Prostatic Urethral Lift: An Innovative Approach to Treating Benign Prostatic Hyperplasia
Prostatic Urethral Lift (PUL) is a minimally invasive procedure for treating benign prostatic hyperplasia (BPH), using small implants to retract prostate tissue and relieve urethral obstruction—offering symptom relief with reduced risk to sexual function and faster recovery compared to traditional surgery.
Introduction
Benign Prostatic Hyperplasia (BPH) is a common condition affecting millions of men worldwide, particularly as they age. Characterized by the enlargement of the prostate gland, BPH can lead to bothersome lower urinary tract symptoms (LUTS), including frequent urination, nocturia, weak urinary stream, and incomplete bladder emptying. Traditionally, the management of BPH has included medications and surgical interventions, such as transurethral resection of the prostate (TURP). In recent years, minimally invasive techniques have emerged, offering patients effective symptom relief with reduced side effects and downtime. Among these, the Prostatic Urethral Lift (PUL) has gained prominence for its unique mechanism and favorable patient outcomes.
What Is Prostatic Urethral Lift?
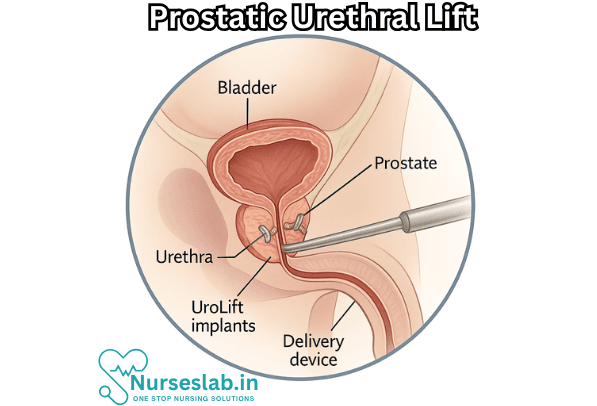
Prostatic Urethral Lift is a minimally invasive surgical procedure designed to treat BPH by opening the urethral channel within the prostate without removing or destroying prostate tissue. The procedure uses small implants to retract the enlarged prostatic lobes, thus relieving pressure on the urethra and improving urinary flow. Unlike traditional surgeries, PUL does not require cutting, heating, or removal of tissue, which translates to a lower risk of complications and a quicker recovery.
Indications and Patient Selection
PUL is typically indicated for men with symptomatic BPH who have failed conservative management with medications or who prefer a minimally invasive option. Ideal candidates generally have prostates of a certain size (typically less than 80 cc), with lateral lobe enlargement rather than medial (middle lobe) obstruction. Patients who wish to preserve sexual function, particularly ejaculation, may especially benefit from PUL, as the procedure has a low risk of causing sexual side effects.
Key Eligibility Criteria:
- Moderate to severe BPH symptoms impacting quality of life
- Prostate size less than 80cc
- No significant median lobe enlargement
- Desire to preserve sexual function
- Failure or intolerance to medications (alpha blockers, 5-alpha-reductase inhibitors)
Procedure Overview
The PUL is generally performed on an outpatient basis and can be completed in less than an hour. The procedure involves the following steps:
- The patient is placed under local, spinal, or mild general anesthesia.
- A cystoscope (a thin, flexible tube with a camera) is inserted into the urethra and advanced to the area of the prostate.
- Through the cystoscope, specialized delivery devices are used to place small permanent implants on both sides of the prostate.
- These implants compress the obstructive prostatic tissue, creating an open channel for urine to pass through.
- Once the desired effect is achieved, the instruments are removed and the patient is monitored for a short period before discharge.
The UroLift System
One of the most widely used systems for PUL is the UroLift® System. This FDA-approved device consists of tiny suture-like implants made from stainless steel and nitinol. The system is engineered to be biocompatible and durable, providing lasting relief without the need for further intervention.
Benefits of Prostatic Urethral Lift
PUL offers several significant advantages over traditional treatments for BPH:
- Minimally Invasive: The procedure does not involve cutting, heating, or removal of prostate tissue, reducing the risk of bleeding and other complications.
- Rapid Symptom Relief: Most patients experience improvement in urinary symptoms within days of the procedure.
- Quick Recovery: The outpatient nature of PUL means that patients can often return to normal activities within 2-3 days.
- Preservation of Sexual Function: Studies have shown that PUL has a negligible risk of causing erectile dysfunction or retrograde ejaculation, problems often seen with other surgical interventions.
