Pyelonephritis is an infection of the kidneys and is most commonly caused by a bacterial infection of the lower urinary tract. Escherichia coli is considered the most common organism causing pyelonephritis.
Pyelonephritis can be categorized as acute or chronic. Acute pyelonephritis is referred to as an active bacterial infection of the kidneys while the chronic type is repeated infection in the upper urinary tract caused by structural deformities, obstruction, reflux, or urinary stasis.
Signs and Symptoms
The common signs and symptoms of this condition include:
- Flank pain
- Dysuria
- Polyuria
- Urinary urgency
- Urinary frequency
- Malaise
- Fever
- Nausea and vomiting
Complications of pyelonephritis include kidney failure and renal scarring. Pyelonephritis can become life-threatening if untreated and bacteria spreads to the bloodstream causing sepsis.
Urinalysis and urine culture tests are indicated when pyelonephritis is suspected and may show bacteriuria, pyuria, and hematuria. Ultrasound tests and CT scans may be done to determine structural abnormalities, renal abscesses, renal scarring, impaired renal function, or obstructions.
Nursing Process
Patients with mild symptoms are treated with antibiotics for 7 to 14 days in an outpatient setting while patients with severe symptoms require hospitalization and IV antibiotic therapy. Surgical interventions like pyelolithotomy, nephrectomy (for severe cases), or ureteral diversion may be indicated to correct structural issues, drain abscesses, or remove an obstruction.
Nurses support patients with pyelonephritis by providing accurate information about individualized treatment plans including medications, nutrition, and fluid therapies. Nurses are vital in educating patients on how to prevent a recurrence of pyelonephritis.
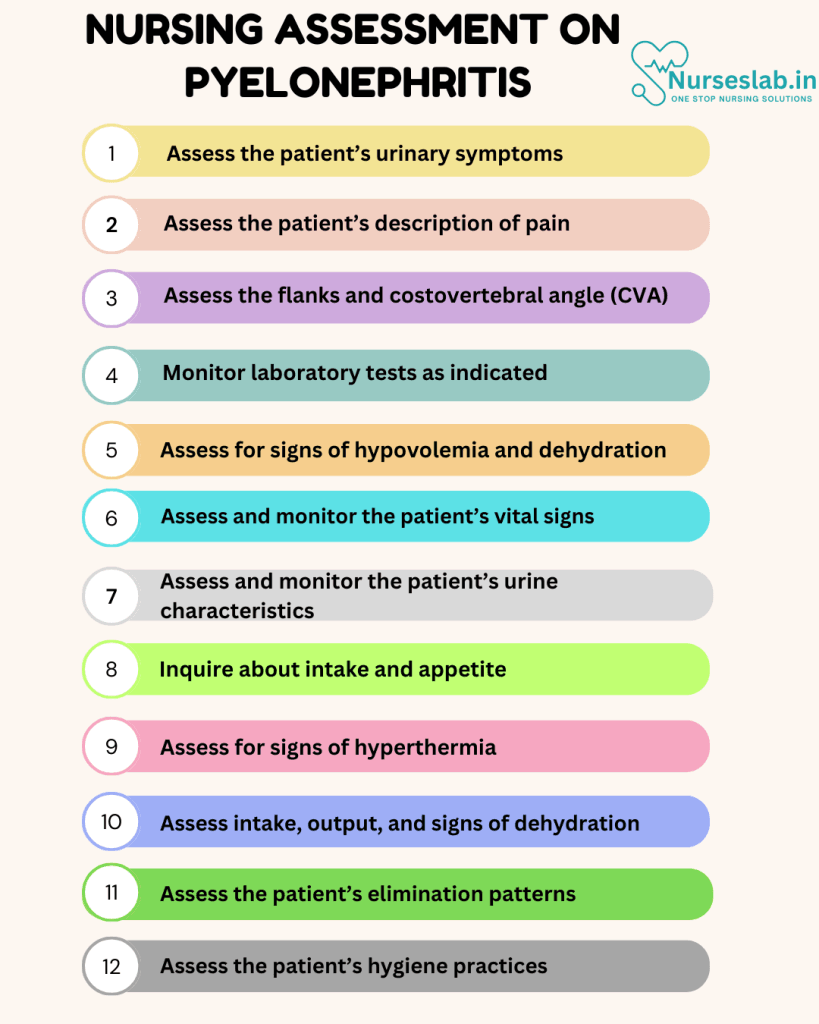
Nursing Assessment
Pyelonephritis is a type of urinary tract infection (UTI) that affects the kidneys. It is a serious condition that can lead to complications if not properly managed. Nurses play a crucial role in the assessment and patients with pyelonephritis, ensuring that they receive comprehensive care that addresses both their physical and emotional needs.
