Delirium is an acute disturbance of mental status and cognition with an acute onset of hours or days. It is often related to dehydration, infection, medications, alcohol withdrawal, dementia, organ failure, severe pain, or the dying process.
Symptoms may include:
- Reduced awareness of surroundings
- Poor memory
- Disorientation to time or place
- Nonsensical speech
- Restlessness
- Uncooperativeness
- Combativeness
- Withdrawal
- Slow movement
- Altered sleep patterns
There are three types of delirium:
- Hyperactive. Patients are often restless, anxious, have rapid mood swings, or may perceive things that aren’t there. This is the easiest type to recognize but often results in incomplete care and safety concerns due to aggressive or combative behavior.
- Hypoactive. Patients with this type of delirium are sluggish, drowsy, slow, or inactive. They may seem like they are in a daze and communicate less.
- Mixed. The patient may shift between hyperactive and hypoactive.
Older adults with a history of dementia who are admitted to the hospital are at a higher risk of experiencing delirium. Unfamiliar surroundings, medications, surgery, or infection can further exacerbate this.
Delirium is diagnosed through a mental status assessment. A physical or neurological assessment can rule out a possible stroke or other cause that may mimic delirium.
Nursing Process
Nurses play a crucial role in identifying patients experiencing delirium. Because they are the ones that provide round-the-clock bedside care, nurses should be among the first to notice any changes in cognitive behavior in the inpatient setting.
The first step to treatment is to identify the underlying cause. This will prevent further mental status deterioration and reduce safety risks. Nurses can educate family members on identifying signs of delirium.
Nursing Assessment
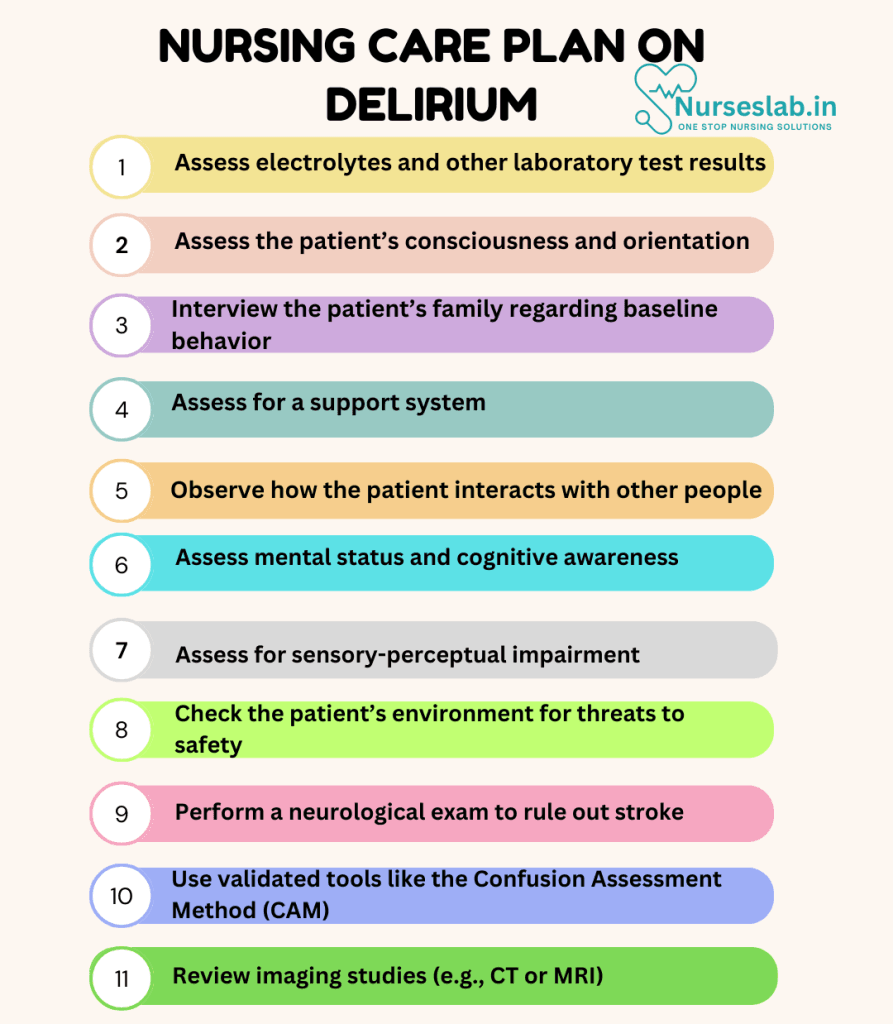
Nursing assessment for Delirium focuses on identifying its underlying causes, monitoring symptoms, and ensuring patient safety. Here are the key components:
1. Health History Review
- Assess for sudden changes in mental status, including confusion, disorientation, or memory impairment.
