Meningitis refers to the life-threatening inflammation of the meninges–the structures found at the vertebral canal and skull enclosing the brain and spinal cord. It is most commonly caused by infectious organisms such as bacteria and viruses and less frequently caused by fungi and parasites.
Risk factors for meningitis include extremes in age, those who live in community settings such as dormitories or military bases, immunosuppression, and not being vaccinated against meningitis.
Meningitis is acquired through two routes of transmission:
- Hematogenous seeding occurs when droplets of bacteria-contaminated respiratory secretions attach to the nasopharyngeal epithelial cells and subsequently enter the bloodstream.
- Direct contiguous spread happens when the pathologic agent infects the cerebrospinal fluid (CSF) through the ears or nose, foreign objects, or exposure during surgical procedures.
Fever, stiff neck, photophobia, headache, dizziness, nausea and vomiting, delirium, confusion, and irritability are some clinical manifestations in patients with meningitis. Young children or infants may present with a high fever, constant crying, inconsolability, drowsiness, and poor feeding.
To confirm meningitis, patients undergo a lumbar puncture to obtain CSF and analyze its white blood cell count, glucose and protein content, and presence of bacteria. A CT scan may also visualize swelling in the sinuses.
Nursing Process
Nurses should remain aware of symptoms and populations at risk for meningitis. Nursing interventions will include close monitoring for complications or deconditioning, preparing the patient for testing, and administering treatments. Nurses should advise patients who are candidates to receive the meningococcal vaccine.
Nursing Assessment
Prompt and effective nursing assessment and intervention are critical to managing meningitis, preventing complications, and promoting patient well-being
Initial Evaluation
The initial evaluation of a patient with suspected meningitis involves a thorough medical history and physical examination. Key aspects to assess include:
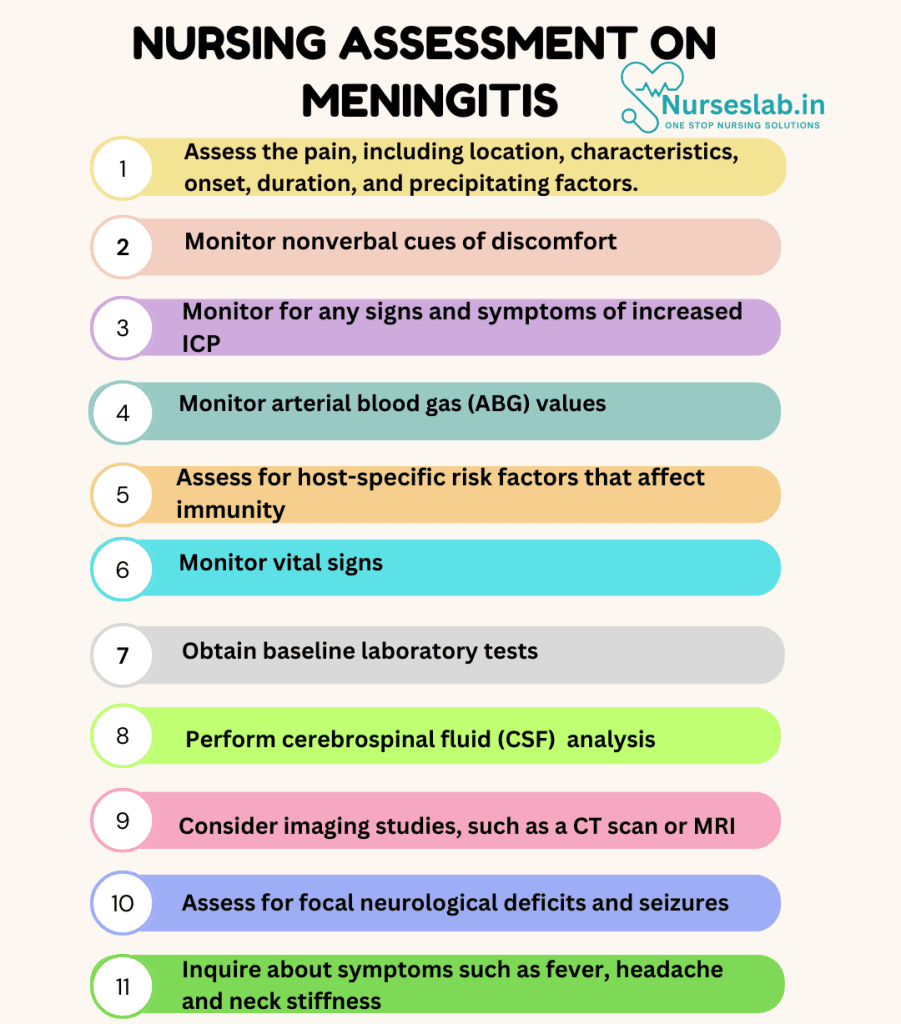
Medical History
- Review the patient’s history for risk factors such as recent infections, head trauma, or exposure to sick individuals.