Clinical Signs and Symptoms
Nurses should be vigilant in recognizing the clinical signs and symptoms of pyelonephritis, which may include:
- Fever and chills
- Flank pain or tenderness
- Frequent, painful urination
- Hematuria or blood in the urine
- Nausea and vomiting
- Malaise or general feeling of discomfort
Patient History
A thorough patient history is essential in the assessment of pyelonephritis. Key aspects to inquire about include:
- Previous history of UTIs or kidney infections
- Underlying medical conditions such as diabetes or kidney stones
- Recent urinary procedures or catheter use
- Medication use, particularly antibiotics
- Hydration status and fluid intake
Physical Examination
The physical examination should focus on:
- Vital signs monitoring, especially temperature and blood pressure
- Assessment of flank tenderness through gentle palpation
- Evaluation of urine output and characteristics
Laboratory and Diagnostic Tests
To confirm the diagnosis of pyelonephritis, several laboratory and diagnostic tests may be ordered, including:
- Urinalysis to identify the presence of bacteria, white blood cells, and red blood cells
- Urine culture to determine the specific causative organism and antibiotic sensitivity
- Blood tests such as complete blood count (CBC) and blood cultures to assess for systemic infection
- Imaging studies like ultrasound or CT scan to identify any structural abnormalities or abscess formation
Nursing Interventions
Nursing intervention is critical components in the care of individuals with pyelonephritis. A holistic approach that addresses the physical, emotional, and educational needs of patients is essential in promoting recovery and preventing complications. Through diligent assessment, targeted interventions, and comprehensive education, nurses can play a pivotal role in the management and rehabilitation of patients with pyelonephritis, helping them achieve optimal health outcomes and improve their quality of life.

Medical Management
Medical management of pyelonephritis typically involves:
- Administration of appropriate antibiotics based on culture and sensitivity results
- Analgesics for pain relief
- Antipyretics to manage fever
Hydration and Nutrition
Ensuring adequate hydration and nutrition is critical in the management of pyelonephritis. Nurses should:
- Encourage increased fluid intake to flush out bacteria from the urinary tract
- Monitor fluid balance and ensure adequate hydration
- Provide nutritional support to maintain energy levels and promote healing
Pain Management
Effective pain management strategies include:
- Administration of prescribed analgesics
- Non-pharmacological methods such as warm compresses to the flank area
- Encouraging rest and relaxation techniques
Monitoring and Follow-up
Continuous monitoring and follow-up are essential to ensure the effectiveness of treatment and to detect any complications. Nurses should:
- Regularly assess vital signs and clinical symptoms
- Monitor urine output and characteristics
- Evaluate the patient’s response to antibiotics and adjust the treatment plan as needed
- Provide education on the importance of completing the full course of antibiotics
Nursing Care Plans
Once the nurse identifies nursing diagnoses for pyelonephritis, nursing care plans help prioritize assessments and interventions for both short and long-term goals of care. In the following section, you will find nursing care plan examples for pyelonephritis.
Acute Pain
The most distinctive symptoms of acute pyelonephritis include pain in the back or flank area. The patient may describe suprapubic symptoms of heaviness, pressure, or discomfort.