- Identify potential triggers such as infections, medication side effects, dehydration, or metabolic imbalances.
- Review the patient’s history of substance use, dementia, or other neurological conditions.
2. Physical Examination
- Observe for signs of restlessness, agitation, or lethargy.
- Assess for fluctuations in consciousness and attention span.
- Monitor for hallucinations or delusions, which may indicate hyperactive delirium.
3. Cognitive and Behavioral Assessment
- Use validated tools like the Confusion Assessment Method (CAM) to evaluate delirium.
- Assess the patient’s ability to focus, sustain, or shift attention.
- Evaluate for emotional changes, such as anxiety, irritability, or apathy.
4. Neurological and Systemic Assessment
- Perform a neurological exam to rule out stroke or other brain injuries.
- Monitor vital signs and check for fever, hypoxia, or hypotension, which may contribute to delirium.
5. Diagnostic Procedures
- Conduct laboratory tests to identify electrolyte imbalances, infections, or organ dysfunction.
- Review imaging studies (e.g., CT or MRI) if structural brain abnormalities are suspected.
Nursing Intervention
Nursing interventions for Delirium focus on addressing the underlying cause, ensuring patient safety, and promoting cognitive function. Here are some key interventions:

1. Address Underlying Causes
- Administer prescribed medications to treat infections, metabolic imbalances, or other medical conditions causing delirium.
- Monitor and correct fluid and electrolyte imbalances.
- Collaborate with healthcare providers to adjust medications that may contribute to delirium.
2. Ensure Safety
- Create a calm and structured environment to reduce confusion and agitation.
- Implement fall precautions, such as bed alarms and side rails.
- Supervise patients with severe disorientation to prevent self-harm or injury.
3. Promote Cognitive Function
- Use reorientation techniques, such as providing clocks, calendars, and familiar objects.
- Engage patients in simple, structured activities to stimulate cognitive function.
- Encourage family involvement to provide emotional support and familiarity.
4. Manage Behavioral Symptoms
- Use non-pharmacological approaches like distraction or redirection for agitation.
- Administer sedatives or antipsychotics only if necessary and prescribed.
- Monitor for changes in behavior and adjust interventions accordingly.
5. Educate and Support
- Educate caregivers about the signs and symptoms of delirium and how to manage them.
- Provide emotional reassurance to patients and families.
- Encourage participation in support groups for coping strategies.
Nursing Care Plans
Once the nurse identifies nursing diagnoses for delirium, nursing care plans help prioritize assessments and interventions for both short and long-term goals of care. In the following section, you will find nursing care plan examples for delirium.
Acute Confusion
Delirium results in acute disorientation and disruptions in cognition.
Nursing Diagnosis: Acute Confusion
Related to:
- Alcohol withdrawal
- Medication side effects
- Anaesthesia
- Sleep deprivation
- Older age
- Metabolic imbalances
- Dementia
- Hypoxemia
- Severe pain
As evidenced by:
- Hallucinations
- Fluctuations in cognition
- Agitation
- Restlessness
- Inability to make decisions
- Inability to follow instructions
Expected outcomes:
- Patient will demonstrate appropriate orientation to person and place.
- Patient will cooperate with care and assessments.
- Patient will communicate needs and follow commands.
Assessment:
1. Assess electrolytes and other laboratory test results.
Abnormalities such as metabolic alkalosis, hyponatremia, hypoglycaemia, or any signs of infection can signal an underlying cause of delirium.
2. Assess the patient’s consciousness and orientation.
The nurse can easily and quickly assess this by observing and asking the patient for their name, location, and date.
3. Interview the patient’s family regarding baseline behavior.
Inquiring how the patient typically behaves and speaks can help assess when the delirium started and what is abnormal or out of character.
Interventions:
1. Reorient the patient as needed.
Help to maintain reality and prevent anxiety by orienting to place and time as needed.
2. Provide familiar objects.
Pictures of family members or a favorite blanket may assist in keeping the patient calm and aware.
