The concept of living liver donation and transplantation stands as one of modern medicine’s most extraordinary achievements—an intersection of scientific progress and human compassion. With the rising prevalence of liver diseases globally, this procedure offers hope not only for patients on transplant waiting lists but also for families seeking a lifeline for their loved ones.
Introduction to Liver Transplantation
The liver, the largest internal organ, performs unimaginable feats: detoxifying blood, producing proteins, regulating nutrients, and supporting immune function. For individuals with severe liver diseases—such as cirrhosis, hepatitis, or genetic disorders—a liver transplant may be the only definitive treatment. Traditionally, these transplants involved organs from deceased donors. However, with increasing demand and a critical shortage of available organs, living donor liver transplants have become a vital alternative.
What Is a Living Liver Donor Transplant?
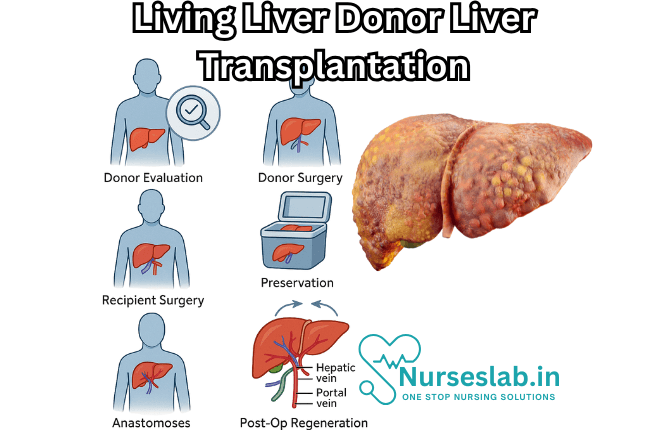
A living liver donor transplant involves removing a portion of the liver from a healthy donor and transplanting it into a recipient whose liver is failing. Remarkably, the liver possesses unique regenerative capabilities: both the donor’s and recipient’s livers will grow and regain normal function within weeks. This procedure is typically reserved for children and adults with end-stage liver disease who cannot wait for a deceased donor.
Types of Living Liver Donation
- Related Donation: Most living liver donors are family members—parents, siblings, or adult children—whose genetic similarity often reduces rejection risk.
- Unrelated Donation: Occasionally, non-related individuals, such as friends or altruistic strangers, may volunteer to donate. This is known as non-directed or altruistic donation.
Eligibility Criteria for Living Liver Donors
Not everyone can be a living liver donor. Rigorous screening ensures the safety of both parties. Criteria typically include:
- Age between 18 and 60 years
- Good physical and mental health
- Blood type compatibility with the recipient
- Absence of significant medical conditions (e.g., liver disease, heart problems, infections)
- Psychological readiness and informed consent
- Healthy body weight and lifestyle habits
A multidisciplinary team—comprised of transplant surgeons, hepatologists, psychologists, and social workers—conducts extensive evaluations. These include blood tests, imaging studies (CT or MRI scans), and psychological assessment to ensure that the donor is well-informed and fully prepared for the process.
The Living Liver Donation Process
Pre-Donation Evaluation
Before any surgery, both donor and recipient undergo extensive evaluation:
- Medical assessment: General health, liver anatomy, and compatibility
- Psychosocial assessment: Motivation, emotional support, and financial readiness
- Education and counseling: Risks, benefits, and long-term considerations
The Transplant Surgery
The living donor liver transplant is a complex operation:
- Donor surgery: The donor is placed under general anesthesia. Surgeons remove a portion of the liver—typically the left lobe for pediatric recipients and the right lobe for adults.
- Recipient surgery: The diseased liver is removed and replaced with the healthy liver segment. Blood vessels and bile ducts are meticulously reconnected.
Both procedures require a highly skilled team and can last several hours. Advanced surgical techniques, improved imaging, and careful planning help minimize risks.
Post-Operative Care
After surgery, both donor and recipient spend several days in the hospital’s intensive care unit for close monitoring.
- Donor recovery: Most donors stay in the hospital for a week, with full recovery expected within six to twelve weeks. Regular follow-up ensures liver regeneration and overall health.
- Recipient recovery: Recipients require immunosuppressive medications to prevent organ rejection and ongoing medical follow-up. Their hospital stay may range from two to three weeks, depending on complications.
Benefits of Living Liver Donation
Living liver donation offers several advantages:
- Shorter waiting time: Recipients can undergo transplantation sooner, reducing the risk of deterioration and death while waiting for an organ.
- Better organ quality: Organs from living donors are typically healthier, as the donor is thoroughly screened and the time between organ removal and transplantation is brief.
- Scheduled surgery: Transplants can be planned at optimal times for both donor and recipient.
- Emotional impact: Donors often describe a profound sense of fulfillment and connection from saving a life.