Nursing Diagnosis: Acute Pain
Related to:
- Inflammation and infection of the urinary tract
As evidenced by:
- Reports of pain/burning/discomfort when urinating
- Dysuria
- Polyuria
- Facial grimace
- Guarding behavior
- Spasm in the bladder and lower back
Expected outcomes:
- Patient will verbalize an absence of flank pain and dysuria.
- Patient will report satisfactory pain control at a level of less than 3 on a scale of 0-10.
Assessment:
1. Assess the patient’s urinary symptoms.
Proper assessment of urinary symptoms can help diagnose pyelonephritis. Common manifestations of pyelonephritis include dysuria, polyuria, frequency, and urgency. Changes in urine odor and color may also indicate bacteriuria.
2. Assess the patient’s description of pain.
Pain associated with pyelonephritis may be described as heaviness, pressure, or discomfort of the back, abdomen, or flank area with or without radiation to the groin. Assess for dysuria or burning with urination.
3. Assess the flanks and costovertebral angle (CVA).
Enlargement, asymmetry, redness, and edema of the flank area can indicate inflammation. Tenderness and discomfort upon percussion on these areas can also indicate infection or inflammation.
4. Monitor laboratory tests as indicated.
Urinalysis indicating pyelonephritis will show a positive leukocyte esterase, presence of white blood cells, bacteria, and occasional protein and red blood cells. A urine culture will help identify specific organisms that are causing the infection. Serum kidney tests like BUN and creatinine can help determine worsening or improving kidney function.
Interventions:
1. Administer medications as indicated.
Antibiotics are prescribed to treat the infection. Antipyretics like acetaminophen are prescribed to help reduce fever and pain.
2. Increase fluids as ordered.
Adequate fluid intake at 2 liters per day will help with urine dilution, promote renal blood flow, reduce bladder irritation, and flush bacteria from the urinary tract.
3. Encourage the patient to avoid urinary tract irritants.
Sodas, spices, tea, alcoholic beverages, and coffee are considered urinary tract irritants and should be avoided.
4. Encourage the patient to void frequently.
Frequent voiding will help to empty the bladder, avoiding bladder distention, reducing urine stasis, preventing reinfection, and lowering bacterial count. Patients may be hesitant to void due to pain but should be educated on these reasons.
5. Assist the patient in using non-pharmacologic techniques for pain management.
Alternative therapies like positioning, heat, relaxation, and guided imagery can help decrease pain, offer distraction, and promote comfort for the patient.
6. Educate the patient about the disease process, prognosis, and treatment regimen.
Patient education is vital to ensure understanding of the disease process and prevention. Stress the importance of completing antibiotic therapy to prevent antibiotic resistance and reinfection.
Deficient Fluid Volume
Pyelonephritis is caused by bacteria that trigger infection and inflammation in the kidneys. As a compensatory mechanism, the kidneys tend to produce more urine which can cause deficient fluid volume and dehydration.
Nursing Diagnosis: Deficient Fluid Volume
Related to:
- Excessive fluid loss
- Disease process
- Diuretic effect
- Inflammatory process
- Insufficient fluid intake
- Inadequate knowledge of fluid needs
- Symptoms of the disease process
As evidenced by:
- Altered mental status
- Altered skin turgor
- Decreased or increased urine output
- Decreased blood pressure
- Dry skin
- Dry mucous membranes
- Increased heart rate
- Increased body temperature
- Thirst
- Loss of appetite
- Weakness
- Diarrhea
- Vomiting
- Nausea
- Fever
- Chills
Expected outcomes:
- Patient will maintain blood pressure, body temperature, and heart rate within normal limits.
- Patient will remain free from any signs and symptoms of dehydration, including dry skin, dry mucous membranes, and altered mental status.
Assessment:
1. Assess for signs of hypovolemia and dehydration.
Pyelonephritis is associated with excessive urine production due to infection and inflammation of the kidneys. Early identification of signs and symptoms of hypovolemia and dehydration (headaches, restlessness, thirst, and inability to concentrate) can help initiate prompt intervention to prevent further complications.
