Anorexia nervosa is a serious eating disorder that is potentially life-threatening if not recognized and treated appropriately. It is characterized by a very low body weight, an intense fear of gaining weight, and a distorted perception of weight. Persons that are anorexic will see themselves as fat even when they are not.
Not all patients with anorexia are thin. Some disguise their thinness and eating habits, making it difficult to recognize this condition. Unhealthy mental and behavioral components are a major aspect of the disease process.
Some signs of anorexia include:
- Intense fear of gaining weight
- Distorted self-image
- Being extremely self-critical
- Having suicidal or self-harming thoughts
- Feeling irritable and/or depressed
- Changes in eating habits
- Sudden change in dietary preferences
- Withdrawing from friends and social events
- Thinning, brittle hair and nails
- Excessive exercise
- Dehydration
- Insomnia
- Fatigue
- Absence of menstruation
- Stomach pain or bloating
- Intentional vomiting or the usage of laxatives or diuretics
- Using diet pills or appetite suppressants
- Eroded teeth or calluses on knuckles from induced vomiting
- Intolerance of cold
Anorexia is generally divided into two subtypes:
- Restrictor type. This patient sets severe limits on their food intake.
- Bulimic type. This patient presents with binging and purging. They eat more than they should and then induce vomiting or take excessive laxatives.
Early treatment is crucial in preventing serious health problems such as heart failure, kidney issues, osteoporosis, substance abuse, and more.
Aside from healthcare providers assessing medical history, lab results, and performing psychological testing, anorexia can be diagnosed based on three criteria listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) published by the American Psychiatric Association.
- Restriction of calorie consumption leading to weight loss or failure to gain weight.
- Intense fear of gaining weight.
- Having distorted views of themselves and their condition.
The biggest challenge with anorexia is that the person suffering may not admit that they are, unless the problem becomes serious enough to become life-threatening. Treatment goals for anorexia include:
- Weight loss stabilization
- Restoration of weight
- Elimination of problematic eating patterns
- Treatment of psychological issues and development of long-term behavioral changes
Nursing Process
Nurses in medical settings may care for patients with anorexia when they are admitted for electrolyte imbalances, heart arrhythmias, and severe malnutrition. Psychiatric nurses may also care for patients with anorexia in instances of suicide attempts, depression, and anxiety. These patients require nonjudgmental support and psychological treatment to learn healthy coping strategies.
Nursing Assessment
Nursing assessment for Anorexia Nervosa focuses on identifying physical, psychological, and behavioral symptoms to ensure effective care. Here are the key components:
1. Health History Review
- Assess for restrictive eating patterns, excessive exercise, or purging behaviors.
- Identify triggers such as stress, societal pressures, or underlying mental health conditions.
- Review the patient’s weight history, including significant weight loss or failure to gain weight.
2. Physical Examination
- Observe for extreme thinness, muscle wasting, or signs of malnutrition.
- Check for vital sign abnormalities, such as bradycardia, hypotension, or hypothermia.
- Evaluate for skin changes, including dry skin, brittle nails, or lanugo (fine hair growth).
3. Behavioral and Psychological Assessment
- Assess for distorted body image and intense fear of weight gain.
- Monitor for obsessive behaviors related to food, calories, or weight.
- Evaluate for coexisting mental health conditions, such as anxiety or depression.
4. Diagnostic Procedures
- Conduct laboratory tests to check for electrolyte imbalances, anemia, or organ dysfunction.
- Review imaging studies (e.g., bone density scans) to assess for osteoporosis.
- Use standardized tools like the Eating Disorder Inventory (EDI) for psychological evaluation.
Nursing Intervention
Nursing interventions for Anorexia Nervosa focus on restoring nutritional balance, addressing psychological factors, and preventing complications. Here are key interventions:
1. Nutritional Support
- Implement a structured meal plan to ensure adequate caloric intake.
- Monitor weight and vital signs regularly to track progress.
- Encourage small, frequent meals to reduce anxiety around eating.
2. Psychological and Emotional Support
- Provide cognitive-behavioral therapy (CBT) to address distorted body image and unhealthy thought patterns.
- Encourage journaling or expressive therapy to help patients process emotions.
- Offer support groups to foster peer encouragement and recovery.
3. Medical Monitoring
- Assess for electrolyte imbalances and administer supplements if needed.
- Monitor for cardiac complications, such as arrhythmias or bradycardia.
