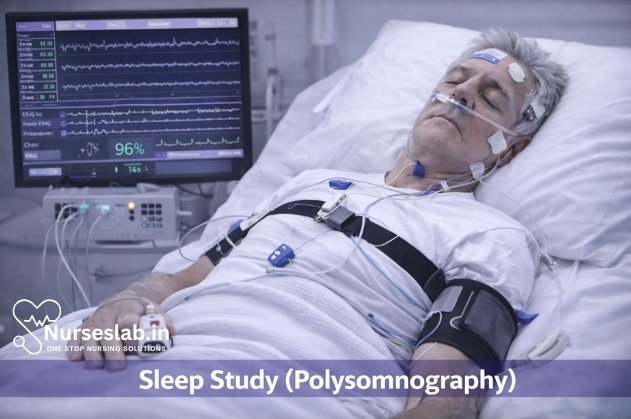
A sleep study, or polysomnography, is an overnight test that monitors brain activity, breathing patterns, oxygen levels, and body movements. It helps diagnose sleep apnea, insomnia, narcolepsy, and other sleep disorders, supporting accurate treatment planning.
Introduction
Sleep is a fundamental physiological process essential for health and well-being. Disruptions in sleep can lead to significant medical, psychological, and social consequences. In clinical practice, the accurate diagnosis of sleep disorders is crucial, and polysomnography—commonly known as a sleep study—serves as the gold standard diagnostic tool.
Definition and Purpose of Polysomnography
Polysomnography is a multi-parametric overnight test that records various physiological parameters during sleep. The term “polysomnography” derives from the Greek ‘poly’ (many), ‘somno’ (sleep), and ‘graphy’ (recording). It is designed to monitor and document brain activity, eye movements, muscle tone, heart rhythm, respiratory effort, airflow, oxygen saturation, and other variables as a patient sleeps.
The primary purpose of polysomnography is to diagnose and characterise sleep disorders such as obstructive sleep apnoea (OSA), central sleep apnoea, periodic limb movement disorder, narcolepsy, REM sleep behaviour disorder, and other parasomnias.
Polysomnography is typically conducted in a specialised sleep laboratory, though advances in technology now allow for home-based studies in selected patients. The test provides objective data regarding the architecture and quality of sleep, enabling clinicians to tailor treatment strategies and improve patient outcomes.
Indications for Polysomnography
Polysomnography is indicated in a wide range of clinical scenarios where sleep disorders are suspected. Common reasons for ordering a sleep study include:
- Obstructive Sleep Apnoea (OSA): Characterised by repetitive episodes of upper airway obstruction during sleep, resulting in fragmented sleep and oxygen desaturation.
- Central Sleep Apnoea: Marked by cessation of respiratory effort due to central nervous system dysfunction.
- Periodic Limb Movement Disorder (PLMD): Involves involuntary repetitive movements of the limbs during sleep, leading to arousals and disturbed sleep.
- Insomnia: Particularly when secondary causes or underlying sleep disorders are suspected.
- Narcolepsy: A disorder marked by excessive daytime sleepiness, cataplexy, and abnormal REM sleep phenomena.
- REM Sleep Behaviour Disorder: Manifested by abnormal movements or behaviours during REM sleep.
- Parasomnias: Such as sleepwalking, night terrors, and other abnormal sleep behaviours.
- Unexplained Daytime Sleepiness: Where the cause is unclear after initial evaluation.
- Assessment of Sleep Quality: In patients with chronic medical conditions, psychiatric illnesses, or unexplained fatigue.
Preparation for Polysomnography
Proper preparation is essential to ensure accurate and reliable results. Patients are typically advised on the following:
- Pre-Test Instructions: Avoid caffeine, alcohol, and sedative medications for at least 24 hours prior to the study unless prescribed by the physician.
- Sleep Hygiene: Maintain a regular sleep-wake schedule for several days before the test.
- Medication Review: Inform the sleep laboratory about all current medications, as certain drugs can affect sleep architecture and test results.
