Voice feminization surgery is a set of surgical procedures designed to raise the pitch and alter the resonance of the voice, helping transgender women or nonbinary individuals achieve a voice that aligns more closely with their gender identity. It may be performed alone or alongside voice therapy.
Introduction
Voice is an integral aspect of personal identity, affecting how individuals perceive themselves and how they are perceived by others. For many transgender women and gender diverse individuals, voice can be a source of gender dysphoria when it does not align with their gender identity. While voice therapy is often the first step for those seeking a more feminine voice, some may choose voice feminization surgery to achieve the vocal characteristics they desire. This document aims to provide a comprehensive overview of voice feminization surgery, including its techniques, outcomes, risks, and considerations for those contemplating this significant step in their gender-affirming journey.
Understanding Voice and Gender
The human voice is a complex phenomenon shaped by numerous anatomical and physiological factors. Pitch, resonance, intonation, and speech patterns all contribute to a voice being perceived as feminine, masculine, or androgynous. The fundamental frequency, measured in Hertz (Hz), is a key determinant: cisgender female voices typically range from 165 to 255 Hz, while cisgender male voices average between 85 and 155 Hz. However, gender perception involves more than pitch alone. The resonance (how sound vibrates in the throat and oral cavity) and prosody (patterns of rhythm and intonation) also play vital roles.
For transgender women and transfeminine individuals, the desire to feminize their voice is deeply rooted in the quest for authenticity and comfort in social situations. An incongruent voice may lead to misgendering, affecting self-confidence and emotional well-being.
Non-Surgical Approaches: Voice Therapy
Before considering surgery, most individuals pursue voice therapy with a speech-language pathologist (SLP) specializing in transgender voice modification. Voice therapy focuses on modifying pitch, resonance, intonation, and communication style through behavioral techniques and exercises. With consistent practice, many achieve a more feminized voice that aligns with their gender identity.
However, voice therapy has its limitations. Not everyone reaches their desired results, particularly in raising pitch or altering resonance significantly. Some may find that their voice fatigues easily, or they revert to their original patterns under stress. For those who remain dissatisfied after extensive voice training, surgical intervention becomes a consideration.
What Is Voice Feminization Surgery?
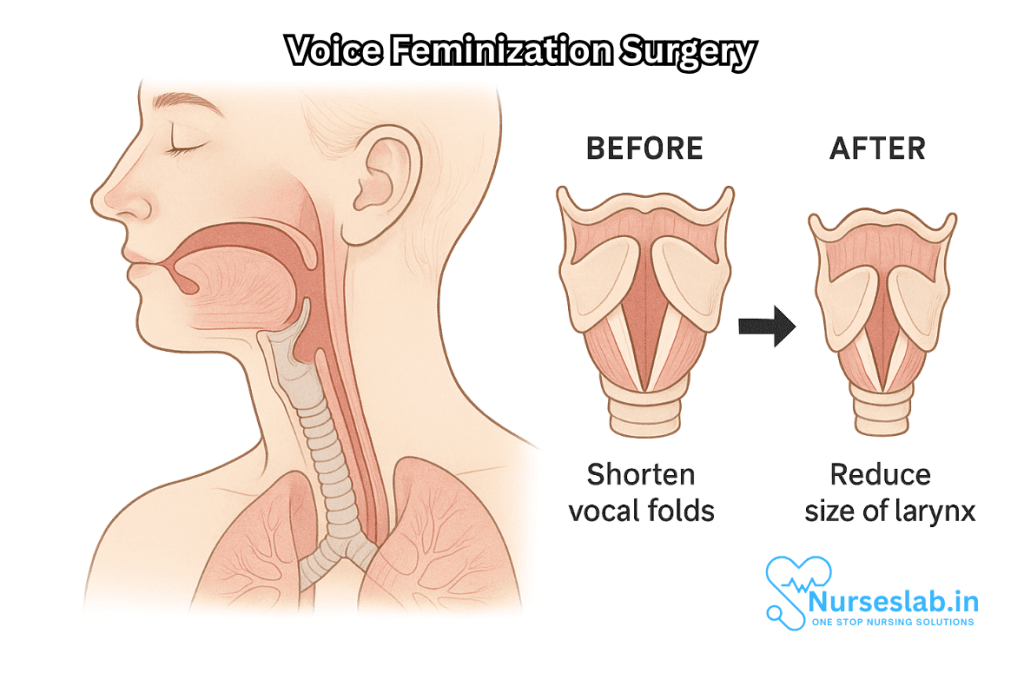
Voice feminization surgery refers to a set of surgical procedures designed to alter the vocal anatomy to produce a higher-pitched, more feminine sounding voice. The main focus is on altering the vocal folds (commonly called vocal cords) to increase their tension and/or reduce their vibrating length, resulting in a higher fundamental frequency. Other procedures may target the resonance structures, such as the vocal tract, or modify the Adam’s apple (thyroid cartilage) for aesthetic purposes.
