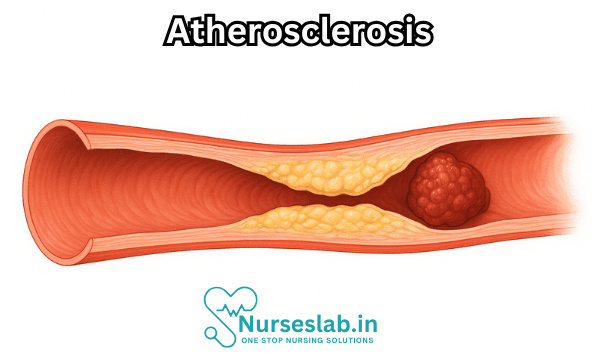
Atherosclerosis, a condition long known to medicine yet still the focus of intense research and clinical attention, is a chronic, progressive disease that affects arteries throughout the body. Characterized by the buildup of plaques—composed of fats, cholesterol, cellular waste products, calcium, and fibrin—within the arterial wall, atherosclerosis narrows and hardens arteries, restricting blood flow and setting the stage for heart attacks, strokes, and a host of other vascular problems.
What is Atherosclerosis?
Atherosclerosis derives from the Greek words “athero,” meaning gruel or paste, and “sclerosis,” meaning hardening. It is the principal cause of cardiovascular diseases—the leading cause of death globally. The disease process begins silently, often decades before symptoms emerge, and can affect any artery in the body, including those supplying the heart (coronary arteries), brain (carotid arteries), limbs (peripheral arteries), and kidneys.
The Pathophysiology of Atherosclerosis
Atherosclerosis is not simply the passive accumulation of lipids in arterial walls but rather a complex, dynamic process involving lipid metabolism, inflammatory responses, and vascular biology. The disease typically progresses through several overlapping stages:
- Endothelial Dysfunction: The innermost lining of arteries, the endothelium, becomes damaged due to factors such as high blood pressure, smoking, diabetes, or elevated cholesterol. This damage compromises the vessel’s barrier function and initiates the disease process.
- Lipid Accumulation: Low-density lipoprotein (LDL) cholesterol infiltrates the damaged endothelium and accumulates within the arterial wall. LDL undergoes oxidation, which provokes local inflammation.
- Inflammation and Immune Response: White blood cells (mainly monocytes and macrophages) are recruited to the site. These cells engulf oxidized LDL, transforming into “foam cells” and forming fatty streaks—the earliest visible sign of atherosclerosis.
- Plaque Formation: Smooth muscle cells migrate from the middle layer of the artery to the intima, proliferate, and produce extracellular matrix, encapsulating the growing mass of lipids and immune cells into a raised plaque.
- Plaque Progression and Complications: Over time, plaques can harden due to calcium deposits and may rupture, triggering blood clot (thrombus) formation. Such events can acutely block arterial flow, leading to heart attack or stroke.
Risk Factors
Atherosclerosis is a multifactorial disease influenced by both modifiable and non-modifiable risk factors.
Non-modifiable Risk Factors
- Age: The risk increases with advancing age.
- Gender: Men are at higher risk than pre-menopausal women, though risk equalizes post-menopause.
- Family History: A family history of cardiovascular disease raises risk.
- Genetics: Certain genetic disorders can predispose individuals to abnormal lipid metabolism.
Modifiable Risk Factors
- High Blood Pressure: Hypertension damages arterial walls, facilitating plaque formation.
- High Cholesterol: Elevated LDL (“bad” cholesterol) and low HDL (“good” cholesterol) levels are key contributors.
- Smoking: Tobacco use accelerates endothelial damage and promotes inflammation.
- Diabetes: High blood sugar damages blood vessels and promotes atherosclerosis.
- Obesity: Excess body fat, particularly abdominal fat, is linked to higher risk.
- Physical Inactivity: Sedentary lifestyle increases susceptibility.
- Diets High in Saturated Fat, Trans Fats, and Simple Sugars: Poor dietary habits contribute to cholesterol buildup.
- Excessive Alcohol Consumption: Can raise blood pressure and contribute to other metabolic disturbances.
- Chronic Stress: May indirectly contribute by worsening other risk factors.
Symptoms and Clinical Manifestations
Atherosclerosis often progresses silently for years or even decades. Symptoms usually become apparent when a significant artery is narrowed or blocked:
- Coronary Arteries: Chest pain (angina), shortness of breath, or heart attack.
- Carotid Arteries: Sudden weakness, confusion, vision problems, or stroke.
- Peripheral Arteries: Leg pain when walking (claudication), numbness, or poor wound healing.
- Renal Arteries: High blood pressure or kidney dysfunction.
Diagnosis of Atherosclerosis
Early diagnosis is crucial but challenging due to the asymptomatic nature of early disease. Diagnostic approaches include:
- Physical Examination: Checking blood pressure, pulses, and looking for signs of arterial narrowing.
- Blood Tests: Measuring cholesterol, blood glucose, and inflammatory markers.
- Imaging Studies:
- Ultrasound (Doppler) for carotid, peripheral, or abdominal arteries
- Coronary angiography or CT angiography to visualize coronary arteries
- Magnetic resonance angiography (MRA)
- Coronary artery calcium scoring
- Electrocardiogram (ECG/EKG): To detect past or ongoing heart attacks.