- Personal Comfort: Bring comfortable nightwear and personal items to the sleep laboratory to facilitate restful sleep.
- Fasting: Fasting is generally not required, but heavy meals should be avoided before the test.
- Arriving Early: Arrive at the sleep centre well before the scheduled time to allow adequate time for electrode placement and acclimatisation.
In paediatric patients, parental presence may be permitted to reduce anxiety. Patients should be advised about the overnight nature of the study and the presence of monitoring equipment.
Procedure Steps:
Polysomnography is typically performed overnight in a controlled environment. The following steps outline the procedure:
- Patient Admission and Consent: Upon arrival, the patient is briefed on the procedure and informed consent is obtained.
- Electrode and Sensor Placement: Multiple electrodes and sensors are attached to the patient’s scalp (for EEG), face (for EOG), chin and legs (for EMG), chest (for ECG), and body (for respiratory effort and movement).
- Baseline Measurements: Pre-sleep baseline readings are recorded to ensure proper functioning of equipment.
- Initiation of Monitoring: The patient is encouraged to sleep naturally while continuous monitoring is conducted throughout the night.
- Real-Time Observation: Technicians observe the patient via video and audio feeds to document behavioural events and ensure safety.
- Data Collection: Physiological data are continuously collected and stored for later analysis.
- Awakening and Equipment Removal: After a minimum of six hours, the patient is awakened, and all electrodes and sensors are removed.
- Post-Test Debriefing: The patient is provided with initial feedback and post-study instructions.
The entire procedure is non-invasive and generally well-tolerated, though some patients may experience minor discomfort due to electrode placement.
Monitoring Parameters in Polysomnography
Polysomnography is distinguished by its ability to simultaneously record multiple physiological variables. The major parameters monitored include:
- Electroencephalogram (EEG): Measures brain wave activity to determine sleep stages (NREM and REM).
- Electrooculogram (EOG): Captures eye movements, crucial for identifying REM sleep.
- Electromyogram (EMG): Records muscle tone, particularly in the chin and limbs, to differentiate sleep stages and detect movement disorders.
- Electrocardiogram (ECG): Assesses heart rate and rhythm during sleep.
- Respiratory Effort and Airflow: Sensors on the chest and abdomen monitor breathing effort; nasal and oral airflow sensors detect apnoeic episodes.
- Pulse Oximetry: Monitors oxygen saturation, identifying hypoxaemic events.
- Body Position and Movement: Sensors track changes in position and detect abnormal movements.
- Snoring Microphone: Records snoring sounds as part of the assessment for sleep-disordered breathing.
These parameters collectively allow for comprehensive evaluation of sleep architecture, breathing patterns, cardiac function, and motor activity during sleep.
Interpretation of Results
Interpretation of polysomnography requires specialised training in sleep medicine. The recorded data are reviewed by a sleep specialist, who analyses the following:
- Sleep Architecture: Distribution of NREM and REM sleep, sleep latency, total sleep time, and sleep efficiency.
- Respiratory Events: Frequency and severity of apnoeas, hypopnoeas, and desaturation episodes.
- Movement Disorders: Presence of periodic limb movements, arousals, and REM sleep behaviour events.
- Cardiac Events: Arrhythmias or abnormal heart rate patterns during sleep.
- Other Abnormalities: Paroxysmal events, parasomnias, or unexplained arousals.
Results are typically summarised in a detailed report, including graphical representations (hypnogram, event summary) and quantitative indices such as the Apnoea-Hypopnoea Index (AHI), Oxygen Desaturation Index (ODI), and Periodic Limb Movement Index (PLMI). These findings guide the diagnosis and management of sleep disorders.
Risks and Benefits of Polysomnography
Risks
- Minimal Physical Risks: Polysomnography is non-invasive; risks are limited to minor skin irritation from electrode adhesive or transient discomfort from sensor placement.
- Sleep Disruption: Some patients may experience difficulty sleeping in a laboratory environment, potentially affecting results.
