Introduction
Carcinoma is a word that often brings a chill to the heart—a term synonymous with cancer, yet distinct in meaning. It is not merely a medical diagnosis, but a profound turning point in the lives of millions every year. To understand carcinoma is to embark upon a journey into the intricate world of cellular biology, genetics, environmental factors, and the complexities of modern medicine.
Understanding carcinoma is essential for both patients and healthcare providers alike.
What is Carcinoma?
Various factors contribute to the risk of developing carcinoma.
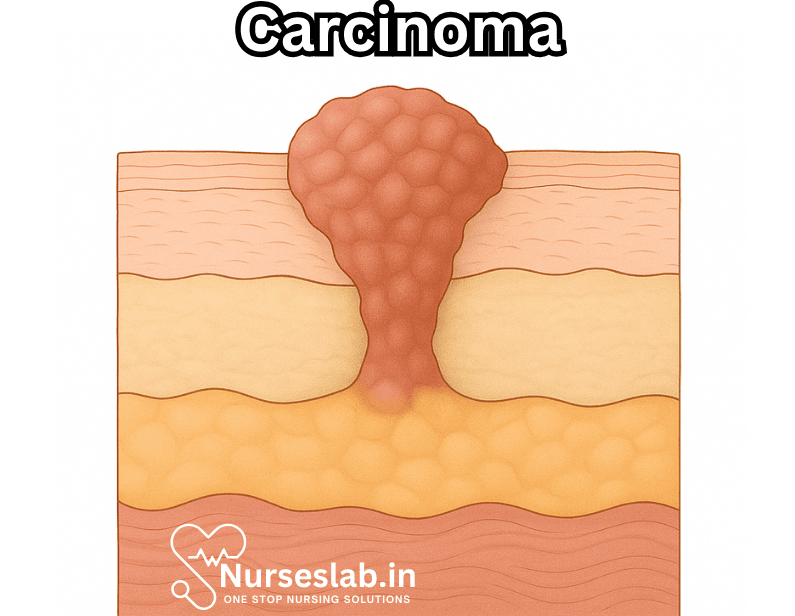
Carcinoma is a type of cancer that begins in epithelial cells—the cells that line the inside and outside surfaces of the body. Epithelial tissues cover the skin, line internal organs and glands, and form the outer layer of many body structures. When these cells undergo malignant transformation, dividing uncontrollably and invading surrounding tissues, the condition is classified as carcinoma.
Distinguishing Carcinoma from Other Cancers
Cancer is a broad term describing uncontrolled cell growth. Carcinoma is just one category, albeit the most common. Other types include:
- Sarcoma: Arises from connective tissues such as bone, muscle, or fat.
- Leukemia: Originates in blood-forming tissues like the bone marrow.
- Lymphoma: Develops from lymphatic cells or tissues.
- Myeloma: Starts in plasma cells of the immune system.
Carcinomas constitute approximately 80-90% of all cancer diagnoses.
Types of Carcinoma
Carcinoma is an umbrella under which several distinct subtypes reside, each with unique characteristics and clinical implications.
Carcinoma can manifest in various forms and requires specific treatment approaches.
Each subtype of carcinoma presents unique challenges for diagnosis and treatment.
1. Adenocarcinoma
Adenocarcinoma arises from glandular epithelial cells. It frequently affects organs such as the lungs, colon, breast, prostate, and pancreas. For instance, most colorectal cancers and a significant proportion of lung cancers are adenocarcinomas.
2. Squamous Cell Carcinoma
Squamous cell carcinoma originates in squamous epithelial cells, which are flat cells found in areas like the skin, mouth, esophagus, and cervix. This type is particularly common in skin cancer and head and neck cancers.
3. Basal Cell Carcinoma
Basal cell carcinoma is the most prevalent form of skin cancer, arising from the basal cells in the epidermis. It is typically slow-growing and rarely metastasizes but can cause significant local tissue destruction.
4. Transitional Cell Carcinoma
This type starts in the transitional epithelium, which lines parts of the urinary tract such as the bladder, ureters, and renal pelvis. Bladder cancer often manifests as transitional cell carcinoma.
5. Other Rare Variants
There are additional, less common forms such as adenosquamous carcinoma (combining features of adenocarcinoma and squamous cell carcinoma), small cell carcinoma (notably in the lung and other organs), and large cell carcinoma.
