A Comprehensive Guide to Orchiectomy
Introduction
Orchiectomy is a surgical procedure involving the removal of one or both testicles. As a medical intervention with deep historical roots, it serves a variety of purposes ranging from treatment of specific medical conditions to gender-affirming care for transgender and non-binary individuals. Its significance spans across urology, oncology, endocrinology, and mental health, making it a multifaceted topic within the realm of modern medicine.
Indications for Orchiectomy
The decision to undergo orchiectomy is often guided by a clear medical rationale or personal need. The most common indications include:
- Testicular Cancer: Orchiectomy is the primary treatment for testicular tumors, typically performed to prevent the spread of malignancy.
- Prostate Cancer: In some advanced cases, orchiectomy is performed to lower testosterone levels, which can help slow the progression of prostate cancer.
- Severe Trauma or Infection: Irreversible damage to the testicles due to injury or infection may necessitate removal to prevent further health complications.
- Testicular Torsion: When blood supply is cut off to a testicle due to twisting (torsion), and if the tissue becomes necrotic, removal may be warranted.
- Hormonal Therapy: As part of gender-affirming surgery for transgender women or non-binary people seeking to lower testosterone and reduce male secondary sexual characteristics.
- Other Medical Conditions: Such as chronic pain syndromes, or as a palliative measure in rare cases of advanced disease.
Types of Orchiectomy
There are several types of orchiectomy, each tailored to the underlying condition and patient goals:
- Simple Orchiectomy: Removal of one or both testicles through a small incision in the scrotum. This is most commonly performed for hormone reduction or for non-malignant testicular conditions.
- Radical Inguinal Orchiectomy: The standard approach for testicular cancer, involving removal of the testicle and spermatic cord through an incision in the groin. This minimizes the risk of spreading cancer cells.
- Subcapsular Orchiectomy: Removal of the glandular tissue inside the testicle, leaving the outer shell for cosmetic purposes. Sometimes chosen for hormonal management in prostate cancer.
- Bilateral vs. Unilateral: Bilateral orchiectomy involves removing both testicles, resulting in complete cessation of natural testosterone production. Unilateral means only one testicle is removed, with partial hormonal function retained.
Preparation for Orchiectomy
Preparation for orchiectomy involves a comprehensive evaluation by a healthcare provider. This process typically includes:
- Detailed medical history and physical examination
- Imaging studies (such as ultrasound or CT scans) to evaluate the anatomy and pathology
- Blood tests to assess overall health and hormone levels
- Discussion of risks, benefits, and alternatives, often involving multidisciplinary teams such as urologists, oncologists, and mental health professionals
- Informed consent, including an understanding of the potential long-term consequences
In some cases, sperm banking may be discussed for those wishing to preserve fertility.
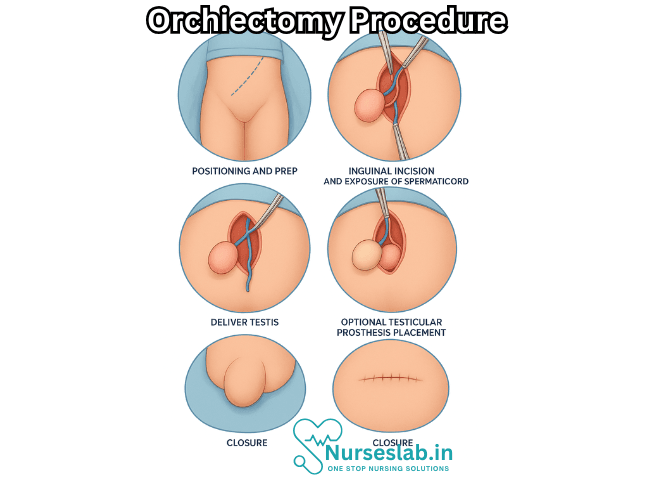
The Orchiectomy Procedure
The surgical technique varies according to the type of orchiectomy:
Simple Orchiectomy
A small incision is made in the scrotum under local, regional, or general anesthesia. The testicle(s) and part of the spermatic cord are removed, and the incision is closed with sutures.
Radical Inguinal Orchiectomy
An incision is made in the groin area, and the testicle, along with the spermatic cord, is carefully dissected and removed to prevent cancer cell spillage. The wound is then sutured.
Subcapsular Orchiectomy
Only the hormone-producing tissue is removed, sparing the outer tissue for appearance.
The procedure typically lasts between 30 minutes to one hour, and most patients are discharged the same day or after a short hospital stay.
Recovery and Aftercare
Post-operative recovery is generally straightforward, but depends on the individual’s health and specific surgical context.
- Pain and swelling are common, managed with pain relievers and ice packs.
- Physical activity should be limited for a few weeks, especially activities that put strain on the groin area.
- Follow-up visits are necessary to monitor healing and manage any complications.
- If the orchiectomy was for cancer, further treatment such as chemotherapy, radiotherapy, or surveillance may be required.
Most wounds heal within two to four weeks.