- Rare Complications: Very rarely, patients may develop allergic reactions to adhesives or experience anxiety due to unfamiliar surroundings.
Benefits
- Accurate Diagnosis: Polysomnography provides objective, multi-dimensional data essential for diagnosing complex sleep disorders.
- Tailored Treatment: Results enable clinicians to customise therapy, improving patient outcomes and quality of life.
- Non-Invasive Nature: The procedure is safe and well-tolerated across age groups, including children and elderly patients.
- Comprehensive Assessment: Simultaneous monitoring of multiple parameters allows for holistic evaluation of sleep health.
The benefits of polysomnography far outweigh its minimal risks, making it the preferred diagnostic modality for sleep-related conditions.
Nursing Care for Patients Undergoing Sleep Study (Polysomnography)
The procedure involves the simultaneous recording of multiple physiological parameters during sleep, including brain waves, oxygen levels, heart rate, breathing, and eye and leg movements. The role of the nurse in the care of patients undergoing polysomnography is critical to ensuring patient safety, comfort, and the accuracy of diagnostic results.
Pre-Procedure Nursing Care
1. Patient Assessment and Preparation
Effective nursing care begins with a thorough assessment of the patient’s medical history, current medications, allergies, and sleep patterns. Nurses should inquire about previous sleep studies, existing sleep disorders, and relevant comorbidities such as cardiovascular, respiratory, or neurological conditions. The following steps are essential in preparing the patient for polysomnography:
- Education and Counseling: Inform the patient about the purpose, process, and expected outcomes of the sleep study. Address any fears or misconceptions, and provide written instructions if necessary.
- Medication Review: Assess all medications, including over-the-counter and herbal supplements, as some substances may affect sleep architecture or interfere with test results. Collaborate with the healthcare provider regarding temporary discontinuation or adjustment of certain drugs if indicated.
- Pre-Procedure Instructions: Advise the patient to avoid caffeine, alcohol, and heavy meals on the day of the study. Instruct them to maintain their usual sleep-wake schedule and bring comfortable sleepwear, personal hygiene items, and any necessary medical devices (e.g., CPAP machine).
- Skin Preparation: Explain the need for clean, dry skin to facilitate electrode adhesion. Ask the patient to shower before arrival and avoid using lotions, oils, or makeup on the face and scalp.
- Allergy and Sensitivity Assessment: Check for allergies to adhesives, electrode gels, or latex, and make appropriate accommodations to prevent skin reactions.
2. Environment Preparation
The sleep lab environment should be quiet, comfortable, and conducive to sleep. Nurses are responsible for ensuring that the room temperature is appropriate, lighting is adjustable, and noise levels are minimized. All equipment, including polysomnograph machines, electrodes, sensors, and monitoring devices, should be checked for functionality and cleanliness prior to patient arrival.
3. Documentation and Consent
Obtain informed consent from the patient or legal guardian, explaining the risks, benefits, and alternatives to the procedure. Document all relevant medical information, allergies, and patient preferences in the nursing record. Ensure that the sleep study requisition is complete and includes clear instructions from the referring physician.
Intra-Procedure Nursing Care
1. Patient Arrival and Settling In
Upon arrival, greet the patient warmly and verify their identity using two identifiers. Escort them to the sleep lab, provide a tour of the facility, and address any questions. Confirm compliance with pre-procedure instructions and assist with changing into sleepwear.
2. Electrode and Sensor Placement
Proper electrode placement is crucial for accurate data collection. Nurses should follow standardized protocols for attaching EEG (electroencephalogram), EOG (electrooculogram), EMG (electromyogram), ECG (electrocardiogram), respiratory effort belts, nasal cannula or thermistor, pulse oximeter, and leg movement sensors. Use hypoallergenic materials if necessary and ensure that all connections are secure but comfortable. Explain each step to the patient to reduce anxiety and promote cooperation.
3. Monitoring and Safety
During the sleep study, nurses must continuously monitor the patient for signs of distress, discomfort, or equipment malfunction. This includes:
- Video and Audio Surveillance: Observe the patient remotely using cameras and microphones to detect abnormal movements or respiratory events.