2. Assess and monitor the patient’s vital signs.
Fluid volume deficits can alter the patient’s vital signs causing tachycardia, tachypnea, hypotension, and an increase or decrease in temperature.
3. Assess and monitor the patient’s urine characteristics.
Urine characteristics like dark, concentrated urine with a strong odor signal hypovolemia, developing dehydration, and progression of the disease.
4. Inquire about intake and appetite.
Pyelonephritis commonly causes anorexia and may even cause nausea and vomiting if severe, disrupting intake. Infants may manifest feeding difficulties, fever, and vomiting. Older adults are at a higher risk of experiencing concerning symptoms from fluid volume deficit, such as mental status changes and decompensation to other organ systems.
Interventions:
1. Monitor the patient’s intake and output.
Urine output is an accurate indicator of fluid balance. An increase or decrease in urine output can indicate kidney injury, infection, or inflammation, further complicating hypovolemia and dehydration.
2. Encourage increased fluid intake.
Adequate fluid intake is encouraged in patients with pyelonephritis, as this condition is characterized by excessive urine production due to infection and inflammation of the kidneys. Adequate fluid intake helps with fluid replacement and prevents dehydration.
3. Administer intravenous fluid therapy as indicated.
For severe cases of pyelonephritis, the patient may need to be admitted to the hospital with intravenous fluid replacement to resolve deficient fluid volume and prevent dehydration.
4. Prevent further fluid loss.
Patients who exhibit fever, vomiting, or diarrhea require antipyretics, antiemetics, and antidiarrheals to prevent further fluid loss.
5. Monitor for complications.
Pyelonephritis can result in urosepsis which is characterized by bacteriuria and bacteremia. It is vital to closely monitor and observe the patient for signs and symptoms of septic shock to prevent further decline in the patient’s intravascular volume.
Hyperthermia
Fever or hyperthermia is a common symptom of pyelonephritis. The triad signs of this acute infection include fever, costovertebral angle pain, and nausea and vomiting, though these may not occur in all patients or all together.
Nursing Diagnosis: Hyperthermia
Related to:
- Inflammatory process secondary to pyelonephritis
- Infectious process secondary to pyelonephritis
As evidenced by:
- Increased body temperature above the normal range
- Chills
- Warm, flushed skin
- Diaphoresis
- Tachycardia
- Tachypnea
Expected outcomes:
- Patient will maintain core body temperature within the normal range.
- Patient will maintain vital signs within normal limits.
Assessment:
1. Assess for signs of hyperthermia.
Assess signs and symptoms of hyperthermia including weakness, tachycardia, headache, irritability, and malaise to determine potential complications or deterioration.
2. Assess and monitor vital signs.
Changes in vital signs including tachycardia and hypertension indicate progression of hyperthermia.
3. Assess intake, output, and signs of dehydration.
Hyperthermia can result in dehydration. Signs and symptoms of dehydration include thirst, poor skin turgor, dry oral membranes, weak and fast pulse, decreased urine output, and increased urine concentration.
Interventions:
1. Provide a tepid sponge bath as needed
A sponge bath with tepid water will reduce fever by dilating the superficial blood vessels, ultimately releasing heat and lowering body temperature. Do not induce shivering as this is the body’s attempt to increase temperature.
2. Encourage adequate fluid intake.
Adequate fluid intake will help prevent dehydration, which is precipitated by the increase in body temperature.
3. Maintain bed rest.
Adequate rest allows the reduction of metabolic demands and oxygen consumption, resulting in a decrease in body temperature.
4. Administer antipyretic medications as indicated.
Antipyretic medications reduce prostaglandin synthesis to lower body temperature.
Impaired Urinary Elimination
Impaired urinary elimination can be a result of sensory impairment, physical abnormality, or a secondary cause of another disorder. This can happen in patients with pyelonephritis due to symptoms of the condition such as frequent urination, a strong, persistent urge to urinate, and urinary hesitancy.