Causes and Risk Factors
Carcinoma develops from a confluence of genetic, environmental, and lifestyle factors.
Genetic Mutations
Cancerous transformation typically begins with mutations in genes that regulate cell growth and division. These mutations may arise spontaneously or be inherited. Oncogenes (genes promoting cell growth) and tumor suppressor genes (genes inhibiting cell growth) play central roles.
Environmental and Lifestyle Factors
- Tobacco Use: A leading cause, particularly for lung, oral, and esophageal carcinomas.
- UV Radiation: Responsible for most skin carcinomas.
- Chronic Inflammation: Persistent irritation or inflammation can lead to carcinogenic changes.
- Diet and Obesity: Linked to gastrointestinal, breast, and other carcinomas.
- Exposure to Carcinogens: Chemicals such as asbestos, benzene, and formaldehyde raise risk.
- Viruses: Human papillomavirus (HPV) is implicated in cervical carcinoma; hepatitis B and C in liver carcinoma.
Age and Gender
The risk of carcinoma increases with age, as genetic mutations accumulate over time. Some carcinomas, such as breast and prostate cancer, show strong gender predilections.
Symptoms and Clinical Presentation
Symptoms vary widely depending on the organ involved, size, and stage of the carcinoma.
- Skin Carcinomas: Persistent sores, new growths, or changes in existing moles.
- Lung Carcinoma: Cough, hemoptysis (coughing up blood), chest pain, or unexplained weight loss.
- Colon Carcinoma: Changes in bowel habits, blood in stool, abdominal pain.
- Breast Carcinoma: Lump in breast, changes in shape, skin dimpling, nipple discharge.
- Bladder Carcinoma: Blood in urine, frequent urination, pain during urination.
Early carcinomas may be asymptomatic and detected only through screening.
Diagnosis
Timely and accurate diagnosis is crucial for effective management.
Screening and Imaging
Techniques such as mammography, colonoscopy, low-dose CT scans, and Pap smears enable early detection, especially in high-risk populations.
Biopsy
Definitive diagnosis requires histological examination of tissue. A biopsy allows pathologists to assess cellular morphology, grade, and stage the carcinoma.
Molecular Testing
Modern oncology increasingly relies on molecular profiling to identify genetic mutations, guide targeted therapies, and predict prognosis.
Staging and Grading
Staging determines the extent of disease spread, whereas grading assesses how abnormal the cancer cells appear.

- Stage 0: Cancer hasn’t spread beyond where it formed. Stage 0 cancer is in situ and is often curable with prompt treatment.
- Stage 1: The tumor is more pronounced than in stage 0. Cancer hasn’t spread to nearby tissues, organs or lymph nodes.
- Stage 2: The tumor is bigger than in stage 1 and may or may not have spread to your lymph nodes.
- Stage 3: The tumor is larger and has spread to nearby tissues or lymph nodes.
- Stage 4: The cancer is metastatic, which means it’s spread to other organs or parts of your body.
Staging is usually done with the TNM system (Tumor, Node, Metastasis).
Treatment Strategies
Carcinoma treatment requires a multidisciplinary approach and is tailored to the individual.
Surgery
Surgical removal is often the first-line treatment for localized carcinomas. Advances in minimally invasive techniques have improved outcomes and reduced recovery times.
Radiation Therapy
Radiation employs high-energy beams to target and destroy malignant cells. It is often used for tumors that are not amenable to surgery or as an adjunct to other treatments.
Chemotherapy
Chemotherapy uses cytotoxic drugs to kill rapidly dividing cells. Side effects can be significant, including fatigue, nausea, immunosuppression, and hair loss.
Targeted Therapy
Newer drugs target specific molecular pathways involved in cancer growth, with fewer side effects than traditional chemotherapy. Examples include tyrosine kinase inhibitors and monoclonal antibodies.
Immunotherapy
Immunotherapy harnesses the body’s own immune system to combat cancer. Immune checkpoint inhibitors and CAR-T cell therapy have revolutionized treatment for certain carcinomas.
Palliative Care
For advanced or incurable carcinoma, palliative care focuses on symptom relief and improving quality of life.
