Calcific tendonitis is a musculoskeletal condition that affects millions of individuals worldwide. Characterized by the accumulation of calcium deposits within the tendons, this disorder most commonly targets the rotator cuff in the shoulder, though it can occur in other tendons throughout the body. The resulting pain and restricted movement can significantly impact daily life, making it essential to understand its origins, presentation, and avenues for effective management.
What is Calcific Tendonitis?
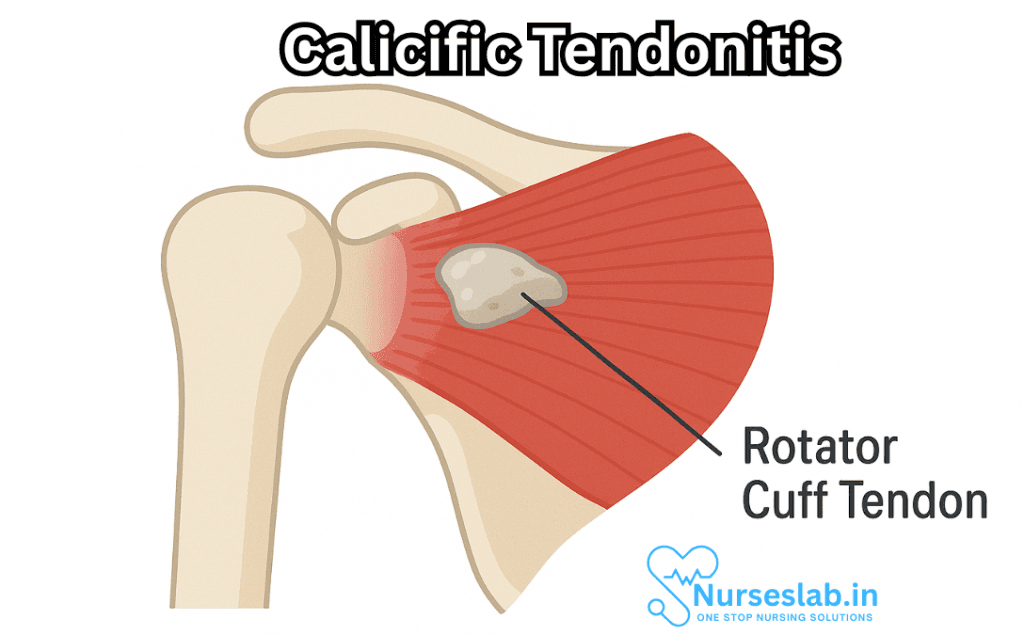
Calcific tendonitis is defined by the pathological deposition of calcium hydroxyapatite crystals within or around tendons. These deposits provoke inflammation and pain, often leading to impaired function. The condition typically affects adults in their 30s to 60s and is more prevalent in women than men. While it is most commonly seen in the shoulder, especially within the supraspinatus tendon of the rotator cuff, other sites such as the hip, elbow, wrist, and knee may also be involved.
Causes and Risk Factors
The exact etiology of calcific tendonitis remains elusive, though several theories have been proposed:
- Degenerative Theory: Suggests that tendon wear and tear over time results in microtrauma, which creates an environment conducive to calcium deposition.
- Cellular Metaplasia: Some researchers believe that local tenocyte (tendon cell) changes lead to the formation of chondrocyte-like cells that promote calcification.
- Genetic and Metabolic Factors: There may be a hereditary predisposition or underlying metabolic disturbance (such as abnormalities in calcium metabolism) that increases susceptibility.
Other risk factors include repetitive overhead activity, diabetes mellitus, thyroid disorders, and certain autoimmune conditions.
Pathophysiology
Calcific tendonitis generally progresses through three stages:
- Pre-calcific Stage: Tendon tissue undergoes transformation, becoming more susceptible to calcium crystal deposition.
- Calcific Stage: Divided into formative and resorptive phases. In the formative phase, calcium deposits accumulate, often without symptoms. The resorptive phase is marked by an influx of inflammatory cells attempting to break down the deposits, which frequently results in acute pain.