- Inquire about symptoms such as fever, headache, neck stiffness, nausea, vomiting, photophobia, and altered mental status, which are common in meningitis.
Physical Examination
- Perform a comprehensive physical examination focusing on signs of meningeal irritation, such as neck stiffness (nuchal rigidity), Brudzinski’s sign, and Kernig’s sign.
- Assess for focal neurological deficits, seizures, and changes in consciousness or behavior.
- Monitor vital signs, including temperature, heart rate, respiratory rate, and blood pressure.
Laboratory Tests
- Obtain baseline laboratory tests, including complete blood count (CBC), blood cultures, and serum electrolytes.
- Perform a lumbar puncture to collect cerebrospinal fluid (CSF) for analysis, including cell count, glucose, protein levels, and culture to identify the causative organism.
- Consider imaging studies, such as a CT scan or MRI, to evaluate for complications like increased intracranial pressure or abscess formation.
Nursing Interventions
Nursing assessment and intervention are integral to the effective management of meningitis. By conducting thorough assessments, creating individualized care plans, and offering continuous support, nurses play a pivotal role in improving the health outcomes and quality of life for patients experiencing meningitis.
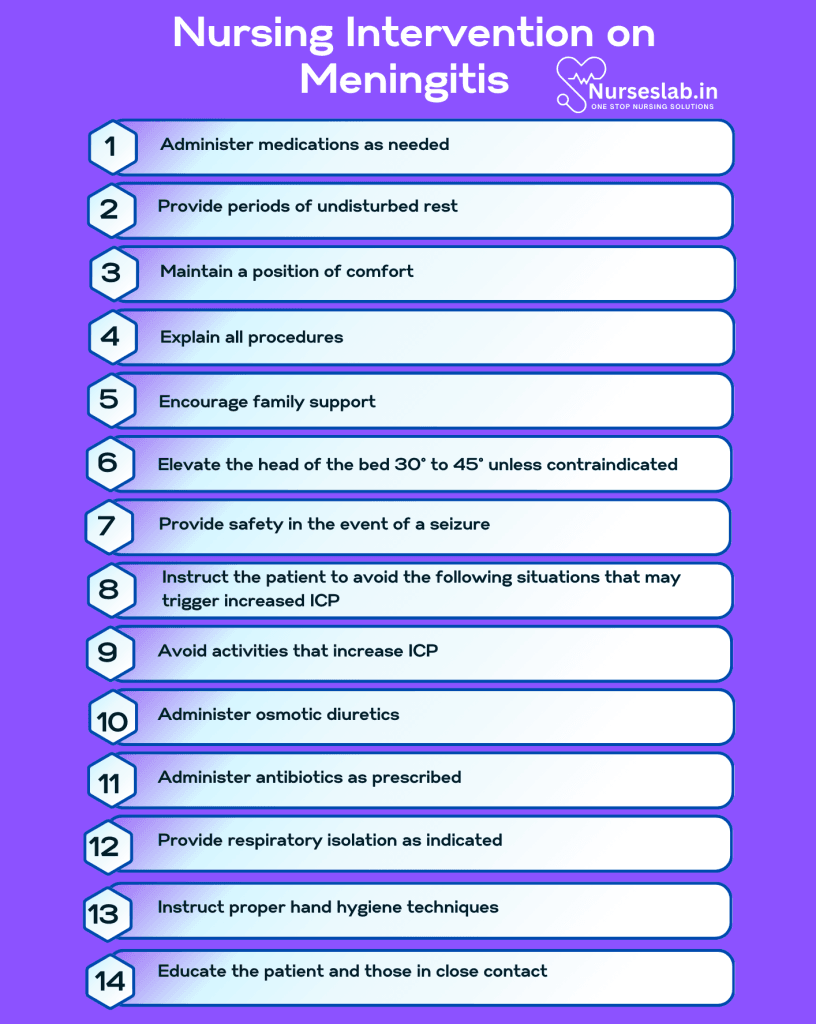
Immediate Care
- Initiate empiric antibiotic therapy as per the physician’s orders while awaiting culture results, particularly in suspected bacterial meningitis.