3. Remain calm and comforting.
Use a calm, reassuring voice and provide touch as long as it doesn’t agitate the patient. Avoid arguing with the patient who is confused.
4. Treat the underlying cause.
An infection may require antibiotics. Severe pain can be treated with opioids. Alcohol withdrawal is treated with anti-anxiety medications. Dehydration requires fluid resuscitation and supplemental electrolytes.
Impaired Social Interaction
Impaired social interaction can happen in patients experiencing delirium due to altered thinking and inappropriate behavior.
Nursing Diagnosis: Impaired Social Interaction
Related to:
- Impaired cognitive functioning
- Altered thought processes
- Biochemical imbalances
As evidenced by:
- Consistent state of disorientation to environment
- Extreme confusion
- Slow/inappropriate response to questions
- Dysfunctional interaction with others
- Inability to focus
- Agitated behavior
- Drowsiness
Expected outcomes:
- Patient will respond appropriately to questions.
- Patient will participate in a group setting within their capabilities.
Assessment:
1. Assess for a support system.
Assess for the presence of family, a spouse, or friends that can assist with communication efforts.
2. Observe how the patient interacts with other people.
The patient may have increased manic behaviors when in a highly-stimulating environment. They may become loud, obscene, or threatening. Identifying environments that make the patient uncomfortable can prevent agitation.
Interventions:
1. Ensure that medications are taken as prescribed.
Some patients may not take medications correctly, either overdosing or underdosing.
2. Provide a calm environment.
Allow the patient to interact with familiar faces by providing an isolated, quiet, and nonstimulating environment.
3. Maintain routines and staff assignments.
Maintaining similar routines, such as eating and bathing schedules, can enhance orientation. If possible, keep the same staff members with the patient to promote communication and trust.
4. Differentiate between delirium and dementia.
Delirium and dementia can occur together or separately, as dementia makes the brain more susceptible to delirium. This can cause delirium to go unrecognized, even for healthcare providers. Delirium is temporary, while dementia is chronic.
Risk for Injury
Since delirium causes disorientation, confusion, and poor decision-making, it poses a significant risk for injury. Ensuring that the patient is safe during the course of recovery is a priority.
Nursing Diagnosis: Risk for Injury
Related to:
- Changes in cognitive function
- Disorientation, confusion
- Unfamiliar environment
As evidenced by:
A risk diagnosis is not evidenced by signs and symptoms as the problem has not occurred yet, and the goal of nursing interventions is aimed at prevention.
Expected outcomes:
- Patient’s family will implement strategies to reduce the risk of injury.
- Patient will remain free of injury.
Assessment:
1. Assess mental status and cognitive awareness.
Changes in mental and cognitive awareness may increase the risk for injury.
2. Assess for sensory-perceptual impairment.
Confused or disoriented patients may have difficulty perceiving environmental stimuli that place them at risk for injuries or falls.
3. Check the patient’s environment for threats to safety.
Patients experiencing cognitive deficits are at risk for common hazards. Clutter, toxic cleaning products, stairs, and easily accessible medications can be hazards.
Interventions:
1. Remain with the patient when agitated or combative.
Staff may need to remain at a distance to prevent injury to themselves, but remaining at the bedside may be necessary to prevent the patient from injuring themselves. Restraints are considered as a last resort.
2. Familiarize them with their environment.
Hospitalization, especially for long durations or associated with surgery or ICU admission, increases the incidence of delirium. Familiarize the patient with their environment and advise on how to call for assistance.
3. Keep items in close reach.
Eyeglasses and hearing aids should be kept close as poor vision and hearing can worsen confusion.
4. Administer antipsychotics.
Patients who are severely combative or uncooperative may require IV or IM medications to induce sedation. Haloperidol is a common medication given to agitated patients to reduce the risk of harm to themselves and others.
Nursing Diagnoses and Rationales for Delirium
1. Acute Confusion
Rationale: Acute confusion is a hallmark of delirium characterized by a sudden onset of altered cognition and attention. This can result from various etiologies including metabolic disturbances, infections, or medication effects. Early recognition and management of acute confusion are essential to prevent worsening of the condition. Frequent cognitive assessments and orientation strategies can help in managing acute confusion.
2. Risk for Injury
Rationale: Patients with delirium are at increased risk for injury due to impaired judgment, disorientation, and potential for wandering. Ensuring a safe environment, including the use of bed alarms, low beds, and close supervision, can mitigate the risk of falls and injuries. Providing a calm and structured environment can also reduce confusion and agitation.