- Ensure hydration to prevent dehydration-related complications.
4. Behavioral Interventions
- Set realistic weight goals and reinforce positive behaviors.
- Limit exercise if excessive activity is contributing to weight loss.
- Educate patients on healthy eating habits and the importance of balanced nutrition.
5. Family and Social Involvement
- Involve family members in therapy to create a supportive environment.
- Educate caregivers on early warning signs and relapse prevention.
- Encourage open communication to reduce feelings of isolation.
Nursing Care Plans
Once the nurse identifies nursing diagnoses for anorexia, nursing care plans help prioritize assessments and interventions for both short and long-term goals of care. In the following section, you will find nursing care plan examples for anorexia.
Disturbed Body Image
Patients who suffer from anorexia restrict themselves from eating because they have a distorted view of their outward appearance.
Nursing Diagnosis: Disturbed Body Image
Related to:
- Mental health disorder
- Eating disorder
As evidenced by:
- Seeing themselves as fat even when they are not
- Fear of rejection or reaction by others
- Negative feelings about their body
- Feelings of hopelessness or powerlessness
- Self-harm
- Frequently looking at self in the mirror
- Obsessive weight checking
- Not eating in public
Expected outcomes:
- Patient will verbalize positive feelings about their body.
- Patient will eat meals in the presence of others.
- Patient will participate in therapy and psychological counseling.
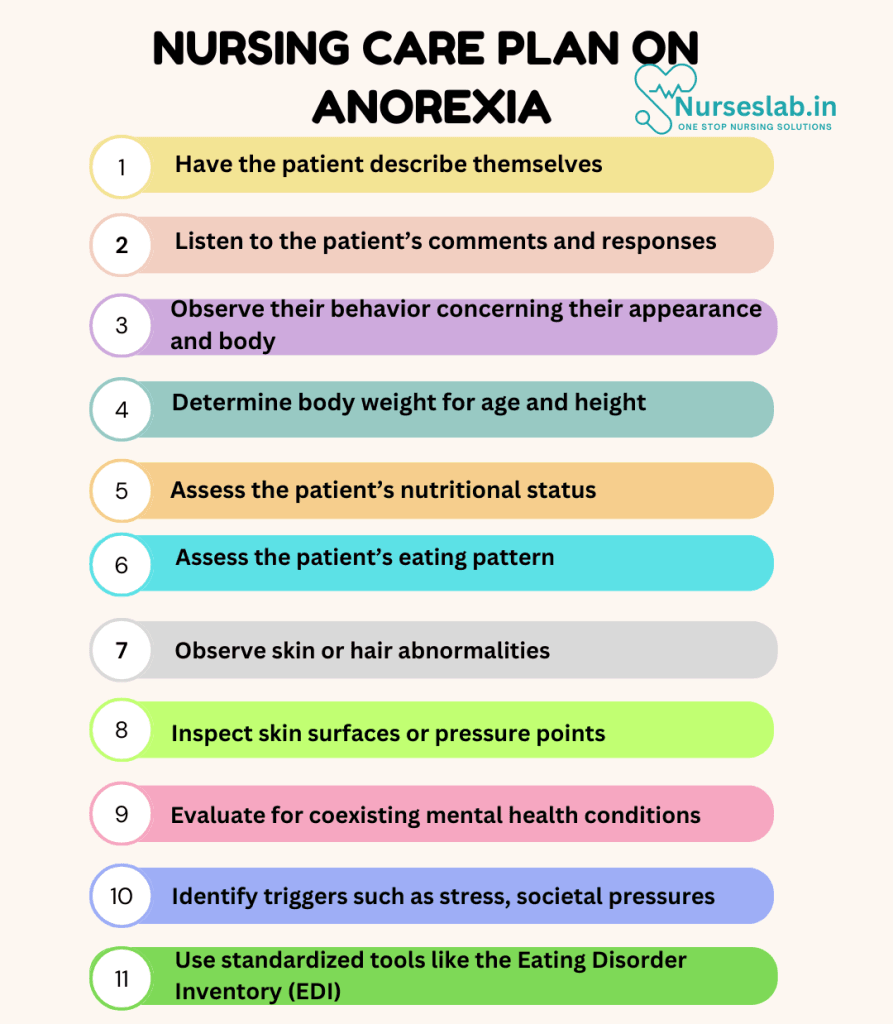
Assessment:
1. Have the patient describe themselves.
Documenting how they see themselves and how they think others see them will help in determining the extent of their body image distortion.