Who Is a Candidate for Voice Feminization Surgery?
Candidates for voice feminization surgery often include transgender women, transfeminine non-binary individuals, and, in some cases, cisgender women with a naturally low pitch who desire a higher voice. Ideal candidates are those who:
- Have undergone a period of voice therapy and have realistic expectations about surgical outcomes
- Are physically healthy and non-smokers
- Understand the potential risks and benefits
- Are committed to post-surgical voice care and therapy
A thorough evaluation by a multidisciplinary team, including an otolaryngologist (ENT specialist), speech-language pathologist, and sometimes a mental health professional, is essential to determine candidacy.
Types of Voice Feminization Surgery
Several surgical techniques have been developed to feminize the voice. The most commonly performed procedures include:
1. Wendler Glottoplasty
This is currently the most widely used technique for voice feminization. During glottoplasty, the surgeon creates an anterior web by suturing the front portions of the vocal folds together. This shortens the effective length of the folds, resulting in a higher pitch, similar to how shortening a guitar string raises its pitch. The procedure is typically performed endoscopically through the mouth, with no external incisions.
2. Cricothyroid Approximation (CTA)
CTA involves bringing the cricoid and thyroid cartilages closer together, mimicking the action of the cricothyroid muscle, which tenses the vocal folds and raises pitch. This procedure can be performed externally via a small neck incision. However, CTA has largely been supplanted by glottoplasty due to concerns regarding predictability and long-term results.
3. Laser-Assisted Voice Adjustment
Lasers can be used to thin the vocal folds, making them vibrate at a higher frequency, thereby increasing pitch. This technique can be less predictable, and results vary based on individual anatomy and healing response.
4. Chondrolaryngoplasty (“Tracheal Shave”)
While not affecting the voice itself, this procedure reduces the prominence of the thyroid cartilage (Adam’s apple), which is often associated with masculine appearance. It is frequently performed alongside vocal feminization surgery for those seeking aesthetic alignment.
5. Other Experimental or Adjunct Procedures
Some surgeons are investigating additional techniques, such as vocal fold shortening, anterior commissure advancement, or modifications of the laryngeal framework. These are less common and typically reserved for specific anatomical needs.
The Surgical Process: Preparation, Procedure, and Recovery
Preoperative Assessment
Before surgery, patients undergo comprehensive evaluations, which may include:
- Videostroboscopy or laryngoscopy to assess vocal fold health
- Acoustic and perceptual voice analyses
- Review of prior voice therapy progress
- General health screening and counseling on expectations
The Procedure
Most voice feminization surgeries are performed under general anesthesia and take one to two hours. For glottoplasty, the surgeon accesses the vocal folds through the mouth using specialized endoscopic instruments. Delicate sutures are placed to create the anterior web, and care is taken to minimize trauma to surrounding tissues.
Postoperative Recovery
The recovery period is crucial for optimal results. Typical guidelines include:
- Absolute voice rest (no talking, whispering, or throat clearing) for 1-2 weeks after surgery
- Gradual reintroduction of voice under the guidance of a speech-language pathologist
- Avoidance of strenuous activity, smoking, or irritants
- Follow-up examinations to monitor healing and suture placement
Most patients can return to daily activities after a week, but the voice continues to change and settle for several months postoperatively.
Expected Outcomes and Effectiveness
The primary goal of voice feminization surgery is to raise the pitch of the voice into the feminine range. Many patients also report changes in resonance, increased confidence, and reduction in gender dysphoria. Results vary, but studies find that the majority of patients achieve a noticeable and satisfactory increase in pitch.
It is important to note:
- Pitch is typically raised by 30-60 Hz, depending on the procedure and individual anatomy
- Quality and flexibility of the voice may change; some variability is expected
- Not all voices will sound “cisgender female,” and some may retain androgynous qualities
- Ongoing voice therapy is essential to optimize and maintain results
Risks, Complications, and Limitations
As with any surgery, voice feminization procedures carry risks, including:
- Hoarseness, breathiness, or loss of vocal power
- Scar tissue formation on the vocal folds (webbing)
- Difficulty projecting the voice or singing
- Permanent loss of lower vocal range
- Need for revision surgery if results are unsatisfactory
- General surgical risks (infection, anesthesia complications)
Complications are relatively rare when performed by experienced surgeons, but it is vital that candidates understand these possibilities.
