Altered mental status (AMS) is a broad term used to represent a variety of diseases affecting mental functioning ranging from mild disorientation to coma. Fundamentally, a patient’s level of consciousness and cognition are combined to form their mental status. Patients may have abnormalities of either one or both of these components.
The range of differential diagnoses is extensive, however, they can often be classified in the following categories:
- Primary intracranial disease
- Systemic illness that affects the central nervous system (infection)
- Exogenous toxins
- Drug withdrawal
Trauma, metabolic abnormalities, and toxic ingestion are the most frequent causes of altered mental status in newborns and young children. Young adults most frequently exhibit altered mental status as a result of exposure to toxic substances or trauma. The most frequent causes of altered mental status in the elderly include stroke, illness, drug-drug interactions, or modifications to the living environment.
Nursing Process
To lower patient morbidity and mortality, it is necessary to identify the early indicators of altered mental status, determine the underlying cause, and administer the proper care. The nurse can assist in symptomatic management techniques including volume resuscitation for shock, antibiotics for sepsis, glucose for hypoglycemia, or the prevention of deterioration by intubating.
A thorough physical examination and history taking are necessary to manage and evaluate changes in mental status. Mental status changes can appear suddenly and are a symptom of an underlying cause. Safety is also a priority as AMS can lead to falls and injury.
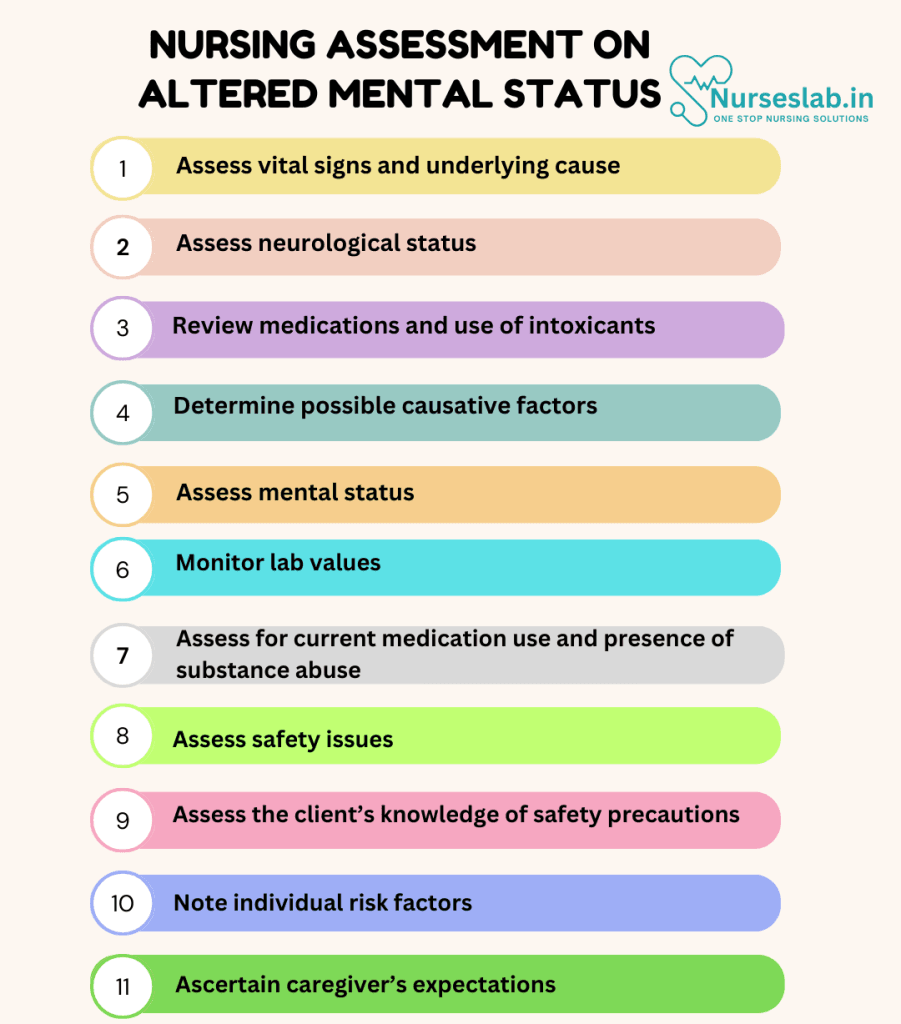
Nursing Assessment
Effective nursing assessment and intervention are crucial in managing AMS to promote patient safety, well-being, and optimal outcomes.