- Post-calcific Stage: The body gradually absorbs the calcium, and normal tendon architecture is restored, usually accompanied by symptom relief.
Clinical Presentation
Calcific tendonitis can range from being entirely asymptomatic to severely disabling. The classic symptoms include:
- Pain: Sudden or progressive, typically localized over the affected tendon. In the shoulder, pain may radiate down the arm or worsen with overhead activities.
- Reduced Range of Motion: Stiffness and difficulty moving the joint, especially during the resorptive phase.
- Weakness: Particularly when the rotator cuff is involved, leading to difficulty lifting or rotating the arm.
- Tenderness and Swelling: In some cases, visible swelling or warmth over the affected area may be present.
Diagnosis
A thorough medical history and clinical examination are crucial, but imaging is central to diagnosing calcific tendonitis. The main modalities include:
- X-rays: Readily reveal calcium deposits, especially during the formative and resorptive phases. Deposits appear as opaque areas in the affected tendon.
- Ultrasound: Useful for assessing the size, consistency, and location of deposits, as well as guiding certain interventions like needle aspiration or lavage.
- MRI: May be warranted if there are concerns about tendon tears or other associated conditions, though it is more costly and less sensitive for detecting calcifications than X-ray or ultrasound.
Differential Diagnosis
Several conditions can mimic calcific tendonitis, including:
- Rotator cuff tears
- Tendinopathies of other causes (overuse, trauma)
- Septic arthritis or bursitis
- Frozen shoulder (adhesive capsulitis)
- Osteoarthritis
An accurate diagnosis is key to directing appropriate treatment.
Treatment and Management
Management of calcific tendonitis is tailored to the severity of symptoms, size and location of deposits, and patient preferences. The majority of patients improve with conservative therapy. Treatment options include:
Conservative (Non-Surgical) Management
- Rest and Activity Modification: Avoiding activities that exacerbate symptoms, especially overhead or repetitive movements.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Reduce pain and inflammation.
- Physical Therapy: Exercises to restore range of motion, strength, and function. Modalities such as ultrasound therapy and heat may also provide relief.
- Corticosteroid Injections: For persistent pain unresponsive to oral medications, injections into the affected region can rapidly reduce inflammation.
- Extracorporeal Shock Wave Therapy (ESWT): Uses high-energy sound waves to break up calcium deposits and stimulate healing. Administered over several sessions, ESWT is increasingly supported by clinical research for refractory cases.
- Ultrasound-Guided Needle Lavage (Barbotage): Involves inserting a needle into the calcium deposit under ultrasound guidance to aspirate (remove) the material, sometimes combined with saline irrigation.
Surgical Management
Surgery is reserved for patients with persistent symptoms despite prolonged conservative treatment or for those with large, symptomatic deposits:
- Arthroscopic Removal: Minimally invasive technique where small instruments are inserted through tiny incisions to remove the deposits and, if necessary, repair the tendon.
- Open Surgery: Less commonly performed, reserved for complex or very large deposits.
Post-surgical rehabilitation is crucial for restoring function and minimizing the risk of recurrence.
Prognosis
The outlook for calcific tendonitis is generally favorable. Many individuals experience spontaneous resolution of symptoms as the body gradually dissolves and absorbs the calcium deposits. With appropriate treatment, most regain full function, though recovery can take weeks to months. Recurrence is possible but uncommon.
Some patients may experience chronic pain or shoulder stiffness, underscoring the importance of early intervention and adherence to rehabilitation protocols.
Prevention
While not all cases of calcific tendonitis can be prevented, certain measures may reduce the risk:
- Engage in regular, balanced exercise to maintain tendon flexibility and strength.
- Warm up before physical activity and stretch afterward.
- Avoid repetitive overhead activities or allow adequate rest and recovery.
- Manage underlying health conditions, such as diabetes or thyroid disorders, which may predispose individuals.
- Maintain a healthy diet and weight, supporting overall musculoskeletal health.