Nursing Diagnosis: Impaired Urinary Elimination
Related to:
- Kidney infection and inflammation
- Weakened bladder muscles
- Anatomic obstruction
As evidenced by:
- Urinary hesitancy
- Urinary retention
- Urinary incontinence
- Urinary urgency
- Dysuria
- Frequent voiding
- Nocturia
Expected outcomes:
- Patient will achieve a normal urinary elimination pattern, as evidenced by the absence of urinary frequency, urgency, and hesitancy.
- Patient will establish lifestyle techniques to prevent urinary infections.
Assessment:
1. Assess the patient’s elimination patterns.
The patient’s elimination patterns can offer insight into causes of infection such as incontinence, delayed urination, or incomplete urination.
2. Assess the patient’s hygiene practices.
Inquire about the patient’s understanding of hygiene in relation to urinary elimination. The patient should be instructed to urinate after sexual activity, wipe front to back after bathroom use, and clean the perineal area daily to avoid infections of the urinary tract.
Interventions:
1. Measure intake and output accurately.
A record of the patient’s intake and output can help determine changes in urine characteristics (amount and concentration), which can indicate the progression of pyelonephritis.
2. Instruct the patient to void every 2-3 hours.
This will help to empty the bladder and prevent the buildup of urine. Bladder training helps in reducing urine leakage and a sense of urgency by increasing the amount of fluid the bladder holds and the time between emptying of the bladder.
3. Check for distention with a bladder scanner.
This can help determine bladder distention or incomplete emptying after urination.
4. Encourage increased fluid intake.
Adequate fluid intake promotes hydration, increases urine production, and flushes out bacteria from the urinary tract system. Patients with incontinence issues can be hesitant to drink enough which creates an environment for dehydration and urinary infection.
5. Facilitate a comfortable voiding position, making use of urinals or bedpans as needed.
Discomfort can affect the patient’s elimination patterns. Offer urinary devices frequently for the patient who cannot communicate to support urination.
Risk for Electrolyte Imbalance
Kidney problems like pyelonephritis cause a decline in kidney function and increase the risk of developing electrolyte imbalances. Symptoms of the disease, including diarrhea, vomiting, fever, and frequent urination, also contribute to electrolyte abnormalities.
Nursing Diagnosis: Risk for Electrolyte Imbalance
Related to:
- Compromised regulatory mechanism
- Disease process
- Inflammatory process
- Inability of the kidneys to filter effectively
- Renal dysfunction
- Symptoms of condition
- Alterations in urination
As evidenced by:
A risk diagnosis is not evidenced by signs and symptoms as the problem has not yet occurred. Nursing interventions are aimed at prevention.
Expected outcomes:
- Patient will experience cessation of symptoms such as fever, diarrhea, and vomiting.
- Patient will maintain vital signs and cardiac rhythm within normal limits.
Assessment:
1. Assess and monitor the patient’s electrolyte levels.
Pyelonephritis often causes hyponatremia and hyperkalemia. Frequent potassium and sodium level evaluation is necessary to monitor the progression of the disease and provide prompt interventions to balance electrolytes.
2. Assess and monitor the patient’s vital signs.
Since patients with pyelonephritis are at risk for developing electrolyte imbalances like hyperkalemia, it is crucial to assess and monitor their vital signs. Hyperkalemia can cause life-threatening cardiac arrhythmias, tachypnea, decreased heart rate, and weak pulses.
3. Assess the patient’s neurologic status and level of consciousness.
Imbalances in electrolytes like sodium, potassium, magnesium, and calcium can cause neurological symptoms like seizures, confusion, muscle weakness, cramps, and tetany.
Interventions:
1. Encourage adequate fluid intake as indicated.
Adequate fluid intake of about 6-8 glasses of water is essential in patients with pyelonephritis as it can help flush bacteria out of the urinary system and prevent dehydration.
2. Administer antibiotic therapy as ordered.
Antibiotic therapy is indicated for patients with pyelonephritis to help clear out infection and inflammation in the urinary system, reducing the risk for electrolyte imbalances as the kidneys can return to their normal filtration functions.