Prognosis and Survival
Prognosis depends on the type, stage, grade, and molecular makeup of the carcinoma, as well as the patient’s overall health. Early-stage carcinomas are often curable; advanced disease requires complex management.
Prevention
Prevention strategies center around reducing modifiable risk factors.
- Avoid tobacco and excessive alcohol consumption.
- Protect skin from excessive sun exposure.
- Adopt a healthy diet and maintain a healthy weight.
- Undergo recommended cancer screenings.
- Vaccinate against oncogenic viruses (e.g., HPV, hepatitis B).
Living with Carcinoma
A diagnosis of carcinoma is life-altering, but advances in medicine have transformed many forms of the disease into manageable, and sometimes curable, conditions. Support from healthcare professionals, family, and cancer advocacy organizations is critical for psychological and emotional well-being.
Nursing Care of Patients with Carcinoma
Nursing care plays a pivotal role in the management of carcinoma, encompassing not only physical care but also emotional, psychosocial, and educational support. This document provides a comprehensive overview of the nursing care required for patients diagnosed with carcinoma, addressing assessment, planning, implementation, and evaluation.
Assessment of the Patient with Carcinoma
Physical Assessment
- Conduct a thorough head-to-toe assessment, focusing on the primary site of carcinoma and possible metastasis.
- Monitor vital signs, noting any abnormalities such as fever, tachycardia, or hypotension.
- Assess for symptoms such as pain, weight loss, fatigue, nausea, vomiting, anorexia, dyspnea, cough, hematuria, or bleeding, depending on the cancer type.
- Observe for signs of infection, especially in immunocompromised patients due to chemotherapy or radiotherapy.
- Evaluate nutritional status, including body weight, appetite, and signs of malnutrition.
- Assess skin integrity, particularly for patients at risk of pressure ulcers or those undergoing radiotherapy.
Psychosocial and Emotional Assessment
- Evaluate the patient’s understanding of the diagnosis, prognosis, and treatment plan.
- Assess emotional responses such as fear, anxiety, depression, anger, or grief.
- Identify coping mechanisms and support systems, including family, friends, and community resources.
- Screen for signs of psychological distress or risk of suicide.
Functional and Environmental Assessment
- Determine the patient’s ability to perform activities of daily living (ADLs) and any limitations resulting from the disease or treatment.
- Assess the home environment for safety, accessibility, and resources to support home care if needed.
Planning Nursing Care
Setting Priorities
Understanding the prognosis for carcinoma is vital for informed decision-making.
- Prioritize symptom management, especially pain and discomfort.
- Focus on preventing complications such as infection, bleeding, and nutritional deficits.
- Address psychosocial and emotional needs, ensuring the patient feels supported and informed.
- Plan for continuity of care from hospital to home or community settings.
Establishing Goals
- Relieve pain and other distressing symptoms.
- Promote optimal nutrition and hydration.
- Prevent and promptly treat complications.
- Enhance patient education and self-care abilities.
- Provide emotional support and counseling.
- Facilitate communication between the patient, family, and healthcare team.
Implementation of Nursing Interventions
Pain Management
- Assess pain regularly using appropriate scales (e.g., numeric, visual analog).
- Administer prescribed analgesics, including non-opioid, opioid, and adjuvant medications as necessary.
- Utilize non-pharmacological approaches such as relaxation techniques, guided imagery, massage, and heat/cold therapy.
- Monitor for side effects of pain medications and advocate for adjustments as needed.
Management of Treatment Side Effects
- Monitor for and manage side effects of chemotherapy, such as nausea, vomiting, mucositis, alopecia, myelosuppression, and neuropathy.
- Support patients undergoing radiotherapy by providing skin care instructions and managing fatigue or localized symptoms.
- Educate patients about possible side effects and self-management strategies.
Infection Prevention
The emotional impact of a carcinoma diagnosis can be profound, affecting patients and families.
- Implement strict hand hygiene and aseptic techniques.
- Monitor for early signs of infection (fever, redness, swelling, malaise).
- Educate patients and families on infection prevention, including avoiding crowds and monitoring for symptoms.
- Administer prophylactic antibiotics or growth factors if prescribed.
Nutritional Support
- Assess dietary intake and preferences.
- Collaborate with dietitians to develop individualized meal plans.
