Mental health is an essential aspect of overall health and involves a person’s psychological, emotional, and social well-being. It affects the way a person feels, thinks, and acts and determines how a person relates to others, handles stress, and makes decisions.
Mental health problems or illnesses can arise anytime throughout a person’s life. Various factors give rise to mental health illnesses including biological factors like genes, environmental factors such as toxins, alcohol, and drugs, family history of mental health illnesses, and life experiences like abuse or trauma.
Signs and symptoms of mental health problems include:
- Sadness
- Inability to concentrate
- Excessive fear
- Excessive guilt
- Withdrawal from society
- Extreme mood changes
- Detachment from reality
- Inability to cope with problems
- Trouble relating to other people or situations
Fortunately, discussions surrounding mental health are becoming more common and resources are readily available to manage mental health disorders.
Nursing Process
Physical assessments, laboratory tests like thyroid tests and drug or alcohol screening, and psychological evaluations are conducted to help diagnose or rule out mental health problems.
While it can be difficult to determine the type of mental health problem a person has, an accurate diagnosis will help guide the most appropriate treatment for the patient.
Medications like antidepressants, mood stabilizers, and antipsychotic drugs are prescribed to help improve symptoms. Psychotherapy, brain-stimulation treatments, and inpatient treatment programs may also be indicated.
Nurses, regardless of specialty, care for patients who display signs of or are at risk of developing mental health problems. Nurses are instrumental in the assessment, management, education, and collaboration of a patient’s mental health.
Nursing Assessment
Mental health is a critical component of overall well-being, affecting how individuals think, feel, and behave. Nurses play a vital role in assessing and promoting mental health, helping to identify and manage mental health disorders, and supporting patients in achieving better mental health outcomes. This document outlines a comprehensive approach to nursing assessment on mental health, covering key areas such as patient history, observation, interview techniques, and the use of standardized assessment tools.

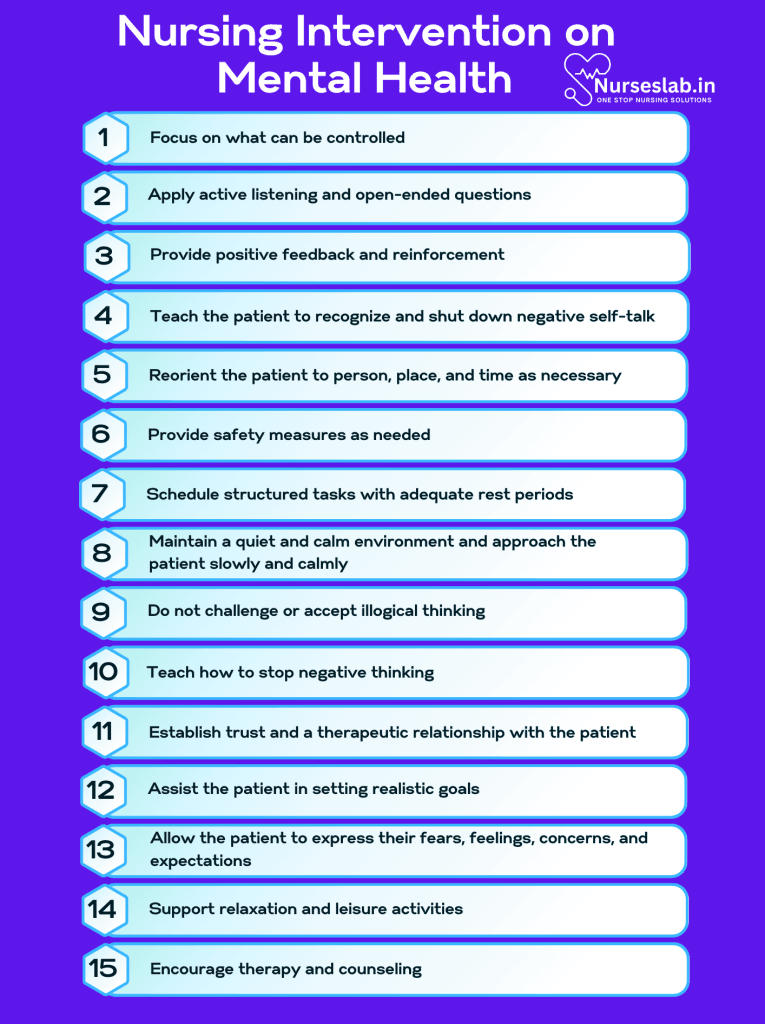
Nursing Interventions
Nurses play a crucial role in the care and support of individuals with mental health conditions. By identifying potential risks and providing targeted interventions, nurses can promote mental well-being and improve the quality of life for patients and their families.
