Community Health: Overall health and well-being are greatly impacted by the communities in which patients live and work. Access to care is influenced by economic, social, and political issues. Depending on the needs of the individual and the population, it may be a major factor in determining physical, emotional, and mental health as well as morbidity and mortality.
Race and ethnicity, educational attainment, gender, and income are examples of structural characteristics that may be significantly predictive of overall health. These kinds of variables reveal risk factors for chronic health conditions and present opportunities for community-based treatments.
Nursing Process
Acute and chronic care are prioritized in community-based nursing, which encompasses practice settings such as:
- Home health
- School nursing
- Case management
- Outpatient clinics and health departments
The focus of nursing practice includes wellness promotion, prevention, maintenance, and disease control. At the disease end of the continuum, acute and chronic disorders have traditionally received the majority of attention in healthcare. Nursing care aimed at prevention and education can improve health outcomes and reduce healthcare burden, resources, and costs.
Nursing Assessment
A comprehensive nursing assessment in community health involves several critical components:

- Demographic Analysis: Understanding the population’s characteristics, including age, gender, ethnicity, and socioeconomic status.
- Health Status: Assessing the community’s overall health, including common illnesses, chronic conditions, and mortality rates.
- Environmental Factors: Evaluating the physical, social, and economic environments that influence health outcomes.
- Health Behaviors: Identifying prevalent health behaviors such as smoking, physical activity, and nutrition.
- Healthcare Access and Utilization: Analyzing the availability, accessibility, and utilization of healthcare services within the community.
Nursing Interventions
Nursing interventions aim to reduce the incidence of diseases and promote healthy behaviors. These include:
- Immunization programs to prevent infectious diseases
- Health education campaigns to raise awareness about healthy lifestyles and disease prevention
- Screening and early detection programs for conditions such as cancer, diabetes, and hypertension
- Nutrition and physical activity initiatives to combat obesity and related health issues
Nursing Care Plans
Once the nurse identifies nursing diagnoses related to community health, nursing care plans help prioritize assessments and interventions for both short and long-term goals of care. In the following section, you will find nursing care plan examples for community health.
Deficient Knowledge
Deficient Knowledge associated with community health can be caused by inadequate knowledge of resources, access to the healthcare system and programs, and an understanding of individual and community health risks.
Nursing Diagnosis: Deficient Knowledge
Related to:
- Inadequate knowledge of community support and resources
- Inadequate access to healthcare professionals
- Lack of financial and social resources
- Program budget, outcome information, or evaluation plan deficiencies
- Inability of existing programs to address health concerns
As evidenced by:
- Community members’ verbalization of confusion/concern
- Community members’ noncompliance with the health program
- Community members’ inquiries about a certain topic
- Community members’ misconceptions
- Community members’ exacerbation of health symptoms
- Health program’s inability to address the health concern
- Preventable hospital readmissions
- Increased incidence of physiological or psychological conditions
Expected outcomes:
- Community will be able to identify the programs’ advantages and disadvantages in achieving health-related objectives.
- Community will be able to create a plan to meet the community’s recognized health needs.
- Community will be able to demonstrate behavior and lifestyle modifications towards the improvement of community health.
Assessment:
1. Assess healthcare providers’ knowledge and practices related to the community’s health.
Having the same knowledge and using the same verbiage makes it easier for those working in the community to recognize one another and communicate ideas more effectively.
2. Assess the community’s existing and potential health problems.
By identifying particular issues, population-based treatments can focus on the existing problem that may be solved by primary prevention and proactive intervention.
3. Assess the community’s resources.
Knowing what resources are currently accessible and how the community accesses them helps to identify potential gaps. Resources may not be meeting the needs of the community or the community may not be aware they exist.
4. Note the community members’ complaints/ concerns.
Taking note of the members’ concerns presents a realistic image of issue areas through feedback from those who are affected most.