Choosing a Surgeon and Facility
Selecting an experienced, board-certified otolaryngologist or laryngeal surgeon with expertise in transgender voice procedures is paramount. Patients are encouraged to:
- Review surgeons’ credentials and before-and-after results
- Seek testimonials from former patients
- Ask about the surgeon’s experience with revision procedures
- Discuss expected outcomes and post-operative care in detail
Some clinics also offer multidisciplinary care, including voice therapy and psychological support, to guide patients through every step.
Cost and Accessibility
Costs for voice feminization surgery vary widely depending on the country, surgeon, and specific procedure. In some regions, public or private health insurance may cover part or all of the cost for medically necessary gender-affirming surgeries. Out-of-pocket expenses can range from several thousand to tens of thousands of dollars. It is important to verify insurance coverage, payment plans, and any financial assistance offered by surgical centers.
Life After Voice Feminization Surgery
The journey does not end with the surgery. Continued voice therapy is essential to reinforce new vocal habits, expand range, and reduce vocal strain. Many patients report increased satisfaction with their social interactions, workplace acceptance, and personal confidence. However, emotional adjustment is a process, and support via counseling, peer groups, or online communities can be invaluable.
Some individuals may grieve the loss of their former voice, particularly if singing or vocal performance was important to them. Open communication with healthcare providers about goals and concerns helps tailor care to each person’s unique needs.
Ethical and Social Considerations
Voice is not the sole determinant of gender identity or authenticity. Not all transgender women or transfeminine individuals desire surgical voice modification, and the decision is deeply personal. Social acceptance, workplace inclusivity, and freedom from discrimination are equally important in supporting gender diversity.
Nursing Care of Patients Undergoing Voice Feminization Surgery
The nursing care associated with voice feminization surgery plays a pivotal role in ensuring safe recovery, optimal surgical outcomes, and strong psychosocial support. This comprehensive guide examines the perioperative nursing care, postoperative considerations, and holistic strategies for supporting patients before, during, and after voice feminization surgery.
Preoperative Nursing Care
Assessment and Education
- Comprehensive Assessment: Gather a detailed medical, surgical, and psychosocial history. Assess the patient’s understanding of the procedure, expectations, and support systems. Screen for comorbidities that may impact surgical risk, such as respiratory or bleeding disorders.
- Voice Therapy History: Confirm completion of preoperative voice therapy, as most surgeons require patients to have already attempted voice modification through non-surgical means.
- Patient Education: Explain the surgical procedure, anticipated outcomes, potential risks, and the importance of postoperative voice rest and ongoing therapy. Discuss realistic expectations regarding pitch increase, vocal quality, and the healing trajectory.
- Psychoeducation: Address fears, anxieties, and misconceptions. Encourage questions and provide culturally sensitive, gender-affirming information.
Preparation and Planning
- Preoperative Instructions: Reinforce fasting guidelines, medication management (such as anticoagulant discontinuation), and preoperative hygiene.
- Coordination: Liaise with the surgical team, speech-language pathologists, and the patient’s support network to ensure continuity of care.
- Consent and Documentation: Verify informed consent and ensure all documentation reflects the patient’s chosen name and pronouns.
Intraoperative Nursing Considerations
- Surgical Site Preparation: Assist with positioning and prepping the neck and laryngeal area according to the surgeon’s preference.
- Infection Control: Employ sterile techniques to minimize infection risk.
- Monitoring: Continuously monitor vital signs and airway patency, as airway management is especially critical in laryngeal surgeries.
- Advocacy: Ensure the surgical team uses the patient’s affirmed name and pronouns, providing a gender-affirming environment.
Immediate Postoperative Nursing Care
Airway and Respiratory Management
- Airway Assessment: Monitor for signs of laryngeal edema, respiratory distress, or airway compromise. Have emergency airway equipment available as needed.
- Oxygen Therapy: Administer supplemental oxygen if required, and monitor oxygen saturation.
- Cough Suppression: Encourage gentle coughing only if necessary, as forceful coughing can disrupt suture lines or surgical alterations.
Pain and Comfort Management
- Pain Assessment: Assess pain using age- and developmentally-appropriate scales. Administer analgesics as prescribed, balancing pain control with the need to avoid medications that may suppress respiration.
- Non-Pharmacological Comfort Measures: Offer ice packs for neck discomfort and promote a calm, quiet environment.