3. Impaired Verbal Communication
Rationale: Delirium can impair a patient’s ability to communicate effectively due to disorganized thinking, attention deficits, and language disturbances. Assessing the patient’s communication abilities and using simple, clear language can facilitate better understanding. Non-verbal communication strategies and involving family members in care can also enhance communication.
4. Disturbed Sleep Pattern
Rationale: Sleep disturbances are common in patients with delirium, which can exacerbate cognitive confusion and agitation. Promoting good sleep hygiene, minimizing nighttime disturbances, and utilizing non-pharmacological interventions for sleep can improve sleep patterns and reduce the severity of delirium.
5. Anxiety
Rationale: Anxiety is often present in patients with delirium due to the fear and confusion associated with the condition. Providing emotional support, explaining the situation clearly, and involving the patient in their care plan can help reduce anxiety. Techniques such as relaxation exercises, and ensuring a familiar environment can also be beneficial.
6. Self-Care Deficit
Rationale: Delirium can impair a patient’s ability to perform activities of daily living independently. Assessing the level of assistance required and providing support for self-care activities are essential. Encouraging participation in care, using adaptive devices, and collaborating with occupational therapy can help maintain the patient’s functional abilities.
7. Social Isolation
Rationale: Patients with delirium may withdraw from social interactions due to confusion and cognitive impairment. Facilitating social engagement, involving family members, and providing opportunities for socialization can reduce feelings of isolation. Structured activities and a supportive environment can also encourage social interaction.
8. Risk for Infection
Rationale: Delirium often accompanies underlying medical conditions that may require invasive procedures or treatments, increasing the risk of infection. Strict adherence to infection control practices, monitoring for signs of infection, and educating the patient and family on infection prevention can help mitigate this risk.
9. Ineffective Coping
Rationale: Patients with delirium may demonstrate ineffective coping mechanisms due to the stress and confusion of their condition. Providing psychological support, teaching coping strategies, and involving mental health professionals can enhance coping skills. Encouraging expression of feelings and offering reassurance can also support the patient’s emotional well-being.
10. Deficient Knowledge
Rationale: Patients and their families may lack understanding of delirium, its causes, and management. Providing education on the nature of delirium, its potential triggers, and the importance of early intervention can empower patients and families. Clear, concise information and encouraging questions are key components of effective education.
REFERENCES
- Doenges, M. E., Moorhouse, M. F. (1993). Nurse’s Pocket Guide: Nursing Diagnoses with Interventions (4th Ed.). F.A. Davis Company.
- Delirium. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/delirium/symptoms-causes/syc-20371386.
- Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2023). Nursing diagnoses handbook: An evidence-based guide to planning care. St. Louis, MO: Elsevier.
- Harding, M. M., Kwong, J., & Hagler, D. (2022). Lewis’s Medical-Surgical Nursing: Assessment and Management of Clinical Problems, Single Volume. Elsevier.
- Herdman, T. H., Kamitsuru, S., & Lopes, C. (2024). NANDA International Nursing Diagnoses – Definitions and Classification, 2024-2026.
- Ignatavicius, D. D., Rebar, C., & Heimgartner, N. M. (2023). Medical-Surgical Nursing: Concepts for Clinical Judgment and Collaborative Care. Elsevier.
- Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014 Mar 8;383(9920):911-22. doi: 10.1016/S0140-6736(13)60688-1. Epub 2013 Aug 28. PMID: 23992774; PMCID: PMC4120864.
- Keenan CR, Jain S. Delirium. Med Clin North Am. 2022 May;106(3):459-469. doi: 10.1016/j.mcna.2021.12.003. Epub 2022 Apr 4. PMID: 35491066.
- Maldonado JR. Acute Brain Failure: Pathophysiology, Diagnosis, Management, and Sequelae of Delirium. Crit Care Clin. 2017 Jul;33(3):461-519. doi: 10.1016/j.ccc.2017.03.013. PMID: 28601132.
- Mattison MLP. Delirium. Ann Intern Med. 2020 Oct 6;173(7):ITC49-ITC64. doi: 10.7326/AITC202010060. PMID: 33017552.
- Silvestri, L. A. (2023). Saunders comprehensive review for the NCLEX-RN examination. St. Louis, MO: Elsevier.
- Bennett, C. (2019). Caring for patients with delirium. Wolters Kluwer Health., Inc.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.