Living With Calcific Tendonitis
Coping with calcific tendonitis can be challenging, especially during acute episodes. Strategies for daily management may include:
- Following a prescribed physical therapy regimen and attending all appointments.
- Using ice packs or heat therapy as recommended for pain management.
- Adhering to prescribed medications and promptly reporting any side effects to healthcare providers.
- Seeking support from family, friends, or support groups for encouragement and advice.
Nursing Care of Patients with Calcific Tendonitis
Effective nursing care plays a central role in symptom management, patient education, and rehabilitation. A holistic, patient-centered approach is essential for optimizing outcomes.
Nursing Assessment
Accurate assessment is the cornerstone of effective nursing care. Nurses must take a detailed history and perform a thorough physical examination.
Key Components of Assessment
- Pain Evaluation: Assess intensity, location, duration, and aggravating/relieving factors using standardized pain scales.
- Mobility Assessment: Evaluate the patient’s ability to move the affected limb and perform daily activities.
- Functional Impact: Determine how the condition affects the patient’s work, sleep, and self-care.
- Psychosocial Assessment: Screen for anxiety, frustration, and impact on mental well-being.
- History of Injury or Overuse: Document any repetitive movements or trauma to the affected area.
- Review of Systems: Rule out systemic causes or underlying metabolic conditions.
Diagnostic Investigations
Nurses may be involved in preparing patients for diagnostic imaging such as:
- Plain Radiography (X-ray): Reveals calcium deposits.
- Ultrasound: Assesses size, location, and stage of calcification.
- MRI (if indicated): Evaluates soft tissue involvement.
Nursing Diagnoses
- Acute or chronic pain related to inflammatory process of tendon.
- Impaired physical mobility related to pain and discomfort.
- Disturbed sleep pattern related to pain, especially at night.
- Deficient knowledge regarding disease process and management.
- Risk for anxiety or depression due to functional limitations and persistent pain.
Nursing Interventions
A multifaceted approach is essential for managing calcific tendonitis. Interventions focus on pain relief, improving function, preventing complications, and patient education.
Pain Management
- Administer Medications: Provide NSAIDs as prescribed for pain and inflammation control. Monitor for side effects, especially gastrointestinal upset.
- Cold Therapy: Apply cold packs to the affected area for 15-20 minutes several times a day to reduce pain and inflammation, particularly during acute flare-ups.
- Heat Therapy: After the acute phase, warm compresses may help relieve stiffness and promote circulation.
- Immobilization: Use of a sling or shoulder immobilizer may be recommended for short durations, but prolonged immobilization should be avoided to prevent stiffness.
- Comfort Measures: Encourage the use of pillows or positioning aids during sleep to enhance comfort, especially at night when pain may worsen.
Enhancing Mobility and Function
- Gentle Range-of-Motion Exercises: Collaborate with physiotherapists to introduce passive and active exercises as tolerated, preventing contractures and maintaining flexibility.
- Occupational Therapy Referral: Facilitate adaptive techniques and assistive devices for activities of daily living if required.
- Education on Activity Modification: Instruct patients to avoid high-impact or repetitive overhead activities during recovery. Guide on safe ways to perform necessary tasks.
- Gradual Increase in Activity: Encourage graded return to activities based on pain tolerance and function.
Patient Education
Informing patients about their condition and involving them in decision-making is crucial for adherence and recovery.
- Explain Disease Process: Use simple language to describe calcific tendonitis, its phases, and expected outcomes.
- Discuss Treatment Options: Include conservative measures, possible interventions (e.g., ultrasound-guided needling, shockwave therapy, or surgery), and expected timelines for improvement.
- Teach Self-care Strategies: Demonstrate proper application of cold/heat, safe exercises, and pain monitoring.
- Medication Education: Review indications, dosages, side effects, and importance of adherence for each prescribed medication.
- Encourage Questions: Create an open environment for patients to express concerns or ask questions.
Preventing Complications
- Monitor for Adverse Reactions: Stay vigilant for potential complications from medications (e.g., NSAIDs-induced gastritis or renal impairment).