Nursing Care Plans
Once the nurse identifies nursing diagnoses related to mental health conditions, nursing care plans help prioritize assessments and interventions for both short and long-term goals of care. In the following section, you will find nursing care plan examples related to mental health conditions.
Chronic Low Self-esteem
Chronic low self-esteem refers to a long-standing negative perception of self-worth and personal abilities. Low self-esteem may be experienced by patients with various mental health disorders such as anxiety disorders, eating disorders, major depressive disorders, and alcohol and drug abuse.
Nursing Diagnosis: Chronic Low Self-esteem
Related to:
- Disturbed body image
- Fear of rejection
- Inadequate social support
- Ineffective communication skills
- Insufficient approval from others
- Low self-efficacy
- Abandonment
- Domestic abuse
As evidenced by:
- Depressive symptoms
- Excessive shame or guilt
- Constant seeking of reassurance
- Hopelessness
- Insomnia
- Loneliness
- Passive behavior
- Overly-conforming behaviors
- Reduced eye contact
- Rejects positive feedback
- Reports repeated failures
- Self-negating verbalizations
Expected Outcomes:
- The patient will verbalize an increased sense of self-worth
- The patient will demonstrate behaviors of improved self-esteem such as eye contact, appropriate physical appearance, posture, and participation in conversations
Assessment:
1. Assess the patient’s past and current achievements.
This shows the patient a more realistic view of his or her strengths and capabilities. Patients with mental health conditions may lose sight of their past accomplishments and tend to exhibit low self-esteem.
2. Assess how the patient views themselves.
Assess for negative self-talk and exaggerated feelings of one’s self. The goal isn’t to reject the patient’s feelings but to gain insight into their view of themself.
3. Assess support systems.
A lack of support can contribute to poor self-worth. A present support system that is degrading or harmful to the patient’s self-esteem may require intervention.
4. Assess for suicidal ideation.
Patients with chronic low self-esteem may have suicidal thoughts or a plan. Ask directly if the patient is thinking of killing or harming themselves.
Interventions:
1. Focus on what can be controlled.
A chronic sense of failure may need to be overcome. The patient may feel that their every action or entire life is a failure. Attempt to have the patient focus only on what can be controlled, and that what may be deemed a “failure” does not have to be tied with one’s sense of self.
2. Apply active listening and open-ended questions.
Therapeutic communication is an important aspect of providing care and support to patients suffering from mental health problems. Communication methods like active listening and using open-ended questions enable the patient to verbalize interests, worries, concerns, and thoughts without interruption.
3. Provide positive feedback and reinforcement.
Continuous positive feedback and support promote the patient’s self-esteem and self-worth. In time, the patient will hopefully begin to believe and be a source of their own positive feedback.
4. Teach the patient to recognize and shut down negative self-talk.
Recognition of negative thoughts enables the patient to develop new ways of coping. The patient can be taught to replace negative ideas and beliefs with positive affirmations.
Disturbed Thought Processes
Mental health problems affect a person’s mood, thoughts, and behavior. Certain mental health disorders may result in disturbed thought processes where the patient experiences alterations in cognition, perception, reasoning, and problem-solving, interfering with their daily life.