- Administer antipyretics to manage fever and analgesics for headache relief.
- Ensure the patient is in a safe environment, minimizing stimuli to reduce the risk of seizures and photophobia.
Monitoring and Support
- Continuously monitor vital signs, neurological status, and signs of increased intracranial pressure (e.g., changes in level of consciousness, pupillary changes, and Cushing’s triad).
- Maintain strict intake and output records to monitor fluid balance and prevent dehydration or fluid overload.
- Provide supportive care, including hydration, nutritional support, and respiratory assistance if needed.
Patient and Family Education
- Educate patients and their families about the nature of meningitis, its symptoms, and the importance of early intervention and ongoing management.
- Provide resources and information to help them make informed decisions about their care.
Nursing Care Plans
Once the nurse identifies nursing diagnoses for meningitis, nursing care plans help prioritize assessments and interventions for both short and long-term goals of care. In the following section, you will find nursing care plan examples for meningitis.
Impaired Comfort
Patients lack physical, psychosocial, cultural, and environmental ease due to the clinical manifestations caused by the disease.
Nursing Diagnosis: Impaired Comfort
Related to:
- Symptoms of disease
- Anxiety of situation
- Threat to health
- Stress
As evidenced by:
- Expression of anxiety, overwhelm
- Alterations in sleeping pattern
- Nausea and vomiting
- Fever
- Severe headache
- Light sensitivity
- Neck stiffness
- Feelings of irritability and restlessness
- Concern about procedures (spinal tap)
Expected outcomes:
- Patient will verbalize a sense of control over their situation.
- Patient will be able to rest/sleep quietly.
Assessment:
1. Assess the patient’s pain, including location, characteristics, onset, duration, and precipitating factors.
At the onset of meningitis, patients may feel severe headaches and neck pain and stiffness that may cause them to be unable to touch the chin to the chest or turn the head.
2. Monitor nonverbal cues of discomfort.
Expression of discomfort varies for each age group. Infants may be lethargic and refuse to eat or have shrill cries.
Interventions:
1. Administer medications as needed.
Analgesics, sedatives, antiemetics, and antipyretics manage the client’s pain, fever, nausea, and vomiting.
2. Provide periods of undisturbed rest.
Overstimulation due to unconsolidated activities may worsen the patient’s hyperirritable state. They are highly sensitive to touch, light, and loud sounds.
3. Maintain a position of comfort.
Nurses may elevate the head or turn patients to anticipate seizure or vomiting episodes. Patients with meningeal irritation and neck pain assume a position wherein the back is extended slightly and the body is curled.
4. Explain all procedures.
Before implementing tests such as a CT scan or spinal tap, educate the patient on what to expect to prevent anxiety and increased stress. If possible, remain with the patient to provide comfort.
5. Encourage family support.
When applicable, allow family visitation to provide emotional support to ease fear.
Risk for Increased Intracranial Pressure
Patients with meningitis may experience increased intracranial pressure (>15 mmHg) from the edema and contaminated CSF in the subarachnoid space.
Nursing Diagnosis: Risk for Increased Intracranial Pressure
Related to:
- Inflammation of the meninges
- Cerebral edema
As evidenced by:
A risk diagnosis is not evidenced by signs and symptoms as the problem has not yet occurred, and the goal of nursing interventions is aimed at prevention.
Expected outcomes:
- Patient will be alert, oriented, and calm without any alterations in the level of consciousness.
- Patient will not experience any seizure episodes.
- Patient will maintain stable vital signs:
- Pulse 60 to 100 beats per minute
- Respirations 16 to 20 breaths per minute
- BP >90/60, <140/90 mmHg
- Patient will not experience vomiting.
- Patient’s ICP monitoring will remain <15 mmHg.
Assessment:
1. Monitor for any signs and symptoms of increased ICP.
Headache, nausea and vomiting, altered mental status, and visual changes such as blurred/double vision may be suspicious for increased ICP. Cushing’s triad (hypertension, bradycardia, and irregular respirations) may signal brain herniation which is fatal. Prompt identification of these signs and symptoms prevents complications and death.
2. Monitor arterial blood gas (ABG) values.
ABG values reflect the gas exchange in the lungs, oxygen level, and arterial CO2. Maintaining arterial O2 (90 to 100 mmHg) and CO2 (25 to 30 mmHg) within normal limits prevents cerebral ischemia, congestion, and increased ICP.