Risks and Complications
Like any surgery, orchiectomy carries potential risks:
- Infection at the incision site
- Bleeding or hematoma
- Chronic pain or discomfort
- Scarring and changes in scrotal appearance
- Psychological impact, including feelings of loss, altered body image, or depression
- If both testicles are removed: infertility and permanent loss of natural testosterone production, which may require lifelong hormone replacement therapy
Most patients experience few complications, especially when the procedure is performed by experienced surgeons and post-operative instructions are carefully followed.
Hormonal and Psychological Implications
The removal of one or both testicles results in a significant reduction or complete loss of testosterone production. The implications of this depend on whether one or both testicles were removed and the reason for surgery.
Unilateral Orchiectomy: If only one testicle is removed, most individuals retain normal hormonal function and fertility, as the remaining testicle compensates.
Bilateral Orchiectomy: Removing both testicles causes permanent infertility and a sharp drop in testosterone, which can lead to symptoms such as reduced libido, erectile dysfunction, hot flashes, fatigue, loss of muscle mass, and osteoporosis. To address these effects, hormone replacement therapy (HRT) may be recommended.
Psychological responses vary. For some, orchiectomy brings relief and aligns with personal health or identity goals. Others may experience grief, anxiety, or challenges with self-image. Mental health support and counseling are important components of holistic care before and after the procedure.
Orchiectomy in Gender-Affirming Care
Orchiectomy plays a vital role in gender-affirming medical care for some transgender women and non-binary people. For those seeking to lower testosterone levels, reduce gender dysphoria, or discontinue anti-androgen medications, orchiectomy offers a permanent solution. The procedure may be performed alone or alongside other surgeries such as vaginoplasty.
Decisions regarding orchiectomy in this context are highly personal and made in collaboration with knowledgeable health professionals to ensure informed consent and supportive care.
Alternatives to Orchiectomy
There are non-surgical alternatives for hormone reduction, such as chemical or medical castration using medications (e.g., anti-androgens, GnRH agonists) that suppress testosterone production. These options are reversible and may be preferred by those who wish to avoid surgery or its permanency.
For testicular cancer, alternatives depend on the stage and type of tumor but may include partial orchidectomy (removal of part of the testicle), close surveillance, or adjuvant therapy.
Fertility Considerations
Patients considering orchiectomy, especially bilateral removal, should discuss fertility preservation options with their healthcare provider. Sperm banking before surgery is an option for many, and should be considered early in the process if future biological parenthood is desired.
Historical and Cultural Aspects
The history of orchiectomy stretches back thousands of years, with varying cultural and medical implications. In ancient times, castration was practiced for religious, social, or punitive reasons, and eunuchs played unique roles in some societies. Today, the procedure is strictly medical and governed by ethical guidelines emphasizing patient autonomy and well-being.
Nursing Care of Patients Undergoing Orchiectomy
Although the operation is often straightforward, it carries significant physical and psychological implications for patients. Holistic nursing care is essential to facilitate recovery, manage complications, and support emotional well-being.
Preoperative Nursing Care
1. Psychological Preparation
- Assessment of anxiety and knowledge: Evaluate the patient’s understanding of the procedure, its purpose, and its implications, including fertility and hormonal consequences.
- Emotional support: Provide reassurance, allow expression of concerns, and address fears regarding body image, masculinity, or sexuality.
- Counseling and education: Offer information about the surgical process, expected outcomes, and recovery. Discuss possible prosthesis implantation and its timing if appropriate.
- Referral: Arrange psychological consultation or peer counseling if needed, especially for patients struggling with the diagnosis or anticipated changes.
2. Physical Preparation
- Preoperative assessment: Obtain a thorough medical history, focusing on allergies, bleeding disorders, and current medications.
- Laboratory investigations: Ensure completion of required preoperative tests, such as CBC, coagulation profile, renal function tests, and type and screen for blood products if indicated.
- Preoperative instructions: Educate the patient about fasting protocols, medication adjustments (e.g., anticoagulants), and pre-surgical hygiene, including shaving or cleansing the surgical site as per hospital protocol.
- Informed consent: Confirm that the patient (and, if applicable, family) has signed the consent form after discussing risks, benefits, and alternatives with the surgical team.
Intraoperative Nursing Care
1. Patient Safety
- Identification: Verify patient identity, surgical site, and type of procedure with the surgical team using the “time out” protocol.
- Positioning: Position the patient appropriately (usually supine), ensuring comfort and prevention of pressure injuries.
- Aseptic technique: Maintain strict asepsis to prevent surgical site infections.
- Monitoring: Assist in monitoring vital signs, oxygen saturation, and overall patient status throughout the procedure.
2. Equipment and Specimen Handling
- Preparation: Ensure availability and functioning of necessary equipment, including surgical instruments, suction, cautery, and optionally, testicular prosthesis.
- Specimen handling: Properly label and transport removed tissue for pathological examination as per protocol.