Nursing Diagnosis: Disturbed Thought Processes
Related to:
- Altered self-concept
- Cognitive dysfunction
- Low self-esteem
- Psychological barriers
- Anxiety
- Fear
- Stressors
- Substance misuse
- Unaddressed trauma
- Social Isolation
As evidenced by:
- Absence of eye contact
- Inaccurate interpretation of stimuli (external or internal)
- Decreased willingness to participate in social interactions
- Difficulty comprehending communication
- Inappropriate social behavior
- Cognitive dissonance
- Inappropriate verbalization
- Speech abnormalities
- Hallucinations/delusions
- Distractibility
- Suspiciousness
Expected Outcomes:
- The patient will maintain reality orientation and communicate and interact with other people according to social norms
- The patient will recognize and implement strategies to manage hallucinations/delusions
Assessment:
1. Assess the patient’s past medical history and identify factors present.
Proper assessment of the patient’s medical history and factors contributing to the patient’s condition is important to help plan the best treatment regimen. Conditions such as dementia, anoxic brain injuries, and schizophrenia may cause disturbed thought processes and all have very different treatments.
2. Assess and review laboratory values.
Mental health problems can be caused by biochemical imbalances. Abnormal laboratory values like hypokalaemia, anaemia, signs of infection, or metabolic alkalosis can indicate causative factors of the patient’s condition.
3. Assess the patient’s cognitive ability.
This will help determine the patient’s ability to participate in the plan of care and treatment regimen.
Interventions:
1. Reorient the patient to person, place, and time as necessary.
When a patient is unable to maintain reality orientation, it can cause anxiety or worsening confusion. Consistent reorientation allows the patient to develop a sense of control and builds a trusting relationship with the healthcare provider.
2. Provide safety measures as needed.
It is always important to consider the patient’s safety at all times since mental health problems can affect the patient’s reactions to external stimuli. Safety measures include side rails, close supervision, or seizure precautions as indicated.
3. Schedule structured tasks with adequate rest periods.
This will help provide adequate stimulation and appropriate treatment interventions while allowing the patient to rest to reduce fatigue.
4. Maintain a quiet and calm environment and approach the patient slowly and calmly.
Patients with disturbed thought processes may respond with exaggerated or aggressive behaviors if overstimulated.
5. Do not challenge or accept illogical thinking.
Patients who express delusions should not have their reality challenged, but the nurse can offer understanding of what the patient is experiencing while maintaining reality.
6. Teach how to stop negative thinking.
Teach the patient strategies such as stating “stop!” or a loud noise such as clapping to interrupt unwanted thoughts.
Ineffective Coping
Patients suffering from mental health disorders may fail to effectively deal with existing problems due to unmanaged stress, poor coping skills, or other life pressures.
Nursing Diagnosis: Ineffective Coping
Related to:
- Inadequate confidence in the ability to deal with a situation
- Inadequate sense of control
- Inadequate social support
- Ineffective tension release strategies
- Inadequate resources
As evidenced by:
- Altered attention
- Altered communication pattern
- Destructive behaviors
- Difficulty organizing information
- Inability to ask for help
- Lack of goal-directed behavior
- Inadequate follow-through
- Inadequate problem-solving skills
- Substance abuse
Expected Outcomes:
- The patient will demonstrate effective coping when faced with unfavorable situations
- The patient will verbalize confidence in dealing with psychosocial issues
Assessment:
1. Assess history of coping.
The nurse can first assess how the patient has coped in the past with difficult situations. The patient may not be equipped with the necessary skills and strategies to cope effectively.
2. Assess for possible causes of ineffective coping.
Lack of problem-solving skills, poor self-concept, lack of social support, or stressors such as finances, living environment, or career pressures will each require their own specific strategies.
3. Assess for destructive habits.
Ineffective coping may be made worse by the use of drugs, alcohol, overeating, sexual behavior, smoking, and more that require treatment.
Interventions:
1. Establish trust and a therapeutic relationship with the patient.
An unbiased attitude establishes trust. An open and patient tone will reduce feelings of isolation and ultimately facilitate coping.
2. Assist the patient in setting realistic goals.
Patients may feel helpless in goal setting especially if they never reach goals. Instruct the patient on how to set short, manageable goals.
3. Allow the patient to express their fears, feelings, concerns, and expectations.
Verbalization of perceived or actual threats can help reduce anxiety and promote open communication with the patient. These should be met without judgment from the healthcare team.