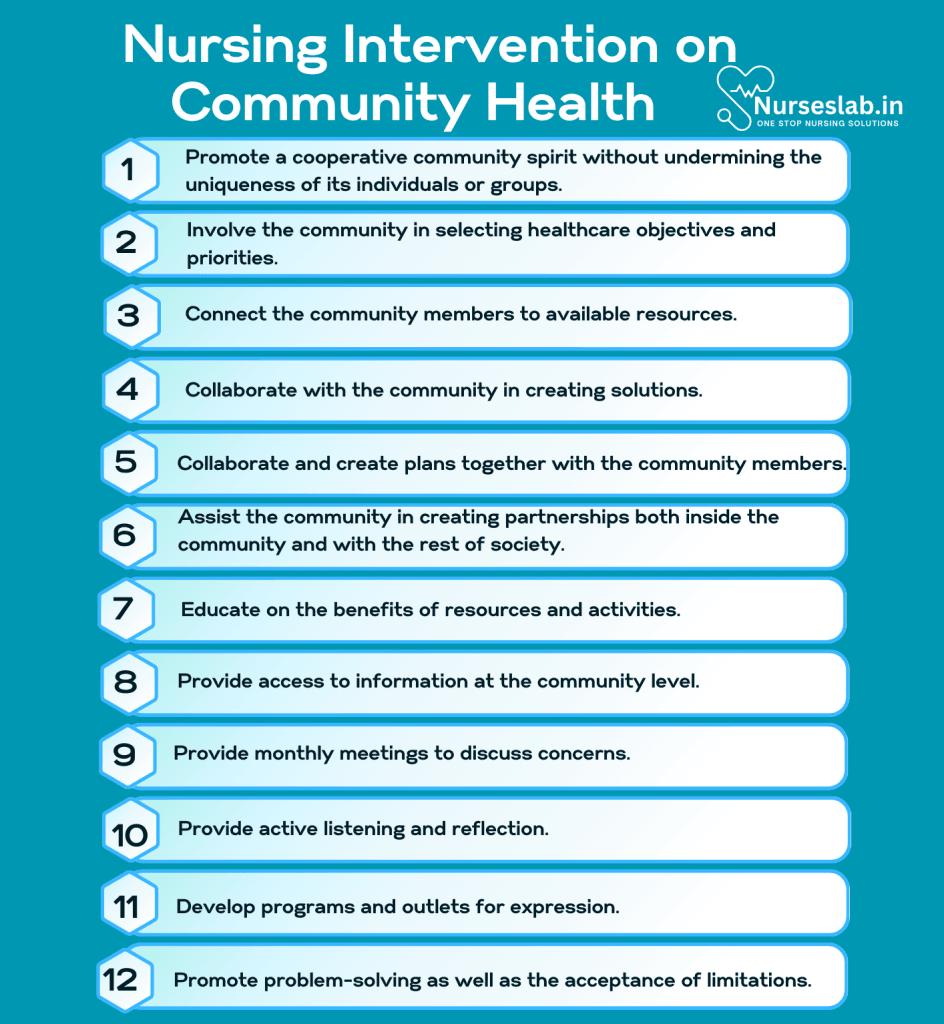
Interventions:
1. Promote a cooperative community spirit without undermining the uniqueness of its individuals or groups.
People are more likely to cooperate to create plans for identifying and improving healthcare for the community when they feel respected and valued.
2. Involve the community in selecting healthcare objectives and priorities.
Involving the community members in assessing the problem and creating goals and priorities that are important to them will increase collaboration and adherence.
3. Connect the community members to available resources.
Assure the best possible delivery of healthcare and connect people to the services they need through transportation support, 2-1-1 programs, and free clinics.
4. Collaborate with the community in creating solutions.
Collaboration encourages a sense of control and involvement, which aids in more efficient problem-solving.
Ineffective Community Coping
Ineffective community coping can be caused by unsatisfactory community efforts to adapt and solve problems in a way that satisfies community desires or needs.
Nursing Diagnosis: Ineffective Community Coping
Related to:
- Insufficient resources for problem-solving
- Inadequate community resources (emergency services, transportation)
- Lack of social support services
As evidenced by:
- Community members’ expression of lack of support or excessive stress
- Higher rates of illness
- High rates of crime, abuse, unemployment, and poverty
- Community members’ expression of powerlessness or hopelessness
Expected outcomes:
- Community will report an identifiable improvement in coping such as decreased crime rates or increased employment
- Community will be able to choose appropriate alternatives to undesirable activities for problem-solving and adaptability
Assessment:
1. Assess the community’s needs.
A needs assessment is essential to identify the gaps preventing it from achieving its targeted objectives.