Risks and Considerations for Donors
While living liver donation is generally safe, it is not without risks. Donors must be aware of possible complications:
- Surgical risks: Bleeding, infection, blood clots, bile duct injury, and anesthesia complications
- Long-term risks: Most donors regain full liver function, but rare complications may include persistent pain, digestive issues, or mental health impacts.
- Financial and lifestyle impacts: Time off work, insurance implications, and potential emotional challenges
Ethical considerations are paramount. Donors must make the decision freely, without coercion, and all aspects of the process should adhere to strict medical and ethical standards.
Risks and Outcomes for Recipients
Recipients face their own risks:
- Surgical complications: Bleeding, infection, rejection, bile duct problems
- Immunosuppression: Medications to prevent rejection can increase susceptibility to infections and other health problems.
- Long-term care: Recipients require lifelong medical follow-up and medication.
Nonetheless, the benefits are substantial—many recipients experience dramatic improvements in quality of life, survival, and the ability to return to normal activities.
Ethical and Social Dimensions
Living liver donation raises important societal and ethical questions:
- How do we ensure donor autonomy and informed consent?
- What safeguards are in place to prevent coercion or financial exploitation?
- How do cultural perceptions shape the willingness to donate?
Ongoing education, public awareness campaigns, and robust legal frameworks help address these concerns, making the process transparent and safe for all participants.
Advances in Living Liver Transplantation
Medical innovation continues to evolve. Surgeons are exploring minimally invasive techniques, robotic-assisted surgery, and better immunosuppressive drugs. Improved imaging and genetic testing help match donors and recipients more precisely, reducing risks and improving outcomes.
Nursing Care of Patients with Living Liver Donor and Transplant
Nurses play a pivotal role throughout the transplantation journey, providing holistic, multidisciplinary, and individualized care to ensure the best possible outcomes for all parties involved.
Preoperative Nursing Care
For the Living Liver Donor
- Health Assessment: Comprehensive physical and psychological assessment is essential. Nurses must coordinate and assist with a range of diagnostic tests, including liver function tests, imaging studies (CT, MRI), and cardiac assessments. Psychological evaluation ensures that the donor is mentally prepared and free from coercion.
- Education: The nurse provides thorough preoperative education about the surgical procedure, risks, benefits, and expected recovery. Education should address potential complications, pain management, activity restrictions, and the importance of follow-up care.
- Informed Consent: Nurses ensure that the donor fully understands the procedure and voluntarily provides informed consent. This includes reviewing all documentation and providing support for any questions or concerns.
- Psychosocial Support: Emotional support for the donor and their family is critical. Nurses facilitate counseling, peer support groups, and access to social services as needed.
For the Liver Transplant Recipient
- Preoperative Stabilization: Recipients often present with complications of liver failure such as ascites, coagulopathy, encephalopathy, or infections. Nurses must monitor and manage these conditions, optimize nutritional status, and correct metabolic imbalances.
- Preoperative Teaching: Recipients and their families require detailed education about the transplant procedure, expected postoperative course, immunosuppressive therapy, and the necessity of lifelong follow-up.
- Psychological Preparation: Anticipation of major surgery can cause anxiety and depression. Nurses provide reassurance, address fears, and arrange for psychological support as appropriate.
- Infection Prevention: Preoperative care includes strict aseptic techniques and infection control measures to minimize perioperative infection risk.
Intraoperative Nursing Care
For Both Donor and Recipient
- Patient Advocacy: The perioperative nurse acts as the advocate for both donor and recipient, ensuring their safety and dignity throughout the procedure.
- Monitoring: Nurses are responsible for continuous monitoring of vital signs, fluid balance, blood loss, and laboratory values. They facilitate communication between the surgical team, anesthesiologists, and other support staff.
- Instrument and Tissue Handling: Strict aseptic technique and proper handling of surgical instruments and tissue samples are crucial to reduce infection and improve surgical outcomes.
- Documentation: Accurate and timely documentation of intraoperative events, interventions, and patient responses is essential for continuity of care.
Immediate Postoperative Nursing Care
For the Living Liver Donor
- Pain Management: Effective pain control is a priority. Strategies include PCA pumps, epidural analgesia, or oral medications, tailored to individual needs and side effect profiles.
- Monitoring for Complications: Nurses must closely observe for signs of bleeding, bile leaks, infection, respiratory complications, and venous thromboembolism. Frequent assessment of vital signs, surgical site, drains, and laboratory values is mandatory.
- Early Mobilization: Encouraging early ambulation helps prevent deep vein thrombosis and promotes recovery. Nurses assist in safe mobilization, physical therapy, and pulmonary exercises.
- Nutrition and Hydration: Gradual progression from IV fluids to oral intake is required. Nurses monitor for tolerance, manage nausea, and encourage a balanced diet as per medical advice.
- Psychosocial Support: Postoperative emotional well-being is as important as physical recovery. Nurses should facilitate supportive counseling and address any feelings of guilt, anxiety, or depression.