4. Support relaxation and leisure activities.
Coping with stress, grief, or other mental health issues requires time for hobbies, exercise, and distraction. Remind the patient to take time to read, write, walk, and enjoy activities.
5. Encourage therapy and counseling.
Mental health professionals can help the patient learn and implement healthy coping mechanisms.
Nursing Diagnosis with Rationale for Mental Health
1. Risk for Self-Harm
Rationale: Individuals with mental health issues such as depression, anxiety, or other mood disorders may experience heightened feelings of worthlessness, hopelessness, or distress, increasing the risk of self-harm. Nurses should closely monitor for signs of self-injurious behavior, provide a safe environment, and offer therapeutic interventions such as counseling and support groups. Educating patients and families about coping strategies and warning signs is also essential.
2. Risk for Ineffective Coping
Rationale: Mental health conditions often impair an individual’s ability to manage stressors effectively. Nurses should assess the patient’s coping strategies, identify maladaptive behaviors, and teach stress management techniques. Providing support through therapeutic communication and connecting patients with community resources can help improve their coping mechanisms.
3. Risk for Social Isolation
Rationale: Mental health issues can lead to withdrawal from social interactions and activities, exacerbating feelings of loneliness and isolation. Nurses should encourage social engagement by identifying and facilitating participation in support groups, community activities, or therapy sessions. They should also educate patients and their families on the importance of maintaining social connections.
4. Risk for Noncompliance with Treatment Regimen
Rationale: Individuals with mental health conditions may struggle with adhering to their treatment plans due to various factors such as forgetfulness, lack of understanding, or side effects of medications. Nurses should provide comprehensive education on the importance of treatment adherence, simplify medication regimens when possible, and involve patients in decision-making. Regular follow-up and support can enhance compliance.
5. Risk for Impaired Self-Esteem
Rationale: Mental health conditions can significantly impact an individual’s self-worth and confidence. Nurses should assess the patient’s self-esteem, provide positive reinforcement, and encourage participation in activities that promote a sense of accomplishment and self-worth. Therapy and counseling can also be beneficial in addressing underlying issues affecting self-esteem.
6. Risk for Disturbed Sleep Pattern
Rationale: Sleep disturbances are common in individuals with mental health conditions. Nurses should assess the patient’s sleep patterns, identify contributing factors, and implement interventions such as establishing a regular sleep routine, creating a conducive sleep environment, and addressing any underlying medical or psychological issues. Educating patients on sleep hygiene practices is also important.
7. Risk for Impaired Family Processes
Rationale: Mental health conditions can strain family relationships and dynamics. Nurses should assess the family’s functioning, provide education on the mental health condition, and involve family members in the patient’s care plan. Offering resources such as family therapy or support groups can help improve communication and support within the family unit.
8. Risk for Knowledge Deficit
Rationale: Patients and their families may lack understanding of the mental health condition, treatment options, and available resources. Nurses should provide clear and concise education tailored to the patient’s and family’s needs, using language that is easily understood. Providing written materials, visual aids, and opportunities for questions can enhance understanding and engagement.
REFERENCES
- About Mental Health Problems. Mental Health Foundation. 2022. https://www.mentalhealth.org.uk/explore-mental-health/about-mental-health-problems
- Mental Disorders. World Health Organization. 2022. https://www.who.int/news-room/fact-sheets/detail/mental-disorders
- Moitra M, Santomauro D, Collins PY, Vos T, Whiteford H, et al. (2022) The global gap in treatment coverage for major depressive disorder in 84 countries from 2000–2019: A systematic review and Bayesian meta-regression analysis. PLOS Medicine 19(2): e1003901. https://doi.org/10.1371/journal.pmed.1003901
- Psychiatric Mental Health Nursing Concepts of Care and Evidence-Based Practice. 8th Edition. Mary C. Townsend, DSN, PMHCNS-BC. 2015. FA Davis Company.
- What is Mental Health? MentalHealth.gov. Last Updated: 02/28/2022. https://www.mentalhealth.gov/basics/what-is-mental-health
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.