- Stress Testing: Exercise or pharmacologic tests to assess blood flow during physical exertion.
Complications of Atherosclerosis
When left unchecked, atherosclerosis can lead to life-threatening events, including:
- Myocardial Infarction (Heart Attack): Sudden blockage of coronary arteries by a ruptured plaque or clot.
- Stroke: Interruption of blood supply to the brain due to carotid artery blockage or embolism.
- Peripheral Artery Disease (PAD): Reduced blood flow to limbs, potentially leading to ulcers or gangrene.
- Aneurysm: Abnormal bulging of weakened arterial walls, especially in the aorta, which may rupture.
- Chronic Kidney Disease: Narrowing of renal arteries impairs kidney function.
Treatment and Management
Modern management of atherosclerosis focuses on slowing progression, relieving symptoms, and preventing complications.
Lifestyle Modifications
- Diet: Emphasize whole grains, fruits, vegetables, lean proteins, and healthy fats (e.g., olive oil, nuts). Reduce saturated fat, trans fats, and sugar intake.
- Exercise: At least 150 minutes of moderate-intensity aerobic activity per week.
- Smoking Cessation: Quitting tobacco is one of the most effective interventions.
- Weight Management: Achieve and maintain a healthy body weight.
- Moderate Alcohol Consumption: If consumed, limit to recommended guidelines.
Medications
- Statins: Lower LDL cholesterol and stabilize plaques.
- Antiplatelet Agents: Such as aspirin, to reduce risk of clot formation.
- Blood Pressure Medications: ACE inhibitors, beta-blockers, and others to manage hypertension.
- Diabetes Management: Control of blood glucose levels.
- Other Lipid-Lowering Medications: Ezetimibe, PCSK9 inhibitors, and fibrates.
Procedures and Surgery
- Angioplasty and Stenting: A balloon-tipped catheter opens narrowed arteries, often with stent placement to keep the vessel open.
- Coronary Artery Bypass Grafting (CABG): Bypassing blocked coronary arteries with a vessel from elsewhere in the body.
- Endarterectomy: Surgical removal of plaque from arteries (often carotid arteries).
Prevention
Prevention of atherosclerosis is often more effective than treating established disease. Key preventive strategies include:
- Adopting a heart-healthy diet (rich in fiber, low in saturated and trans fats)
- Regular physical activity
- Avoiding tobacco products
- Maintaining a healthy weight
- Controlling blood pressure, cholesterol, and blood sugar if necessary
- Managing stress
- Regular health checkups for early detection and management of risk factors
REFERENCES
- American Heart Association. Atherosclerosis and Stroke. https://www.stroke.org/en/about-stroke/stroke-risk-factors/atherosclerosis-and-stroke. Last reviewed 10/8/2023.
- Yao BC, Meng LB, Hao ML, Zhang YM, Gong T, Guo ZG. Chronic stress: a critical risk factor for atherosclerosis. J Int Med Res. 2019 Apr;47(4):1429-1440. doi: 10.1177/0300060519826820. Epub 2019 Feb 24. PMID: 30799666; PMCID: PMC6460614.
- American Heart Association. What is Atherosclerosis?. https://www.heart.org/en/health-topics/cholesterol/about-cholesterol/atherosclerosis Last reviewed 11/6/2020.
- Dawson LP, Lum M, Nerleker N, Nicholls SJ, Layland J. Coronary Atherosclerotic Plaque Regression: JACC State-of-the-Art Review. https://pubmed.ncbi.nlm.nih.gov/34991791/. J Am Coll Cardiol. 2022 Jan 4;79(1):66-82.
- Libby P. The changing landscape of atherosclerosis. https://pubmed.ncbi.nlm.nih.gov/33883728/. Nature. 2021 Apr;592(7855):524-533.
- Merck Manual (Consumer Version). Atherosclerosis https://www.merckmanuals.com/home/heart-and-blood-vessel-disorders/atherosclerosis/atherosclerosis. Last revised 9/2022.
- National Heart, Lung, and Blood Institute (U.S.) What Is Atherosclerosis. https://www.nhlbi.nih.gov/health/atherosclerosisLast updated 3/24/2022.
- National Institute of Diabetes and Digestive and Kidney Diseases (U.S.) Renal Artery Stenosis. https://www.niddk.nih.gov/health-information/kidney-disease/renal-artery-stenosis. Last reviewed 7/2014.
- National Library of Medicine (U.S.) Atherosclerosis. https://medlineplus.gov/atherosclerosis.html Last updated 2/8/2021..
- Nayor M, Brown KJ, Vasan RS. The molecular basis of predicting atherosclerotic cardiovascular disease risk. https://pubmed.ncbi.nlm.nih.gov/33476202/. Circ Res. 2021 Jan 22;128(2):287-303.
- Reyes-Soffer G, Ginsberg HN, Berglund L, et al. Lipoprotein(a): A Genetically Determined, Causal, and Prevalent Risk Factor for Atherosclerotic Cardiovascular Disease: A Scientific Statement From the American Heart Association. https://pubmed.ncbi.nlm.nih.gov/34647487/ Arterioscler Thromb Vasc Biol. 2022 Jan;42(1):e48-e60.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