Postoperative Nursing Care
1. Immediate Postoperative Care
- Airway and breathing: Monitor airway, respiratory rate, and oxygen saturation until the patient regains full consciousness.
- Circulation: Observe vital signs closely for signs of bleeding or shock.
- Pain management: Assess pain level regularly and administer analgesics as prescribed. Encourage use of a scrotal support or towel roll under the scrotum to reduce discomfort and swelling.
- Surgical site monitoring: Inspect the incision for bleeding, hematoma, swelling, or signs of infection (redness, warmth, discharge). Check for excessive drainage and reinforce dressings as necessary.
- Prevention of complications: Encourage early but gentle mobilization to prevent deep vein thrombosis (DVT). Monitor for urinary retention and bowel function post-anesthesia.
- Fluid and nutritional management: Initially start with clear fluids, then progress diet as tolerated. Monitor for nausea or vomiting, managing as needed.
2. Ongoing Postoperative Care
- Pain and discomfort: Continue to monitor and manage pain, utilizing pharmacological and non-pharmacological interventions such as ice packs, positioning, and relaxation techniques.
- Incision care: Instruct patient on wound care, keeping the area clean and dry, and recognizing signs of infection. Advise when to change dressings and when to seek help.
- Activity and mobility: Encourage gradual resumption of normal activities as tolerated, avoiding strenuous activity, heavy lifting, or sexual activity until cleared by the surgeon.
- Prevention of complications: Monitor for fever, persistent pain, excessive swelling, hematoma, or signs of systemic infection. Watch for symptoms of pulmonary embolism or DVT, such as leg pain or swelling, chest pain, or shortness of breath.
3. Psychological and Emotional Support
- Counseling and reassurance: Continue to address concerns about body image, sexuality, fertility, and future health. Provide up-to-date information about prognosis and long-term outcomes.
- Support for partners and family: Involve significant others in teaching and support, as appropriate, to help them understand and assist in the patient’s recovery.
- Referral to support groups: Suggest patient support groups or counseling services specializing in cancer, surgical recovery, or gender-affirming care, depending on the patient’s context.
Discharge Planning and Home Care
1. Patient Education
- Incision and wound care: Teach proper wound care, signs of infection, and the importance of keeping the area dry.
- Pain management: Advise on use of prescribed pain medications and non-pharmacological techniques at home.
- Activity restrictions: Instruct on limitations regarding physical activity, driving, and sexual intercourse until cleared by the healthcare provider.
- Scrotal support: Recommend wearing supportive underwear or a scrotal support garment until swelling subsides.
- Follow-up appointments: Emphasize the importance of keeping surgical follow-ups and monitoring for complications or recurrence of disease.
- Signs to report: Advise prompt reporting of fever, increasing pain, redness, discharge from the incision, swelling, or difficulty urinating.
2. Long-term Considerations
- Hormonal replacement: After bilateral orchiectomy, discuss the need for lifelong testosterone replacement therapy (TRT), monitoring for symptoms of deficiency and side effects.
- Fertility options: Address sperm banking or fertility preservation preoperatively if future fertility is a concern, especially for patients undergoing the procedure for cancer or before gender-affirming therapy.
- Body image and sexuality: Discuss options for testicular prosthesis and referral to counseling for those experiencing distress about body image or sexuality.
- Psychosocial adaptation: Offer ongoing support and resources to help patients adjust to changes in self-perception and lifestyle.
Special Considerations
1. Pediatric and Adolescent Patients
- Family involvement: Involve parents or guardians in the preparation and recovery process. Offer age-appropriate explanations and emotional support.
- Fertility concerns: Address future fertility and hormonal implications with the patient and family.
2. Gender-Affirming Orchiectomy
- Respect for identity: Use affirming language and respect the patient’s chosen name and pronouns.
- Holistic support: Coordinate with multidisciplinary teams, including mental health professionals and endocrinologists, as needed.
REFERENCES
- American Cancer Society. Surgery for Testicular Cancer. https://www.cancer.org/cancer/types/testicular-cancer/treating/surgery.html. Last revised 5/2018.
- Okoye E, Saikali SW. Orchiectomy. https://www.ncbi.nlm.nih.gov/books/NBK562336/. 2022 Aug 28. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan.
- Anderson E, Pascoe C, Sathianathen N, Katz D, Murphy D, Lawrentschuk N. Subinguinal orchiectomy-A minimally invasive approach to open surgery. BJUI Compass. 2020;1(5):160-164. doi:10.1002/bco2.33
- Gupta V, Giridhar A, Sharma R, Ahmed SM, Raju KVVN, Rao TS. Malignancy in an undescended intra-abdominal testis: A single institution experience. Indian J Surg Oncol. 2021;12(1):133-138. doi:10.1007/s13193-020-01262-9
- van der Sluis WB, Steensma TD, Bouman MB. Orchiectomy in transgender individuals: A motivation analysis and report of surgical outcomes. Int J Transgend Health. 2020;21(2):176-181. doi:10.1080/26895269.2020.1749921
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