Initial Evaluation
The initial evaluation of a patient with AMS involves a thorough medical history, physical examination, and diagnostic tests. Key aspects to assess include:
Medical History
- Review the patient’s medical history for potential causes of AMS, such as infections, metabolic disturbances, neurological conditions, psychiatric disorders, and substance use.
- Inquire about the onset, duration, and progression of symptoms, as well as any associated factors such as recent illnesses, medication changes, or traumatic events.
- Assess for any history of previous episodes of AMS or underlying chronic conditions that may contribute to the current presentation.
Physical Examination
- Conduct a comprehensive physical examination, focusing on vital signs, neurological status, and any signs of trauma or infection.
- Evaluate the patient’s level of consciousness, orientation, memory, attention, and cognitive function using standardized assessment tools such as the Glasgow Coma Scale (GCS) or Mini-Mental State Examination (MMSE).
- Assess for potential indicators of underlying medical conditions, such as fever, dehydration, hypoxia, or signs of substance intoxication or withdrawal.
Diagnostic Tests
- Obtain laboratory tests to evaluate potential metabolic, infectious, or toxic causes of AMS, including complete blood count (CBC), electrolytes, glucose, liver and renal function tests, and toxicology screens.
- Perform imaging studies, such as computed tomography (CT) scan or magnetic resonance imaging (MRI) of the brain, to identify any structural abnormalities, such as stroke, hemorrhage, or tumors.
- Consider additional tests, such as lumbar puncture, electroencephalography (EEG), or urine analysis, based on clinical suspicion of specific conditions, such as meningitis, seizure disorder, or urinary tract infection.
Nursing Intervention
Nursing interventions for altered mental status focus on assessing the underlying cause, ensuring patient safety, and promoting cognitive function. Here are some key interventions:

Immediate Care
- Ensure patient safety by implementing fall precautions, monitoring vital signs, and providing a calm and structured environment.
- Address any immediate medical needs, such as administering intravenous fluids for dehydration, oxygen therapy for hypoxia, or antipyretics for fever.
- Collaborate with the healthcare team to initiate appropriate medical treatments based on the identified underlying cause of AMS.
Ongoing Monitoring
- Closely monitor the patient’s mental status, vital signs, and response to interventions, documenting any changes or trends in symptoms.
- Assess for potential complications, such as aspiration, pressure ulcers, or infections, and implement preventive measures as needed.
- Provide supportive care, including assistance with activities of daily living (ADLs), nutrition, and hydration, to promote patient comfort and well-being.
Patient and Family Education
- Educate the patient and their family about the potential causes and treatment options for AMS, emphasizing the importance of adherence to prescribed medications and follow-up care.
- Discuss strategies to manage stress and prevent future episodes, such as maintaining a healthy lifestyle, recognizing early warning signs, and seeking prompt medical attention for any concerning symptoms.
- Provide resources and support for coping with the emotional and psychological impact of AMS, including referral to counseling or support groups as needed.
Discharge Planning
- Develop a comprehensive discharge plan that includes clear instructions for medication management, follow-up appointments, and any necessary home care or support services.
- Ensure that the patient and their family understand the discharge plan and have access to emergency contact information and crisis intervention resources.
- Coordinate with community resources and healthcare providers to facilitate a smooth transition from hospital to home and support ongoing recovery and management of AMS.
Nursing Care Plans
Once the nurse identifies nursing diagnoses for an altered mental status, nursing care plans help prioritize assessments and interventions for both short and long-term goals of care. In the following section, you will find nursing care plan examples for altered an mental status.