- Vital Signs Monitoring: Regularly check heart rate, oxygen saturation, and respiratory rate, especially for high-risk patients.
- Immediate Response: Be prepared to intervene in case of medical emergencies, such as arrhythmias, severe desaturation, or seizures. Emergency equipment and medications should be readily accessible.
- Comfort Measures: Adjust pillows, bedding, and room temperature as needed. Offer reassurance and address any sleep disruptions caused by anxiety or unfamiliar surroundings.
4. Documentation During the Study
Accurate documentation is essential for interpreting sleep study results. Nurses should record:
- Time of lights out and lights on
- Any interventions or disturbances during the night
- Patient complaints or requests
- Technical issues with equipment
- Medication administration, if applicable
Note any factors that could affect sleep quality, such as pain, noise, or anxiety, as these may need to be considered during data analysis.
Post-Procedure Nursing Care
1. Electrode Removal and Skin Care
After the study, gently remove all electrodes and sensors, taking care to avoid skin irritation or injury. Clean residual gel or adhesive from the skin using mild soap and water. Inspect for any redness, swelling, or allergic reactions, and provide appropriate care.
2. Patient Recovery and Discharge
Allow the patient time to fully awaken and orient themselves. Offer breakfast or light refreshments if appropriate. Review the post-study instructions, which may include resuming regular medications, follow-up appointments, and information about when results will be available.
3. Patient Education and Support
Provide verbal and written information about potential side effects, such as mild skin irritation or disrupted sleep, and advise the patient to report any concerning symptoms. Encourage questions and offer support regarding anxiety about test results or future treatment options.
4. Documentation and Communication
Document the completion of the study, any post-procedure complications, and patient responses. Communicate significant findings or concerns to the sleep specialist or referring physician promptly.
Special Considerations in Nursing Care
1. Pediatric and Geriatric Patients
Children and older adults may require additional support and reassurance. For pediatric patients, allow a parent or caregiver to remain present if possible, and use age-appropriate explanations. For elderly patients, be mindful of mobility issues, sensory deficits, and comorbidities that may affect tolerance of the procedure.
2. Patients with Disabilities or Chronic Illness
Adapt care for patients with physical, cognitive, or sensory impairments. Use communication aids, ensure accessibility, and modify equipment placement as needed. Consult with multidisciplinary teams for complex cases.
3. Cultural Sensitivity
Respect patients’ cultural beliefs and preferences regarding sleep, privacy, and physical contact. Provide interpreters or culturally appropriate educational materials if necessary.
4. Quality Assurance and Professional Development
Nurses involved in sleep studies should participate in ongoing education and training to stay current with advances in polysomnography technology, sleep medicine, and patient safety practices. Regular audits of procedures and outcomes help maintain high standards of care.
REFERENCES
- American Academy of Sleep Medicine. In-Lab Sleep Study. http://sleepeducation.org/essentials-in-sleep/in-lab-sleep-study
- National Sleep Foundation. Sleep Assessment & Evaluation: Sleep Center/Lab Tools. http://sleepdisorders.sleepfoundation.org/chapter-1-normal-sleep/sleep-assessment-evaluation-sleep-center-lab-tools/
- National Sleep Foundation. Sleep Studies http://sleepfoundation.org/sleep-topics/sleep-studies).
- National Heart, Lung, and Blood Institute. Sleep Studies (http://www.nhlbi.nih.gov/health/health-topics/topics/slpst).
- American Thoracic Society. Patient Education/Information Series. Sleep Studies: In the Sleep Laboratory and in the Home. https://www.thoracic.org/patients/patient-resources/resources/sleep-studies.pdf
- Welch KC, Goldberg AN. Chapter 41. Sleep Disorders. In: Lalwani AK, eds. CURRENT Diagnosis & Treatment in Otolaryngology—Head & Neck Surgery, 3e. New York, NY: McGraw-Hill; 2012.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