2. Listen to the patient’s comments and responses.
Assess for comments of negative self-talk in general conversation.
3. Observe their behavior concerning their appearance and body.
Ritualistic behaviors such as body-checking or concealment of their appearance provide insight into how the patient feels about themselves.
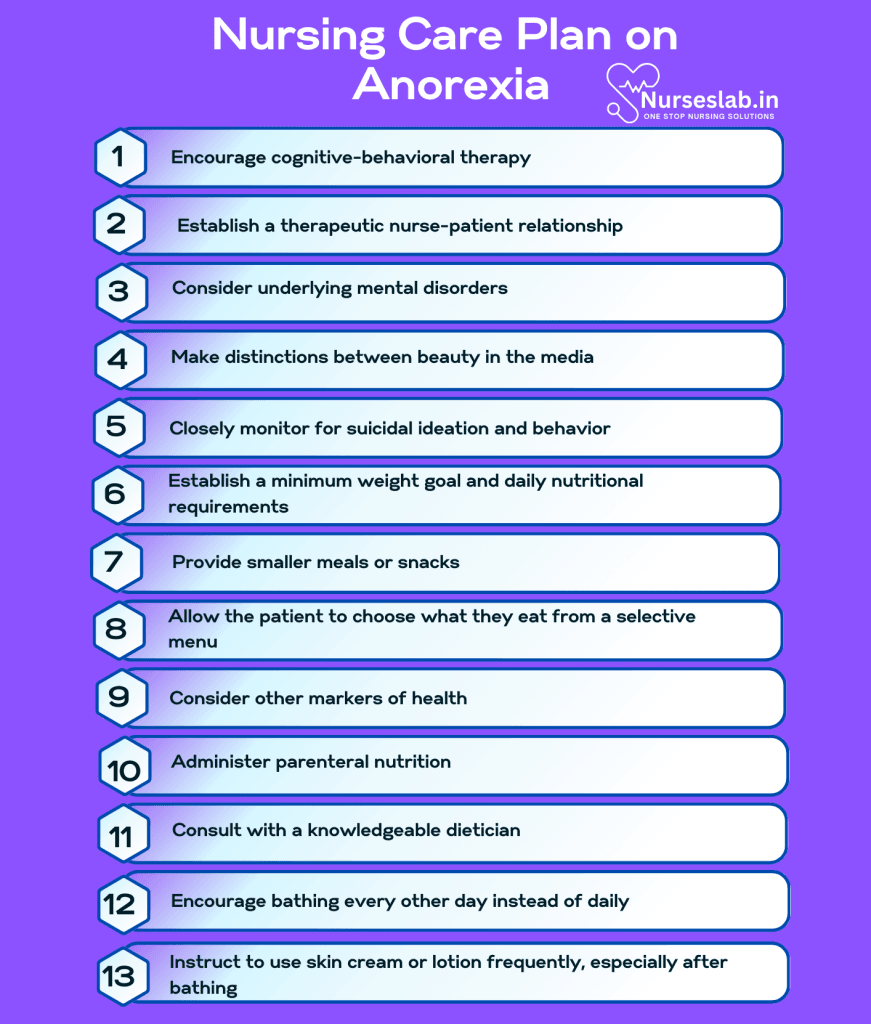
Interventions:
1. Encourage cognitive-behavioral therapy.
This form of therapy helps improve body image by modifying dysfunctional thoughts, feelings, and behaviors.
2. Establish a therapeutic nurse-patient relationship.
Developing an unbiased relationship with the patient will help build trust, which is necessary to treat a chronic eating disorder.
3. Consider underlying mental disorders.
Patients with eating disorders often suffer from personality disorders, severe depression, substance abuse, and more. Treatment of these conditions, along with anorexia, is paramount for long-term success.
4. Make distinctions between beauty in the media.
Adolescents with anorexia may be influenced by TV, magazines, and social media or even by parents or family members. They may feel pressured to appear a certain way. Patients may need to unlearn what they have been taught about unrealistic beauty standards.
5. Closely monitor for suicidal ideation and behavior.
Suicidal thoughts may occur when the patient is experiencing severe anxiety, depression, or hopelessness regarding weight and appearance. Recognition and safety is a priority.
Imbalanced Nutrition: Less Than Body Requirements
Nutritional imbalances can occur in patients suffering from anorexia due to an abnormally low level of nutrients due to a limitation of dietary intake or purging.