For the Liver Transplant Recipient
- Hemodynamic and Respiratory Stability: Recipients require intensive monitoring in the immediate postoperative period. Nurses assess for signs of graft dysfunction, hemodynamic instability, respiratory compromise, and manage supportive devices such as ventilators.
- Immunosuppression Management: Immunosuppressive drugs are critical for graft survival but increase infection risk. Nurses administer medications precisely, monitor for side effects, and educate patients about adherence and signs of rejection/infection.
- Infection Control: Vigilant infection prevention through aseptic techniques, hand hygiene, and isolation precautions when necessary is essential. Nurses monitor for early signs of infection and promptly report concerns.
- Renal Function and Fluid Balance: Postoperative acute kidney injury is a risk; nurses monitor urine output, electrolytes, and fluid status closely.
- Graft Function Monitoring: Serial assessments of liver enzymes, coagulation profiles, and bilirubin are required. Nurses look for clinical signs of rejection, such as fever, jaundice, or abdominal pain, and report changes immediately.
- Pain and Comfort: Managing pain, nausea, pruritus, and sleep disturbances is vital for promoting healing and well-being.
- Patient and Family Education: Continuous education about medication regimens, wound care, activity limitations, infection warning signs, and lifestyle modifications should be provided.
- Psychological Support: Adjustment to life post-transplant can be overwhelming. Nurses provide ongoing emotional support and coordinate with mental health professionals.
Long-term Nursing Care and Follow-Up
Living Liver Donor
- Physical Recovery: Regular follow-up to monitor healing, liver regeneration, and detect late complications (e.g., incisional hernia, biliary issues) is necessary. Nurses coordinate appointments and facilitate communication between donor and healthcare team.
- Psychosocial Well-being: Donors may experience a range of emotions post-donation, from pride to anxiety. Ongoing counseling and peer support can help address these concerns.
- Lifestyle Guidance: Nurses encourage a return to normal activities, healthy diet, avoidance of hepatotoxins (alcohol, certain medications), and maintenance of overall wellness.
Liver Transplant Recipient
- Immunosuppression and Medication Adherence: Long-term immunosuppressive therapy requires strict adherence. Nurses reinforce the importance of medication schedules and regular laboratory monitoring.
- Complication Surveillance: Nurses educate and monitor for late complications, such as chronic rejection, recurrent disease, cardiovascular issues, and malignancies.
- Infection Prevention: Recipients remain immunocompromised for life; infection prevention through vaccinations, hygiene, and avoidance of sick contacts remains a priority.
- Quality of Life Support: Assisting patients in returning to daily life, work, and social activities, while recognizing the challenges of chronic disease management, is essential.
- Mental Health: Chronic illness and transplantation can impact mental health. Nurses screen for depression, anxiety, and adjustment disorders, and facilitate referrals as needed.
Ethical and Cultural Considerations
- Autonomy and Informed Consent: Nurses uphold the principle of autonomy by ensuring that both donors and recipients make informed, voluntary decisions about their care.
- Cultural Sensitivity: Transplantation can have unique cultural and religious implications. Nurses must provide culturally competent care, respecting beliefs and practices related to organ donation and surgery.
- Confidentiality: The privacy of both donor and recipient should be strictly maintained throughout the process.
REFERENCES
- American Liver Foundation. Living Donor Liver Transplant Information Center: An Introduction for Donors and Recipients. https://liverfoundation.org/liver-diseases/treatment/living-donor-liver-transplant-information-center/an-introduction-for-donors-and-recipients/. Updated 2/5/2024.
- Townsend CM Jr, et al. Liver transplantation. In: Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 21st ed. Elsevier; 2022. https://www.clinicalkey.com.
- American Transplant Foundation. Living Donation Guide https://www.americantransplantfoundation.org/about-transplant/living-donation/.
- Au KP, Chok KSH. Minimally invasive donor hepatectomy, are we ready for prime time? (https://pubmed.ncbi.nlm.nih.gov/29991875/) World J Gastroenterol. 2018 Jul 7;24(25):2698-2709.
- Dew MA, Butt Z, Humar A, DiMartini AF. Long-Term Medical and Psychosocial Outcomes in Living Liver Donors. https://pmc.ncbi.nlm.nih.gov/articles/PMC5510163/). Am J Transplant. 2017 Apr;17(4):880-892.
- Cameron AM, et al. Role of liver transplantation for portal hypertension. In: Current Surgical Therapy. 13th ed. Elsevier; 2020. https://www.clinicalkey.com.
- Nydam TL, Reddy MS, Pomfret EA, Rela M. Progression of living liver donation worldwide. https://pubmed.ncbi.nlm.nih.gov/29432257/). Curr Opin Organ Transplant. 2018 Apr;23(2):162-168.
- Hendrickse A, Ko J, Sakai T. The care of donors and recipients in adult living donor liver transplantation. BJA Educ. 2022 Oct;22(10):387-395. doi: 10.1016/j.bjae.2022.06.004. Epub 2022 Aug 23. PMID: 36132878; PMCID: PMC9482866.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





