleared by the transplant team.
Patient and Family Education
Effective education is central to positive outcomes. Nurses must provide clear, ongoing instruction about:
- Medication regimen and potential interactions.
- Warning signs of complications – when and how to seek immediate medical attention.
- Importance of scheduled follow-up appointments and laboratory testing.
- Healthy lifestyle choices, including smoking cessation, alcohol avoidance, and regular exercise.
- Strategies for coping with the psychological impact of transplantation.
- Infection prevention, such as immunization schedules and personal hygiene.
Discharge Planning and Home Care
Transitioning to Home Care
- Assessment of home environment for safety, cleanliness, and access to healthcare.
- Coordination with community health services for ongoing nursing and medical visits.
- Provision of written and verbal instructions for daily care, medication administration, and symptom monitoring.
Support Systems
- Facilitating access to peer support networks and transplant organizations.
- Ongoing communication between the transplant team and community providers.
Common Challenges and Solutions
Medication Adherence
- Use of pillboxes, alarms, and reminders to promote adherence.
- Addressing barriers such as financial constraints or misunderstanding of instructions.
Managing Side Effects
- Regular assessment and management of medication-induced side effects.
- Collaboration with physicians for dose adjustments or substitution.
Preventing Readmission
- Comprehensive education on warning signs and timely intervention.
- Coordination of care with outpatient providers.
Role of the Multidisciplinary Team
Nursing care is coordinated within a multidisciplinary framework. Nurses work alongside physicians, pharmacists, dieticians, social workers, and physiotherapists to ensure holistic patient management. Clear documentation, communication, and collaboration are essential to prevent errors and optimize patient outcomes.
REFERENCES
- American College of Gastroenterology. Liver Transplantation. https://gi.org/topics/liver-transplantation/). Updated 7/2023.
- American Liver Foundation. Liver Transplant. https://liverfoundation.org/for-patients/about-the-liver/liver-transplant/). Updated 3/22/2024.
- Busuttil RW, et al., eds. Donor selection and management. In: Transplantation of the Liver. 3rd ed. Saunders Elsevier; 2015. https://www.clinicalkey.com.
- Cahn-Fuller KL, Parent B. Transplant eligibility for patients with affective and psychotic disorders: a review of practices and a call for justice. https://pmc.ncbi.nlm.nih.gov/articles/PMC5721543/. BMC Med Ethics. 2017;18(1):72.
- Ekser, B, et al. Current status of combined liver-kidney transplantation. International Journal of Surgery. 2020; doi:10.1016/j.ijsu.2020.02.008.
- Dababneh Y, Mousa OY. Liver Transplantation. [Updated 2025 Jun 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559161/
- Kwong A, et al. OPTN/SRTR 2018 annual data report: Liver. American Journal of Transplantation. 2020; doi:10.1111/ajt.15674.
- Merck Manual Professional Version. Liver Transplantation. https://www.merckmanuals.com/professional/immunology-allergic-disorders/transplantation/liver-transplantation. Updated 8/2022.
- National Institute of Diabetes and Digestive and Kidney Diseases (U.S.). Liver Transplant. https://www.niddk.nih.gov/health-information/liver-disease/liver-transplant. Updated 3/2017.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