Nursing Diagnosis: Imbalanced Nutrition: Less Than Body Requirements
Related to:
- Eating disorder
- Limited food intake
- Malnourishment
- Induced purging
- Excessive exercise
As evidenced by:
- Excessive weight loss
- Fatigue
- Hair loss
- Brittle nails
- Dry skin
- Electrolyte imbalances
- Anemia
- Loss of menses
Expected outcomes:
- Patient will verbalize an understanding of their nutritional needs.
- Patient will display improvement of weight as evidenced by a BMI of at least 19.
- Patient will demonstrate adherence to dietary interventions and treatment.
Assessment:
1. Determine body weight for age and height.
Measuring a person’s weight accurately is the first step in the initial assessment. Weight is used as a basis for caloric and nutritional requirements. BMI may be used by some healthcare professionals.
2. Assess the patient’s nutritional status.
Information about the patient’s initial nutritional status will help identify the problem and its severity. Since anorexic patients do not get adequate nutrients from food, the possibility of malnutrition is extremely high, if not entirely certain. Nutritional imbalances can be visualized through lab tests for electrolytes, protein levels, albumin, and more.
3. Assess the patient’s eating pattern.
Eating patterns are often abnormal in patients suffering from anorexia. An understanding of the patient’s eating pattern will provide baseline data and determine what interventions might be helpful.
Interventions:
1. Establish a minimum weight goal and daily nutritional requirements.
Patients with anorexia are fearful of gaining weight. Instead of providing a weight range that may cause patients to feel their number is “too high,” work towards a minimum weight number.
2. Provide smaller meals or snacks.
Re-introduction to food may be tricky as rapid refeeding may cause gastric dilation, especially after a long period of intense dieting. The patient may also fear large meals and need to start with bites or snacks.
3. Allow the patient to choose what they eat from a selective menu.
This way, the patient is made to feel like they are in control of the situation while helping them gain some confidence, ultimately leading to healthier choices.
4. Consider other markers of health.
Weight isn’t the most important goal. When the patient begins to have better digestion, sex hormones have returned along with menses, energy and sleep are improved, and the patient is mentally stable, they are likely at a stable weight.
5. Administer parenteral nutrition.
Nutritional support can be provided if the caloric intake is insufficient to sustain their metabolic needs. TPN may be required to stabilize electrolytes.
6. Consult with a knowledgeable dietician.
The dietician should be well-versed in treating patients with eating disorders to provide the most helpful and unbiased nutritional support.
Risk for Impaired Skin Integrity
With poor eating habits, patients with anorexia experience nutritional deprivation. This will result in physical changes in the hair, skin, and nails.
Nursing Diagnosis: Risk for Impaired Skin Integrity
Related to:
- Alteration in nutritional state
- Purging
- Emaciation
- Dehydration
As evidenced by:
A risk diagnosis is not evidenced by signs and symptoms as the problem has not yet occurred and the goal of nursing interventions is aimed at prevention.
Expected outcomes:
- Patient will verbalize understanding of how poor nutrient intake affects the skin and hair.
- Patient will demonstrate the prevention of skin breakdown.
- Patient will demonstrate improved hair growth and skin appearance.
Assessment:
1. Observe skin or hair abnormalities.
Assess for thinning hair with breakage, thin, brittle nails, dry, itchy skin, and more that signals poor nutrition.
2. Inspect skin surfaces or pressure points.
Lack of hydration and proper nutrition leads to decreased perfusion and poor circulation. Patients with severe anorexia nervosa may be extremely underweight with bony prominences at an increased risk for pressure sores or skin breakdown.
Interventions:
1. Encourage bathing every other day instead of daily.
Frequent baths contribute to further drying of the skin. Do not scrub the skin with abrasive cleansers or cloths.
2. Instruct to use skin cream or lotion frequently, especially after bathing.
Lotions and creams will aid in lubricating the skin, which will decrease itching. Maintaining soft and smooth skin may also help in boosting their self-esteem.
3. Encourage vitamins.
Biotin is often taken to support hair and nail strength.
4. Educate the patient on the importance of frequent changing of position.
Changing positions will help circulation and prevent sores on bony prominences by avoiding prolonged pressure.
5. Emphasize the importance of adequate fluid intake and proper nutrition.
Improved nutrition and hydration will enhance skin suppleness and elasticity and prevent dryness and cracking.