- Reduced Use of Catheters: The need for postoperative catheterization is lower compared to TURP and other procedures.
- Durable Results: Clinical trials indicate sustained improvement in urinary symptoms for at least 3-5 years post-procedure.
Risks and Potential Complications
As with any surgical procedure, PUL is not without risks. However, the overall complication rate is low. Common adverse events include:
- Mild to moderate pain or discomfort during urination (dysuria)
- Hematuria (blood in the urine), which is usually temporary
- Urgency or frequency of urination for several days post-procedure
- Pain or discomfort in the pelvic region
- Rarely, urinary tract infection or implant dislodgement
Most of these symptoms resolve spontaneously or with simple treatments. Serious complications such as infection, implant migration, or urethral injury are infrequent.
Recovery and Aftercare
Following a PUL, patients are typically observed for a brief period to ensure there are no immediate complications. Most can return home the same day. Recovery is generally rapid:
- Most men resume normal activity within 1-2 days.
- Mild side effects such as discomfort, urgency, or frequency typically resolve within a week.
- Patients are advised to avoid strenuous activity and heavy lifting for several days.
- Follow-up visits are scheduled to monitor progress and ensure optimal symptom relief.
Comparative Effectiveness: PUL vs. Other Treatments
The effectiveness of PUL has been evaluated against other BPH treatments, including TURP, laser therapies, and medication.
Prostatic Urethral Lift vs. TURP
TURP has long been considered the gold standard for surgical management of BPH; however, it is more invasive, requires general or spinal anesthesia, and carries a higher risk of complications such as bleeding, infection, and sexual side effects. PUL, by contrast, has a lower complication rate, a quicker recovery, and preserves sexual function but may be less effective in men with very large prostates or median lobe enlargement.
Prostatic Urethral Lift vs. Medications
Medications such as alpha blockers and 5-alpha-reductase inhibitors are often the first line of treatment but may cause side effects (dizziness, fatigue, sexual dysfunction) and may be ineffective in many cases. PUL offers a more definitive and rapid solution for patients who do not respond to or tolerate these drugs.
Patient Experience and Satisfaction
Studies have shown high rates of satisfaction among men who undergo PUL. Improvements in urinary flow, reduction in nocturia, and enhanced quality of life are frequently reported. The low incidence of sexual side effects is a major benefit for many patients.
Long-Term Outcomes
Clinical data indicate that symptom relief and improved urinary function persist for several years following PUL. Some men may require additional treatments or repeat procedures, but the overall rate of reintervention is low.
Limitations and Considerations
Not all patients are candidates for PUL. Men with very large prostates, significant median lobe enlargement, or concomitant prostate cancer may require alternative interventions. It is essential to consult with a urologist to determine the most appropriate treatment based on individual anatomy, symptom severity, and personal preferences.
Nursing Care of Patients Undergoing Prostatic Urethral Lift
Nursing care plays a pivotal role in the perioperative and postoperative management of patients who undergo Prostatic Urethral Lift, ensuring safety, comfort, and optimal outcomes. This document outlines key nursing interventions, patient education strategies, and holistic care considerations for patients receiving PUL.
Preoperative Nursing Considerations
Assessment
- Complete medical history, focusing on urological symptoms, underlying comorbidities (e.g., cardiovascular disease, diabetes), allergies, and medication use (especially anticoagulants and antiplatelets).
- Physical examination, including vital signs and baseline assessment of urinary function (voiding patterns, post-void residual volume, presence of hematuria).
- Laboratory investigations as ordered: urinalysis, renal function tests, coagulation profile.
Patient Preparation
- Educate the patient about the procedure, expected outcomes, risks, and benefits using understandable language and visual aids if available.
- Discuss potential complications: urinary retention, bleeding, discomfort, infection.
- Obtain informed consent and verify completion of preoperative checklist.
- Ensure the patient has followed preoperative instructions, such as fasting or withholding certain medications.
- Provide emotional support to address anxiety or concerns.
Postoperative Nursing Care
Immediate Postoperative Management
- Monitor vital signs and observe for signs of postoperative complications: bleeding, infection, urinary retention.
- Assess pain levels and administer analgesics as prescribed. Non-opioid medications are preferred due to minimal tissue disruption with PUL.
- Check the urinary output: frequency, urgency, dysuria, hematuria, or retention.
- Monitor for hematuria: Mild blood-tinged urine is common initially but should resolve within days.
- Encourage early ambulation to reduce thromboembolic risk and promote recovery.