Ineffective Cerebral Tissue Perfusion
Ineffective cerebral tissue perfusion associated with altered mental status can be caused by decreased cerebral blood flow due to underlying conditions such as metabolic conditions (e.g. hypoglycemia or hypoxia), low levels of acetylcholine synthesis, and substrate deficiency for neural function.
Nursing Diagnosis: Ineffective Tissue Perfusion
Related to:
- Decrease cerebral blood flow
- Metabolic conditions
- Primary intracranial disease
- A systemic disease affecting the central nervous system (CNS)
- Exogenous toxins
- Drug withdrawal
As evidenced by:
- Decreased Glasgow coma scale (GCS)
- Decreased level of consciousness (LOC)
- Diminished reflexes
- Alterations in pulse rate
- Alterations in blood pressure
- Increased intracranial pressure
- Decrease cerebral perfusion pressure
- Behavioral changes
Expected outcomes:
- Patient will be able to demonstrate effective tissue perfusion as evidenced by the GCS and LOC within normal limits
- Patient will not experience worsening in AMS such as coma or require intubation
Assessment:
1. Assess vital signs and underlying cause.
Persistent fluctuations in vital signs may trigger cerebral hypoperfusion and inadequate blood supply in the brain. The nurse can monitor the vital signs and assess for an underlying cause through a thorough physical examination and history assessment.
2. Assess neurological status.
A detailed neurological and cognitive assessment including the Glasgow coma scale (GCS) and level of consciousness (LOC) is done to determine whether there is a nervous system problem. Neurological checks should be performed frequently and routinely to quickly recognize changes.
3. Review medications and use of intoxicants.
Assess the client’s medication regimen for overdoses of narcotics or improper use of antihypertensives. Assess for alcohol or illegal substance use affecting AMS.
Interventions:
1. Determine the appropriate level of care.
Collaborate with the interdisciplinary team to determine the appropriate level of care. Patients with AMS related to cerebral perfusion likely require monitoring in the neuro-ICU by specially trained nurses.
2. Administer fluids and electrolytes as prescribed.
Fluid resuscitation aims to improve cerebral tissue perfusion and hemodynamics. To compensate for losses and keep circulation and cellular function intact, provide fluids and electrolytes as needed.
3. Prepare the client for surgical procedure as indicated.
The client may be a candidate for a surgical procedure such as carotid endarterectomy or evacuation of cerebral hematoma or lesion. The nurse must prepare for a possible surgical procedure to improve tissue perfusion in the brain.
Acute Confusion
Acute confusion associated with altered mental status can be caused by a disruption to consciousness, attention, cognition, and perception that occurs suddenly and is reversible.
Nursing Diagnosis: Acute Confusion
Related to:
- Alteration in brain function
- Alteration in sleep
- Alcohol or drug abuse
- Hypoxia
- Metabolic imbalances
- Delirium
- Disrupted perception
Evidenced by:
- Hallucinations
- Restlessness
- Decreased level of consciousness
- Impaired cognition
- Disrupted psychomotor functioning
- Inability to perform purposeful behavior
- Inappropriate verbal responses
Expected outcomes:
- Patient will be able to regain orientation to person, place, and time
- Patient will identify lifestyle changes to prevent acute confusion reoccurrence
Assessment:
1. Determine possible causative factors.
Acute confusion is a symptom that can be brought on by a variety of causes, including hypoxia, metabolic, endocrine, and neurological problems, toxins, electrolyte imbalances, infections of the CNS, nutritional deficiencies, and acute psychiatric illnesses.
2. Assess mental status.
The nurse can perform a thorough mental status assessment that can assist in differentiating between mental illness, cognitive disability, and mood disorders.
3. Monitor lab values.
If mental or psychosocial issues are ruled out, obtain a CBC panel, ABGs, liver function levels, urinalysis, and more to decipher internal causes of AMS.
4. Assess for current medication use and presence of substance abuse.
Certain medications such as barbiturates, amphetamines, and opiates as well as substances like alcohol or illegal drugs are associated with a high risk of adverse reactions, delirium, and confusion, especially during the withdrawal stage.