Interventions:
1. Elevate the head of the bed 30° to 45° unless contraindicated.
Head elevation facilitates venous drainage to minimize cerebrovascular congestion. Thus, decreasing ICP.
2. Provide safety in the event of a seizure.
Seizure activity may occur as a result of meningitis or ICP. Prevent injuries by padding side rails, placing mats on the floor, and having emergency equipment at the bedside.
3. Instruct the patient to avoid the following situations that may trigger increased ICP:
- Carotid massage – causes bradycardia and decreased systemic circulation, followed by a sudden increase in circulation.
- Neck flexion restricts jugular venous drainage, thereby increasing cerebrovascular congestion and ICP.
- Rapid position changes – extreme flexion of hips and knees increases intrathoracic pressure and inhibits jugular venous drainage causing increased cerebrovascular congestion and ICP.
4. Avoid activities that increase ICP.
Coughing, suctioning, repositioning, and bathing may potentially increase ICP. Perform only as required.
5. Administer osmotic diuretics.
Mannitol can reduce cerebral edema and decrease ICP.
Risk for Infection
The patient is at risk for the hematogenous spread of the pathogenic agent, causing further complications.
Nursing Diagnosis: Risk for Infection
Related to:
- Stasis of body fluids
- Suppressed inflammatory response
- Lack of knowledge to avoid exposure to pathogens
As evidenced by:
A risk diagnosis is not evidenced by signs and symptoms as the problem has not yet occurred, and the goal of nursing interventions is aimed at prevention.
Expected outcomes:
- Patient will maintain vital signs within normal limits
- Patient will demonstrate normal CSF findings:
- Color: Clear
- Specific gravity/pH: 1.006–1.007/7.4
- Opening pressure: 50–200 mm H2O
- RBCs count: 0
- WBC count: 0–5, predominantly lymphocytes
- Proteins: 15–40 mg/dL
- Lactate: 1–3 mmol/ L
- Glucose: 50–80 mg/dL
- Microbial examination: No microorganism
- Patient will verbalize the understanding of risk factors for meningitis
Assessment:
1. Assess for host-specific risk factors that affect immunity.
Immunocompromised patients with HIV, diabetes, liver disease, or those who take steroids or undergo chemotherapy do not have the optimal immune response to combat opportunistic infections.
2. Monitor vital signs.
Hyperthermia, tachycardia, and tachypnea may indicate inflammatory or infectious processes. Noting the presence of a new onset of fever facilitates prompt identification and management.
Interventions:
1. Administer antibiotics as prescribed.
Bacterial meningitis is treated with broad-spectrum antibiotics such as ampicillin, ceftriaxone, and vancomycin. Antibiotics are selected based on the culture results, and they must pass the blood-brain barrier to penetrate the CSF adequately.
2. Provide respiratory isolation as indicated.
Meningitis is transmitted through droplets of contaminated respiratory secretions. Respiratory isolation measures such as wearing masks may be implemented and continued for 24 hours after the initiation of antimicrobials. Patients should be placed on droplet precautions in the hospital setting.
3. Instruct proper hand hygiene techniques.
Hand hygiene is the first line of defense against infection.
4. Educate the patient and those in close contact.
Education is important to prevent the spread. Prophylactic treatment may be required for some individuals in certain cases of meningitis. Vaccination can prevent meningitis and should be recommended for eligible patients.
Nursing Diagnoses and Rationales for Meningitis
1. Acute Pain
Rationale: Patients with meningitis often experience severe headache, neck stiffness, and other forms of pain due to inflammation of the meninges. Effective pain management can improve patient comfort and facilitate other aspects of care. Administering prescribed analgesics, monitoring pain levels, and employing non-pharmacological pain relief methods such as cold packs or relaxation techniques are essential.
2. Risk for Infection
Rationale: Meningitis, whether bacterial or viral, is an infectious disease that can spread to others or worsen in the patient. Implementing strict infection control measures, educating patients and families on hygiene practices, and monitoring for signs of secondary infections are vital to prevent the spread and complications of the disease.
3. Ineffective Cerebral Tissue Perfusion
Rationale: Inflammation and increased intracranial pressure associated with meningitis can compromise blood flow to the brain, leading to potential brain damage. Monitoring neurological status, maintaining head elevation, and ensuring adequate oxygenation can support cerebral perfusion and reduce the risk of complications.