2. Assess disaster plans and response to emergencies.
Evaluate the policies of local and regional efforts in the face of epidemics, threats, terrorist attacks, and natural catastrophes to assess preparedness.
3. Identify the availability, accessibility, and usage of community resources.
Even when resources are accessible, they are not always utilized properly or to their full potential. Evaluate programs and resources available, referral processes, and follow-up measures.
4. Identify unmet community expectations.
Establishing shortcomings is the first step in overcoming gaps. Communication is crucial to understanding the perspective of the community.
Interventions:
1. Collaborate and create plans together with the community members.
Organize interactions inside the community to manage interactions and meet needs. This encourages long-term participation and adherence.
2. Assist the community in creating partnerships both inside the community and with the rest of society.
Creating partnerships between the community and society encourages the community’s long-term development and constant improvement to address both present and upcoming issues.
3. Educate on the benefits of resources and activities.
Help the community recognize the benefits of improvement efforts and how their safety, health, and happiness depend on a cohesive community working together.
4. Provide access to information at the community level.
Meet them where they are. Use TV, flyers, radio, social media, and more to disseminate resource information. Information needs to be geared toward all educational and cultural levels.
Readiness for Enhanced Community Coping
Readiness to meet improved community adaptation and problem-solving through activities, management, and communication.
Nursing Diagnosis: Readiness for Enhanced Community Coping
Related to:
- Motivation to improve health and stress management
- Desire to increase social change
- Responsiveness of possible community transformation
As evidenced by:
- Positive communication among groups
- Addition of health programs (nutrition, exercise, immunizations)
- Community planning events
Expected outcomes:
- Community will be able to effectively manage stressors through community resources
- Community will be able to verbalize appropriate coping techniques
Assessment:
1. Review the community’s plan for coping with problems.
Reviewing the community’s plan for coping with problems will help in the improvement of the plan according to the current needs of the community.
2. Assess the stressors of the community.
When preparing interventions to improve coping skills, it is important to accurately identify unique community stressors to know which interventions are relevant.
3. Assess the community members’ social support.
Community leaders can assist in supporting healthy coping to enable the community to move forward and improve current situations.
4. Assess the community’s current coping strategies.
Determining the current community coping strategies will assist in recognizing negative coping mechanisms and which techniques are needed.
Interventions:
1. Provide monthly meetings to discuss concerns.
Discuss existing stressors and upcoming or future concerns for effective intervention and planning.
2. Provide active listening and reflection.
Actively listening to the community members and reflecting on how they perceive their current situation can offer insight. The nurse will also gain more data to establish an accurate plan.
3. Develop programs and outlets for expression.
Coping can be enhanced through art, music, exercise, meditation, and more. Provide classes and stress-management programs to educate on proper coping.
4. Promote problem-solving as well as the acceptance of limitations.
Problem-solving skills can be taught but successful coping also involves recognizing and accepting when situations cannot be changed.
Nursing Diagnoses and Rationale for Community Health
1. Risk for Infection
Rationale: Community health settings often involve diverse populations, including individuals with chronic illnesses, elderly patients, and those with compromised immune systems. The close quarters and frequent interactions can facilitate the spread of infectious diseases. Nurses should promote hand hygiene, administer vaccinations, and educate patients about infection prevention measures to reduce the risk of infection. Regular screenings and timely treatment are crucial for managing potential outbreaks.
2. Ineffective Health Maintenance
Rationale: Patients may lack the knowledge, resources, or motivation to effectively manage their health, particularly those with chronic conditions or socioeconomic challenges. Nurses should conduct thorough assessments to identify barriers to health maintenance and collaborate with patients to develop personalized care plans. Providing education on disease management, medication adherence, and lifestyle modifications can empower patients to take control of their health.
3. Noncompliance
Rationale: Noncompliance with medical recommendations and treatment plans can result from various factors, including financial constraints, cultural beliefs, and lack of understanding. Nurses should use a patient-centered approach to address these issues, building trust and rapport with patients. Simplifying treatment regimens, involving family members in care, and utilizing community resources can enhance compliance and improve health outcomes.
4. Impaired Social Interaction
Rationale: Social isolation and impaired social interaction can have significant impacts on mental and physical health, particularly among elderly and disabled patients. Nurses should assess patients’ social support networks and encourage participation in community activities and support groups. Facilitating access to transportation and social services can help patients maintain meaningful connections and reduce feelings of loneliness.