Interventions:
1. Provide constant orientation to person, place, and time as needed.
Reorient as needed to person, place, time, and situation. Challenging illogical thinking may cause defensive reactions. Hence, presenting reality will help the client by eliminating confusion.
2. Prevent sundowning.
The nurse can encourage the client to get plenty of exposure to light, maintain a routine of activities, limit napping during the daytime, and provide familiar objects.
3. Educate caregivers to monitor the client at home.
Caregivers must know when to contact the healthcare provider for a sudden change or worsening in cognition and behavior.
4. Provide a stable and calm environment.
Prevent worsening confusion and potential agitation by providing an environment that is quiet without overstimulation that allows for rest.
Risk for Injury
Risk for Injury associated with altered mental status can result in physical harm due to a disruption of consciousness, attention, and cognition as well as impaired perception. This increases the risk of an unsafe environment and the risk of injury.
Nursing Diagnosis: Risk for Injury
Related to:
- Alteration in brain function
- Impaired sleep cycle
- Hypoxia
- Intoxication
Note: A risk diagnosis is not evidenced by signs and symptoms as the problem has not yet occurred. Interventions are aimed at prevention.
Expected outcomes:
- Patient will be able to verbalize an understanding of risk factors that may cause injury
- Patient will identify behaviors and measures to reduce risk factors and protect themselves from injury
- Patient will remain free from injury
Assessment:
1. Assess safety issues.
The nurse can make detailed evaluations of potential safety issues related to AMS. Inaccurate assessment, intervention, or referral may increase the risk of harm.
2. Assess the client’s knowledge of safety precautions.
Assess for awareness of the needs for safety, injury prevention, and motivation to do so in settings such as the home, community, and workplace. This may help the nurse identify areas of inaccuracy, knowledge deficits, and the need for education, especially for clients with AMS.
3. Note individual risk factors.
The client’s age, gender, developmental stage, capacity for making decisions, and degree of cognitive limit and competence should all be noted. These have an impact on the client’s capacity to protect oneself and/or others.
4. Ascertain caregiver’s expectations.
Clients who have AMS typically have caregivers. Review the expectations of caregivers who care for those who are elderly, mentally disabled, or emotionally fragile.
Interventions:
1. Provide safe nursing care.
The nurse must consider a culture of safety when implementing nursing care to promote client safety and serve as an example of safe conduct.
2. Inform the client about all treatments and medications.
Communication with the client is essential because it builds and preserves trust. Clear communication can help the client feel less angry, worried, and depressed as well as increase cooperation with the implementation of care and improve the safety of the client.
3. Reduce the risk of injury.
The nurse can identify safety measures and interventions that promote both individual and environmental safety. Examples include keeping the bed alarm on, keeping the call bell within reach, using assistive devices, and more.
4. Prepare the client for a safe home environment.
Discuss safety measures to improve the home environment such as equipment needs, fall prevention, how to call for help, medication safety, and more.
Nursing Diagnoses and Rationales for Altered Mental Status
1. Risk for Anxiety
Rationale: The unpredictable nature of bipolar disorder and its potential complications can cause significant anxiety for patients and their families. Monitoring for signs of anxiety, providing reassurance, and offering psychological support can help manage anxiety. Involving mental health professionals and encouraging relaxation techniques, such as deep breathing exercises and mindfulness, can also be beneficial.
2. Risk for Noncompliance
Rationale: Patients with bipolar disorder may struggle with adherence to treatment regimens due to side effects, denial of illness, or cognitive impairments during mood episodes. Educating patients about the importance of medication adherence, simplifying medication schedules, and involving them in decision-making can improve compliance. Regular follow-ups and the use of reminder tools can also support adherence.
3. Chronic Low Self-Esteem
Rationale: Bipolar disorder can lead to feelings of worthlessness and low self-esteem, especially during depressive episodes. Providing positive reinforcement, setting achievable goals, and encouraging participation in therapeutic activities can help boost self-esteem. Offering individual and group therapy sessions can also support the patient’s self-worth and personal growth.