Nursing Diagnoses and Rationales for Anorexia
1. Imbalanced Nutrition: Less Than Body Requirements
Rationale: Anorexia leads to insufficient nutrient intake, resulting in a negative energy balance that can cause severe weight loss and malnutrition. Regularly monitoring the patient’s weight, dietary intake, and nutritional status is critical. Encouraging small, frequent, nutrient-dense meals and involving a dietitian for personalized meal planning can help address these nutritional deficits.
2. Disturbed Body Image
Rationale: Individuals with anorexia often have a distorted perception of their body size and shape, which fuels their restrictive eating behaviors. Providing psychological support and cognitive-behavioral therapy can help patients develop a healthier body image and reduce the fixation on weight and appearance.
3. Anxiety
Rationale: Anxiety is commonly associated with anorexia, as patients may experience intense fear of gaining weight or losing control over their eating habits. Implementing anxiety-reducing techniques such as relaxation exercises, mindfulness, and therapy can help manage these feelings and improve overall mental health.
4. Risk for Electrolyte Imbalance
Rationale: Restrictive eating and purging behaviors can lead to significant electrolyte imbalances, which pose serious health risks. Monitoring electrolyte levels, educating patients about the dangers of these imbalances, and encouraging balanced nutrition and hydration are essential in preventing complications.
5. Ineffective Coping
Rationale: Anorexia is often a coping mechanism for underlying emotional issues such as low self-esteem, trauma, or perfectionism. Assessing the patient’s coping strategies and providing alternative, healthy coping mechanisms through therapy and support groups can aid in long-term recovery.
6. Low Self-Esteem
Rationale: Individuals with anorexia frequently struggle with feelings of inadequacy and low self-worth. Building self-esteem through positive reinforcement, therapy, and activities that promote self-acceptance and personal achievements can help improve their mental well-being.
7. Social Isolation
Rationale: Anorexia can lead to withdrawal from social activities and relationships, further exacerbating feelings of loneliness and depression. Encouraging participation in social activities, creating a supportive community environment, and facilitating group therapy can help patients reconnect with others and rebuild their support networks.
8. Risk for Cardiac Complications
Rationale: Severe malnutrition and electrolyte imbalances can lead to life-threatening cardiac issues such as arrhythmias and heart failure. Continuous monitoring of cardiac function, providing appropriate medical interventions, and ensuring the patient receives adequate nutrition and electrolyte balance are crucial in preventing these complications.
9. Knowledge Deficit
Rationale: Patients with anorexia may lack understanding of the disease, its effects on the body, and the importance of nutrition for overall health. Providing comprehensive education about anorexia, its consequences, and strategies for healthy eating and recovery is vital in empowering patients to take control of their health.
10. Risk for Self-Harm
Rationale: The psychological distress associated with anorexia can increase the risk of self-harming behaviors. Implementing safety plans, providing mental health support, and closely monitoring the patient for signs of self-harm are essential in ensuring their safety and well-being.
REFERENCES
- Anorexia nervosa. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/anorexia-nervosa/symptoms-causes/syc-20353591.
- Anorexia Nervosa. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/9794-anorexia-nervosa.
- Anorexia Nervosa. Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/eating-disorders/anorexia-nervosa.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
- Bulechek, G. M., Butcher, H. K., Dochterman, J. M., & Wagner, C. M. (2018). Nursing Interventions Classification (NIC) (7th ed.). St. Louis, MO: Elsevier.
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). NANDA International Nursing Diagnoses: Definitions and Classification 2018-2020. New York: Thieme.
- Mehler, P. S., & Andersen, A. E. (2017). Eating disorders: A guide to medical care and complications (3rd ed.). Baltimore, MD: Johns Hopkins University Press.
- National Institute for Health and Care Excellence. (2017). Eating disorders: Recognition and treatment. NICE guideline [NG69]. Retrieved from https://www.nice.org.uk/guidance/ng69
- Yager, J., Devlin, M. J., Halmi, K. A., Herzog, D. B., Mitchell, J. E., Powers, P., & Zerbe, K. J. (2014). Guideline Watch (August 2012): Practice Guideline for the Treatment of Patients with Eating Disorders, 3rd Edition. Focus, 12(4), 416-431.
- Doenges, M. E., Moorhouse, M. F. (1993). Nurses’s Pocket Guide: Nursing Diagnoses with Interventions (4th Ed.). F.A. Davis Company.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.