Voice Rest Protocol
- Strict Voice Rest: Enforce absolute voice rest (no speaking, whispering, coughing, or throat clearing) for the initial postoperative period, often ranging from 7 to 14 days, depending on the surgeon’s protocol.
- Communication Alternatives: Provide patients with writing boards, communication apps, or other non-verbal tools to reduce the temptation or need to speak.
- Patient and Family Education: Clearly explain the rationale for voice rest and involve family/support persons in reinforcing compliance.
Nutrition and Hydration
- Diet Advancement: Start with clear liquids, advancing to a soft diet as tolerated. Monitor for swallowing difficulties or aspiration risk.
- Hydration: Encourage adequate fluid intake to keep mucosa moist and promote healing.
Monitoring for Complications
- Hemorrhage: Observe the surgical site for bleeding, swelling, or hematoma formation around the neck and airway.
- Infection: Monitor for fever, local redness, warmth, or purulent drainage and report concerns promptly.
- Laryngeal Injury: Assess for changes in breathing, unusual neck pain, or difficulty swallowing that may suggest nerve or tissue injury.
Ongoing Postoperative and Discharge Care
Gradual Reintroduction of Voice Use
- Speech Therapy: Coordinate with speech-language pathologists for tailored voice therapy, beginning with gentle, supervised vocal exercises once cleared by the surgeon.
- Education: Teach patients about vocal hygiene, such as adequate hydration, avoidance of throat clearing, and strategies to prevent vocal strain.
- Monitoring: Regularly assess vocal quality, pitch, and any signs of vocal fatigue or distress.
Wound and Self-Care Management
- Wound Care: Instruct patients on incision care, signs of infection, and when to seek medical attention.
- Activity Restrictions: Advise on avoiding heavy lifting, straining, or any activities that may increase neck pressure until cleared by the surgeon.
Pain and Symptom Management
- Pain Control: Continue appropriate analgesia and teach patients how to manage mild discomfort at home.
- Addressing Side Effects: Prepare the patient for possible sensations of throat tightness, mild hoarseness, or temporary swallowing changes, all of which typically resolve with healing.
Psychosocial and Emotional Support
- Gender-Affirming Care: Provide respectful, inclusive, and affirming interactions at every phase of care. Use the patient’s affirmed name and pronouns in all communications and documentation.
- Emotional Support: Recognize the profound impact of voice on gender identity and self-confidence. Connect patients with peer support, mental health professionals, and community resources as needed.
- Family and Social Involvement: Encourage supportive involvement from family and chosen community, and provide education about the recovery process and expectations.
Follow-Up and Long-Term Care
- Scheduled Assessments: Arrange follow-up appointments with the surgical team and voice specialists to monitor healing, vocal progress, and to adjust the care plan if necessary.
- Long-Term Outcomes: Track overall satisfaction with voice changes, monitor for late complications such as scarring or granulation tissue, and address any concerns that arise post-surgically.
Patient Education and Empowerment
Nursing care is not only about providing direct clinical support but also about empowering patients with the knowledge and tools to manage their recovery. Key educational topics include:
- What to expect during each phase of recovery
- Signs and symptoms that require immediate medical attention
- Vocal hygiene and techniques to preserve the new voice
- Navigating social interactions and integrating the new voice into daily life
Special Considerations
- Cultural Sensitivity: Recognize the diverse needs and backgrounds of patients seeking voice feminization. Provide care that is free from bias and sensitive to individual gender identities and expressions.
- Accessibility: Ensure that information and resources are accessible to patients of varying literacy and language backgrounds.
- Continuity of Care: Collaborate with multidisciplinary teams—including surgeons, speech therapists, mental health providers, and community advocates—to deliver seamless, patient-centered care.
REFERENCES
- D’haeseleer E, Papeleu T, Leyns C, Adriaansen A, Meerschman I, Tomassen P. Voice Outcome of Glottoplasty. J Voice. Published online February 9, 2023.
- Kim HT. Vocal Feminization: Current Strategies and Patient Perspectives. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7024865/. Int J Gen Med. 2020;13:43-52
- Nuyen BA, Qian ZJ, Campbell RD, Erickson-DiRenzo E, Thomas J, Sung CK. Feminization Laryngoplasty: 17-Year Review on Long-Term Outcomes, Safety, and Technique. https://pubmed.ncbi.nlm.nih.gov/34399638/. Otolaryngol Head Neck Surg. 2022;167(1):112-117.
- Srivastava R. Laryngeal and Voice Surgery. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9398523/. Indian J Plast Surg. 2022;55(2):174-178.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