- Prevent Joint Stiffness: Stress the importance of continued gentle movement within pain limits.
- Fall Prevention: Educate on home safety if mobility is compromised to reduce the risk of falls.
- Skin Integrity: Examine for redness or skin breakdown under slings or splints, particularly in older adults.
Psychosocial and Emotional Support
Living with chronic pain or functional impairment can take a toll on mental health.
- Active Listening: Offer empathetic support and validate patients’ experiences of pain and frustration.
- Emotional Support: Involve family and support networks in care planning when appropriate.
- Refer to Counseling: Suggest mental health resources if anxiety, depression, or adjustment difficulties are identified.
Collaboration with the Health Care Team
Nurses should maintain open communication and collaboration with the multidisciplinary health care team, including:
- Physicians for ongoing medical management and evaluation of treatment response.
- Physical and occupational therapists for rehabilitation planning and progression of mobility exercises.
- Pharmacists for medication review and patient counseling.
- Mental health professionals for psychological support as needed.
Discharge Planning and Continuity of Care
Preparing for discharge and ensuring continuity of care are essential, especially if the patient has had an intervention or has limited mobility.
- Assessment of Home Environment: Identify potential barriers to physical activity or safety hazards.
- Provision of Educational Materials: Supply written instructions for self-management, exercises, and medication use.
- Scheduling Follow-Up: Ensure timely follow-up appointments with relevant providers to monitor progress.
- Community Resources: Inform about support groups or community physical therapy services.
Patient Outcomes and Evaluation
Nursing care should be evaluated regularly to ensure that:
- Pain levels are reduced and manageable.
- Mobility and function are improving progressively.
- Patient demonstrates understanding of disease and self-care strategies.
- No complications (e.g., medication side effects, falls, contractures) are developing.
- The patient’s psychological well-being is maintained or improved.
Special Considerations
Some patients may require additional considerations:
- Elderly Patients: Monitor closely for medication side effects, and pay extra attention to mobility and fall risks.
- Patients with Co-morbidities: Collaborate with the health care team for integrated care, especially in cases of diabetes, renal impairment, or cardiovascular disease.
- Pediatric Patients: Though rare, adapt education and intervention appropriately for age and developmental stage.
REFERENCES
- Wainner R, Hasz M. Management of acute calcific tendinitis of the shoulder. Journal of Orthopaedic & Sports Physical Therapy [serial online]. March 1998;27(3):231-237.
- Kachewar SG, Kulkarni DS. Calcific tendinitis of the rotator cuff: a review. Journal of Clinical and Diagnostic Research. 2013 Jul;7(7):1482-5.
- Kim MS, Kim IW, Lee S, Shin SJ. Diagnosis and treatment of calcific tendinitis of the shoulder. Clin Shoulder Elb. 2020 Nov 27;23(4):210-216. doi: 10.5397/cise.2020.00318. https://pmc.ncbi.nlm.nih.gov/articles/PMC7726362/
- Farin PU, Räsänen H, Jaroma H, Harju A. Rotator cuff calcifications: treatment with ultrasound-guided percutaneous needle aspiration and lavage. Skeletal Radiol. 1996 Aug;25(6):551-4.
- Zhang H, Wang Y, Yang J, Zhao Z, Zhang W, Liu X. Ultrasound-guided needling combined with high- or low-energy extracorporeal shock wave therapy versus needling alone for calcified rotator cuff: a retrospective study. Orthop J Sports Med. 2024;12(11):23259671241275078. doi:10.1177/23259671241275078
- Darrieutort-Laffite C, Blanchard F, Le Goff B. Calcific tendonitis of the rotator cuff: From formation to resorption. Joint Bone Spine. 2018 Dec;85(6):687-692.
- Merolla G, Singh S, Paladini P, Porcellini G. Calcific tendinitis of the rotator cuff: state of the art in diagnosis and treatment. J Orthop Traumatol. 2016;17(1):7-14. doi:10.1007/s10195-015-0367-6
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