4. Deficient Knowledge
Rationale: Patients and their families may lack understanding of meningitis, its causes, symptoms, treatment options, and preventive measures. Providing comprehensive education about the disease, medication adherence, and recognizing early signs of complications can empower patients and families to manage the condition effectively and reduce anxiety.
5. Hyperthermia
Rationale: Fever is a common symptom of meningitis and can exacerbate discomfort and dehydration. Regular monitoring of body temperature, administering antipyretics as prescribed, and employing cooling measures can help manage hyperthermia and improve patient comfort.
6. Disturbed Sensory Perception
Rationale: Meningitis can cause sensory disturbances such as photophobia, phonophobia, and altered auditory perception. Creating a calm and dimly lit environment, using earplugs or eye masks, and minimizing sensory stimuli can help reduce discomfort and agitation.
7. Risk for Seizures
Rationale: Inflammation and increased intracranial pressure may predispose patients with meningitis to seizures. Continuous monitoring for seizure activity, ensuring safety measures, and administering anticonvulsants as prescribed are critical to managing this risk.
8. Imbalanced Nutrition: Less Than Body Requirements
Rationale: Patients with meningitis may have decreased appetite, nausea, vomiting, and difficulty swallowing, leading to inadequate nutritional intake. Providing small, frequent meals, offering nutritional supplements, and involving a dietitian can ensure adequate nutrition and support recovery.
9. Risk for Fluid Volume Deficit
Rationale: Fever, vomiting, and decreased oral intake can lead to dehydration in patients with meningitis. Monitoring fluid balance, encouraging fluid intake, and administering intravenous fluids as necessary are essential to maintain hydration and prevent complications.
10. Impaired Physical Mobility
Rationale: Severe pain, stiffness, and neurological deficits can limit the mobility of patients with meningitis. Encouraging regular movement, providing assistive devices, and involving physical therapy can help maintain mobility and prevent complications such as muscle atrophy and pressure ulcers.
REFERENCES
- Carpenito, L.J. (2013). Nursing diagnosis: Application to clinical practice. (14th ed.). Lippincott Williams & Wilkins.
- Doenges, M. E., Moorhouse, M.F., & Murr, A.C. (2019). Nursing care plans: Guidelines for individualizing client care across the life span. (10th ed.). F.A. Davis.
- Hersi K, Gonzalez FJ, Kondamudi NP. Meningitis. [Updated 2022 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459360/
- Hrishi, A. P., & Sethuraman, M. (2019). Cerebrospinal Fluid (CSF) Analysis and Interpretation in Neurocritical Care for Acute Neurological Conditions. Indian journal of critical care medicine: peer-reviewed, official publication of Indian Society of Critical Care Medicine, 23(Suppl 2), S115–S119. https://doi.org/10.5005/jp-journals-10071-23187
- Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2023). Nursing diagnoses handbook: An evidence-based guide to planning care. St. Louis, MO: Elsevier.
- Archibald LK, Quisling RG. Central Nervous System Infections. Textbook of Neurointensive Care. 2013 May 7:427–517. doi: 10.1007/978-1-4471-5226-2_22. PMCID: PMC7122753.
- Ashwal, S. (1995). Neurologic Evaluation of the Patient With Acute Bacterial Meningitis. Neurologic Clinics, 13(3), 549-577. https://doi.org/10.1016/S0733-8619(18)30034-3
- Harding, M. M., Kwong, J., & Hagler, D. (2022). Lewis’s Medical-Surgical Nursing: Assessment and Management of Clinical Problems, Single Volume. Elsevier.
- Herdman, T. H., Kamitsuru, S., & Lopes, C. (2024). NANDA International Nursing Diagnoses – Definitions and Classification, 2024-2026.
- Hersi K, Gonzalez FJ, Kondamudi NP, et al. Meningitis (Nursing) [Updated 2023 Aug 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK568762/
- Ignatavicius, D. D., Rebar, C., & Heimgartner, N. M. (2023). Medical-Surgical Nursing: Concepts for Clinical Judgment and Collaborative Care. Elsevier.
- Silvestri, L. A. (2023). Saunders comprehensive review for the NCLEX-RN examination. St. Louis, MO: Elsevier.
- Jameson, L.J., et al. (2018). Harrison’s principles of internal medicine. (20th ed.). McGraw Hill.
- Jane LA, Wray AA. Lumbar Puncture. [Updated 2022 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557553/
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.