5. Knowledge Deficit
Rationale: A lack of knowledge about health conditions, treatments, and preventive measures can hinder patients’ ability to make informed decisions and effectively manage their health. Nurses should provide clear, evidence-based education tailored to the patient’s needs and level of understanding. Using visual aids, demonstrations, and teach-back methods can enhance comprehension and retention of information.
6. Imbalanced Nutrition: Less than Body Requirements
Rationale: Chronic respiratory distress and increased caloric expenditure from labored breathing can lead to weight loss and malnutrition in patients with emphysema. Appetite may also be reduced due to fatigue and depression. Nurses should assess nutritional status and collaborate with dietitians to develop a high-calorie, high-protein diet plan. Small, frequent meals and nutritional supplements can help meet the patient’s caloric needs. Encouraging adequate hydration is also important for mucus clearance.
7. Disturbed Sleep Pattern
Rationale: Dyspnea and coughing can interfere with the patient’s ability to achieve restful sleep, leading to fatigue and decreased overall well-being. Nurses should assess the patient’s sleep patterns and recommend strategies to improve sleep quality, such as elevating the head of the bed, using a humidifier, and practicing good sleep hygiene. Medications to manage symptoms and promote relaxation may also be beneficial.
8. Chronic Sorrow
Rationale: The progressive and irreversible nature of emphysema can lead to feelings of loss and chronic sorrow as patients cope with declining health and changes in lifestyle. Nurses should provide empathetic support and facilitate open discussions about the patient’s feelings and concerns. Referrals to counseling services or mental health professionals can help patients navigate their emotional responses and develop effective coping strategies.
9. Ineffective Coping
Rationale: The daily challenges of living with emphysema can overwhelm patients and their families, leading to ineffective coping mechanisms. Providing education about the disease, involving patients in their care plans, and encouraging the use of adaptive coping strategies can enhance their ability to manage the condition. Nurses should also assess for signs of depression or other mental health issues and provide appropriate referrals.
10. Social Isolation
Rationale: Limitations in physical activity and dependence on supplemental oxygen can restrict patients’ social interactions, leading to feelings of isolation and loneliness. Nurses should encourage patients to maintain social connections through phone calls, video chats, and participation in online support groups. Facilitating access to community resources and activities that accommodate the patient’s limitations can help reduce social isolation and improve quality of life.
11. Risk for Falls
Rationale: Elderly patients and those with mobility impairments are at an increased risk of falls, which can lead to serious injuries and complications. Nurses should conduct fall risk assessments and implement fall prevention strategies, such as providing assistive devices, removing environmental hazards, and educating patients and caregivers about safety measures. Regular exercise programs to improve strength and balance can also help reduce the risk of falls.
12. Altered Family Processes
Rationale: Chronic illnesses and health challenges can disrupt family dynamics and create stress within the household. Nurses should assess the impact of the patient’s condition on family members and provide support and resources to help families adapt. Encouraging open communication, providing education about the illness, and connecting families with support groups can promote healthy family processes and enhance coping.
13. Risk for Caregiver Role Strain
Rationale: The demands of caregiving can be physically and emotionally draining, leading to caregiver role strain. Nurses should assess caregivers for signs of stress and burnout and offer support and resources to alleviate the burden. Providing education about self-care, connecting caregivers with respite services, and facilitating access to counseling can help caregivers maintain their own health and well-being.
14. Dysfunctional Grieving
Rationale: Patients and their families may experience dysfunctional grieving in response to a serious diagnosis, loss of function, or death. Nurses should provide compassionate support and facilitate healthy grieving processes. Referrals to grief counselling and support groups can help individuals navigate their emotions and find constructive ways to cope with loss.
REFERENCES
- Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2019). Nurse’s pocket guide: Diagnoses, interventions, and rationales (15th ed.). F A Davis Company.
- Institute of Medicine (US) Committee. (1988). Public health as a problem-solving activity: Barriers to effective action – The future of public health – NCBI bookshelf. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK218227/
- Nies, M. A., & McEwen, M. (2019). Community/Public Health Nursing: Promoting the health of populations (7th ed.). Saunders.
- Rector, C. (2018). Community and Public Health Nursing : Promoting the Public’s Health (9th ed.). Wolters Kluwer Law & Business.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.