3. Monitor the effects of current medications.
Certain medications like diuretics and cardiac medications can affect the patient’s fluid and electrolyte balance. It is vital to review and monitor the patient’s medication regimen so changes can be initiated to prevent further decline in electrolyte balance.
4. Alleviate symptoms.
Pyelonephritis can cause fever, chills, diarrhea, and vomiting, leading to dehydration and alterations in electrolytes. Control symptoms through antipyretics, antiemetics, antidiarrheals, and electrolyte replacement therapy.
5. Educate the patient and family about symptoms of electrolyte alterations.
Hyponatremia is common in pyelonephritis, and this is typically manifested as muscle cramps, lethargy, nausea, and altered mental status, while hyperkalaemia manifests as restlessness, muscle weakness, and diarrhoea. Children and infants are at a higher risk of experiencing severe effects of dehydration, infection, and electrolyte abnormalities.
Nursing Diagnosis and Rationale for Pyelonephritis
1. Acute Pain
Rationale: Pyelonephritis often presents with intense flank and abdominal pain due to inflammation and infection of the kidneys. Nurses should assess the location, intensity, and duration of pain, and administer prescribed analgesics. Non-pharmacological interventions such as heat application and relaxation techniques may also help alleviate discomfort.
2. Impaired Urinary Elimination
Rationale: The infection can lead to symptoms such as dysuria, frequency, urgency, and hematuria. Nurses should monitor urine output, characteristics, and report any significant changes. Educating patients about the importance of completing the full course of antibiotics and proper hydration can facilitate effective urinary elimination and reduce the risk of recurrence.
3. Risk for Fluid Volume Deficit
Rationale: Fever, vomiting, and increased urinary output associated with pyelonephritis can lead to dehydration. Nurses should monitor fluid intake and output, encourage oral hydration, and administer intravenous fluids when necessary. Assessing for signs and symptoms of dehydration, such as dry mucous membranes and decreased skin turgor, is crucial.
4. Hyperthermia
Rationale: Pyelonephritis often causes high fever due to the body’s response to infection. Nurses should regularly monitor the patient’s temperature, administer antipyretics as ordered, and implement cooling measures such as tepid sponge baths. Encouraging adequate fluid intake can also help manage fever.
5. Risk for Sepsis
Rationale: Severe pyelonephritis can lead to systemic infection and sepsis. Nurses should be vigilant for signs of systemic infection such as increased heart rate, low blood pressure, and altered mental status. Timely administration of antibiotics, close monitoring of vital signs, and prompt reporting of any deterioration are essential in preventing sepsis.
6. Deficient Knowledge
Rationale: Patients may lack knowledge about pyelonephritis, its causes, and treatment. Nurses should provide education on the importance of medication adherence, recognizing symptoms of recurrence, and lifestyle modifications to prevent future infections. Visual aids and written instructions can enhance understanding.
7. Anxiety
Rationale: The sudden onset of symptoms and potential complications of pyelonephritis can cause anxiety. Nurses should offer emotional support, provide information about the condition and its treatment, and create a calming environment to help reduce anxiety. Referral to counseling services may be beneficial for some patients.
REFERENCES
- Acute Pyelonephritis. Copyright © 1994-2022 by WebMD LLC. https://emedicine.medscape.com/article/245559-overview
- Belyayeva M, Jeong JM. Acute Pyelonephritis. [Updated 2021 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519537/
- Bono MJ, Reygaert WC, Doerr C. Urinary Tract Infection (Nursing) [Updated 2021 Jun 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK568701/
- Lewis’s Medical-Surgical Nursing. 11th Edition, Mariann M. Harding, RN, PhD, FAADN, CNE. 2020. Elsevier, Inc.
- Medical-Surgical Nursing: Concepts for Interprofessional Collaborative Care. 9th Edition. Donna D. Ignatavicius, MS, RN, CNE, ANEF. 2018. Elsevier, Inc.
- Pyelonephritis: Kidney infection. National Kidney and Urologic Diseases Information Clearinghouse. https://www.niddk.nih.gov/health-information/kidney-disease/kidney-infection-pyelonephritis
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.