- Provide instructions on proper perineal hygiene to reduce infection risk.
Catheter Management
- Most patients do not require a postoperative catheter, but if retention occurs, a temporary urinary catheter may be placed.
- Monitor catheter drainage, ensure patency, and maintain aseptic technique during care.
- Educate the patient about signs of catheter-related complications (pain, leakage, infection).
Infection Prevention
- Monitor for fever, chills, dysuria, or suprapubic discomfort.
- Teach the patient to recognize and report symptoms of urinary tract infection (UTI).
- Maintain strict hand hygiene and use appropriate personal protective equipment during all procedures.
- Administer prescribed antibiotics if indicated.
Patient Education and Discharge Planning
Activity and Lifestyle Modifications
- Advise the patient to avoid strenuous activities, heavy lifting, or vigorous exercise for at least one week or as directed by the physician.
- Encourage gentle walking and gradual return to normal activities as tolerated.
- Suggest avoiding sexual intercourse until cleared by the healthcare provider (typically one to two weeks post-procedure).
Medication and Symptom Management
- Review prescribed medications: analgesics, antibiotics, or alpha-blockers if used.
- Explain possible side effects and instruct on proper administration.
- Emphasize adherence and completion of any antibiotic course to prevent infection.
- Teach monitoring of urinary symptoms: frequency, urgency, stream strength, and nocturia.
Signs of Complications
- Educate the patient and family about warning signs: persistent hematuria, inability to void, severe pain, fever, foul-smelling urine.
- Provide clear instructions for when and how to seek medical attention.
- Supply contact information for follow-up and emergency care.
Holistic and Psychosocial Support
- Recognize and address emotional reactions: anxiety, embarrassment, or fear of recurrence.
- Offer access to counselling services or support groups for men with BPH.
- Provide reassurance regarding the minimally invasive nature of PUL and its generally favorable outcomes.
Follow-up and Long-term Care
Outpatient Follow-up
- Schedule follow-up visits to assess symptom improvement, monitor for late complications, and ensure proper implant function.
- Urinalysis and ultrasound may be performed to evaluate bladder emptying and residual urine.
- Review long-term management of BPH symptoms and lifestyle modifications.
Continued Education
- Update patient knowledge as new recommendations or research emerges regarding PUL and BPH management.
- Encourage patients to maintain healthy habits to support urinary tract health: adequate hydration, balanced nutrition, regular physical activity.
REFERENCES
- American Urological Association. Innovations in Treatment of BPH. https://www.urologyhealth.org/healthy-living/care-blog/2018/innovations-in-treatment-of-bph. Updated 2/27/2018.
- Rahman A, Leslie SW, Desai D. Prostatic Urethral Lift. [Updated 2024 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/sites/books/NBK606089/
- Garcia C, Chin P, Rashid P, et al. Prostatic Urethral Lift: A Minimally Invasive Treatment for Benign Prostatic Hyperplasia. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4494639/. Prostate Int. 2015 Mar;3(1):1-5.
- Lerner LB, McVary, KT, Barry MJ et al. Management of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia: AUA Guideline Part I, Initial Work-Up and Medical Management. https://pubmed.ncbi.nlm.nih.gov/34384237/. J Urol. 2021 Aug 13; 206: 806.
- Loloi J, Feiertag N, Gautam K, et al. An Update on the Outcomes of Patients Treated with Urolift for Benign Prostatic Hyperplasia. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8205643/. Res Rep Urol. 2021 Jun 11;13:347-355.
- National Institute of Diabetes and Digestive and Kidney Diseases (U.S.). Prostate Problems. https://www.niddk.nih.gov/health-information/urologic-diseases/prostate-problems. Updated 3/2016.
- Roehmholdt MJ, Bentley DF. Large Pelvic Hematoma after UroLift® Procedure for Treatment of BPH with Median Lobe. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8942674/. Case Rep Urol. 2022 Mar 16;2022:7065865.
- Roehrborn CG, Barkin J, Gange SN, et al. Five Year Results of the Prospective Randomized Controlled Prostatic Urethral L.I.F.T. Study. https://pubmed.ncbi.nlm.nih.gov/28646935/. Can J Urol 2017;24(3):8802-8813.
- The British Association of Urological Surgeons (BAUS). Prostatic Urethral Lift (Urolift®) Implant. https://www.baus.org.uk/_userfiles/pages/files/Patients/Leaflets/Urolift.pdf. Updated 12/2021.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