4. Sleep Pattern Disturbance
Rationale: Bipolar disorder often disrupts normal sleep patterns, with insomnia during manic episodes and hypersomnia during depressive episodes. Monitoring sleep patterns, creating a restful environment, and establishing a regular sleep routine can help manage sleep disturbances. Administering sleep aids or mood stabilizers as prescribed and encouraging relaxation techniques before bedtime can also be effective.
5. Ineffective Role Performance
Rationale: The symptoms of bipolar disorder can impair the patient’s ability to fulfill their roles in family, work, or social settings. Assessing the impact of the disorder on role performance, providing role-specific support, and involving occupational therapy can help patients regain functionality. Encouraging gradual reintegration into daily roles and responsibilities can promote a sense of normalcy and purpose.
6. Disturbed Thought Processes
Rationale: Altered mental status can lead to disorganized thinking, impaired judgment, and difficulty concentrating. Monitoring cognitive changes, providing a structured environment, and using clear and simple communication can help manage disturbed thought processes. Cognitive-behavioral therapy and medication adjustments may also be necessary.
7. Impaired Social Interaction
Rationale: Altered mental status can affect a patient’s ability to engage in appropriate social interactions and maintain relationships. Encouraging participation in social activities, providing social skills training, and facilitating support groups can enhance social functioning. Family education and involvement are also crucial in supporting the patient’s social interactions.
8. Risk for Injury
Rationale: Patients with altered mental status may be at increased risk for injury due to impaired judgment, agitation, or psychomotor disturbances. Implementing safety measures, closely monitoring the patient, and providing a secure environment can help prevent injuries. Educating caregivers about potential risks and safety strategies is also important.
9. Self-Care Deficit
Rationale: Altered mental status can impair a patient’s ability to perform activities of daily living (ADLs). Assessing the patient’s self-care abilities, providing assistance with ADLs, and encouraging participation in self-care activities can promote independence. Occupational therapy and adaptive equipment may also be beneficial.
10. Risk for Violence
Rationale: Patients with altered mental status may exhibit aggressive or violent behaviors due to confusion, paranoia, or frustration. Monitoring for signs of agitation, using de-escalation techniques, and providing a calm and safe environment can help manage violent behaviors. Involving mental health professionals and considering medication adjustments may also be necessary.
REFERENCES
- Blanchard, G. (2022, May 13). Evaluation of altered mental status. Clinical decision support for health professionals. https://bestpractice.bmj.com/topics/en-us/843
- Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2019). Nurse’s pocket guide: Diagnoses, interventions, and rationales (15th ed.). F A Davis Company.
- Hinkle, J. L., & Cheever, K. H. (2018). Management of Patients With Neurologic Dysfunction. In Brunner and Suddarth’s textbook of medical-surgical nursing (11th ed., pp. 5169-5213). Wolters Kluwer India Pvt.
- Patti, L., & Gupta, M. (2022, May 1). Change in mental status – StatPearls – NCBI bookshelf. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK441973/
- American Psychiatric Association. (2023). Diagnostic and Statistical Manual of Mental Disorders (5th ed., Text Revision). American Psychiatric Publishing.
- Barr, J., et al. (2023). Clinical Practice Guidelines for the Management of Pain, Agitation, and Delirium in Adult Patients in the Intensive Care Unit. Critical Care Medicine, 51(4), e58-e110.
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2024). NANDA International Nursing Diagnoses: Definitions & Classification 2024-2026. Thieme.
- Inouye, S. K., et al. (2023). Delirium in elderly people. The Lancet, 401(10395), 1615-1628.
- Swartz, M. H. (2022). Textbook of Physical Diagnosis: History and Examination (8th ed.). Elsevier.
- Toney-Butler, T. J., & Thayer, J. M. (2023). Nursing Process. In StatPearls. StatPearls Publishing.
- Wilson, J. E., et al. (2024). Delirium. Nature Reviews Disease Primers, 10(1), 1-34.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.