- Encourage small, frequent meals high in calories and protein.
- Monitor for signs of malnutrition, dehydration, or swallowing difficulties.
- Provide oral care to reduce the risk of mucositis and promote appetite.
Prevention of Complications
- Monitor for anemia, bleeding, and thrombocytopenia, especially in patients receiving chemotherapy.
- Educate about signs of bleeding and interventions to reduce risk (e.g., avoiding sharp objects, using soft toothbrushes).
- Implement fall prevention strategies for weak or debilitated patients.
- Promote mobility and prevent deep vein thrombosis through exercises and ambulation as tolerated.
Psychosocial Care and Counseling
- Provide emotional support through active listening, empathy, and reassurance.
- Refer to counseling services, social workers, or support groups as needed.
- Engage family in care planning and encourage open communication.
- Respect cultural, spiritual, and personal values in planning and delivery of care.
Patient Education
- Educate about the disease process, expected treatment outcomes, and potential complications.
- Teach self-care practices, such as mouth care, infection prevention, and medication management.
- Ensure the patient and family are aware of when to seek medical attention for new or worsening symptoms.
- Provide written materials and resources for further information.
Evaluation of Nursing Care
- Regularly assess progress toward goals and adjust the care plan as needed.
- Evaluate pain control, nutritional status, emotional well-being, and prevention of complications.
- Solicit feedback from the patient and family to ensure satisfaction and address unmet needs.
- Document all interventions and responses comprehensively.
Special Considerations
Palliative and End-of-Life Care
- For patients with advanced carcinoma, focus shifts to comfort, dignity, and quality of life.
- Manage symptoms aggressively, including pain, dyspnea, anxiety, and constipation.
- Facilitate discussions about goals of care, advance directives, and end-of-life wishes.
- Support the family throughout the dying process and provide bereavement resources.
Ethical and Legal Considerations
- Respect patient autonomy and informed consent at every stage of care.
- Safeguard patient confidentiality.
- Advocate for the patient’s rights and best interests.
Collaboration with the Interdisciplinary Team
- Nurses work closely with physicians, oncologists, pharmacists, dietitians, social workers, and rehabilitation specialists.
- Regular team meetings and communication are essential for coordinated, holistic care.
REFERENCES
- Basset-Seguin N, Herms F. Update in the management of basal cell carcinoma.. https://pubmed.ncbi.nlm.nih.gov/32346750/ Acta Derm Venereol. 2020;100(11):adv00140.
- Bengtsson A, Andersson R, Ansari D. The actual 5-year survivors of pancreatic ductal adenocarcinoma based on real-world data. Sci Rep. 2020;10(1):1-9. doi:10.1038/s41598-020-73525-y
- Kuhn E, Morbini P, Cancellieri A, Damiani S, Cavazza A, Comin CE. Adenocarcinoma classification: patterns and prognosis.. https://pubmed.ncbi.nlm.nih.gov/30259909/ Pathologica. 2018;110(1):5-11.
- Infante M, Berghmans T, Heuvelmans MA, Hillerdal G, Oudkerk M. Slow-growing lung cancer as an emerging entity: from screening to clinical management. Eur Respir J. 2013;42(6):1706-22. doi:10.1183/09031936.00186212
- National Cancer Institute. SEER Training Modules. Cancer Classification.. https://training.seer.cancer.gov/disease/categories/classification.html
- Fiala C, Diamandis EP. Mutations in normal tissues-some diagnostic and clinical implications. BMC Med. 2020;18(1):283. doi:10.1186/s12916-020-01763-y
- Parikh U, Chhor CM, Mercado CL. Ductal carcinoma in situ: the whole truth.. https://pubmed.ncbi.nlm.nih.gov/29045181/ AJR Am J Roentgenol. 2018;210(2):246-255.
- Que SKT, Zwald FO, Schmults CD. Cutaneous squamous cell carcinoma: incidence, risk factors, diagnosis, and staging.. https://pubmed.ncbi.nlm.nih.gov/29332704/ J Am Acad Dermatol. 2018;78(2):237-247.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.
Palliative care for carcinoma patients focuses on enhancing quality of life.
Collaborative care teams are essential for managing complex cases of carcinoma.
Awareness and education about carcinoma can lead to better outcomes for patients.





