Aortic dissection is a rare but potentially fatal condition that demands prompt recognition and treatment. Characterized by a tear in the inner layer of the aorta—the body’s largest artery—this medical emergency can quickly lead to severe complications, including organ failure and death. Understanding its pathophysiology, risk factors, clinical presentation, diagnostic approaches, and management strategies is essential for clinicians and crucial for public awareness.
Introduction
The aorta is the primary artery carrying oxygenated blood from the heart to the rest of the body. Due to the high-pressure blood flow and the vital nature of the organs it supplies, any compromise to its structural integrity, such as an aortic dissection, can have devastating consequences. Although aortic dissection is relatively uncommon, its sudden onset and rapid progression make it a leading cause of cardiovascular mortality after heart attack and stroke among non-traumatic causes.
Pathophysiology
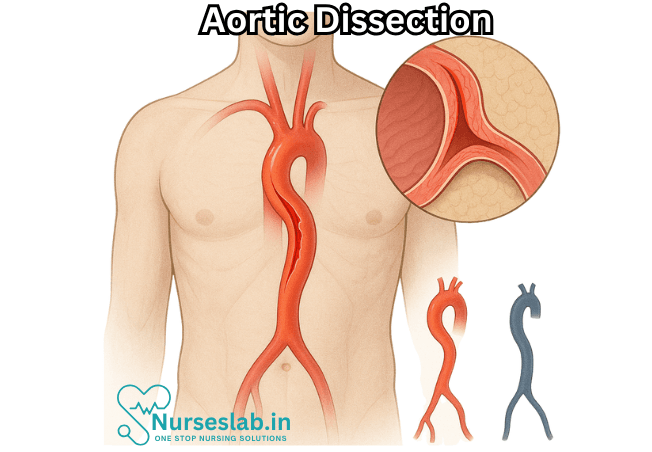
Aortic dissection occurs when a tear develops in the innermost layer (intima) of the aorta. Blood surges through this tear, separating (dissecting) the inner and middle layers (media) of the arterial wall. This creates a false lumen a new channel within the aortic wall which may extend along the length of the vessel. The process can obstruct blood flow to vital organs, rupture outward, or involve major branches of the aorta, all of which can be catastrophic.
There are two primary classification systems for aortic dissection:
Stanford Classification:
- Type A: Involves the ascending aorta (may extend to the arch or descending aorta)
- Type B: Involves only the descending aorta (distal to the left subclavian artery)
DeBakey Classification:
- Type I: Originates in the ascending aorta, propagates to at least the aortic arch and often beyond
- Type II: Confined to the ascending aorta
- Type III: Originates in the descending aorta, rarely extends proximally
Risk Factors
Several risk factors predispose individuals to aortic dissection, including:
- Chronic hypertension (the most significant risk factor)
- Connective tissue disorders (e.g., Marfan syndrome, Ehlers–Danlos syndrome)
- Bicuspid aortic valve
- Pre-existing aortic aneurysm
- Congenital heart disease
- Family history of aortic disease
- Age (most common in people aged 60–80, but those with connective tissue disorders may present younger)
- Male sex (higher prevalence, though anyone can be affected)
- Cocaine or stimulant use
- Pregnancy (especially in the third trimester, though rare)
- Iatrogenic causes (procedures involving the aorta, such as cardiac surgery or catheterization)
Understanding these factors highlights the importance of routine monitoring and risk assessment, particularly in individuals with hereditary syndromes or chronic hypertension.
Clinical Presentation
The classic symptom of aortic dissection is sudden, severe chest or back pain, often described as “tearing” or “ripping.” However, symptoms can vary dramatically, leading to misdiagnosis.
- Chest pain (anterior for Type A, interscapular for Type B)
- Back or abdominal pain
- Syncope (fainting)
- Shortness of breath
- Stroke-like symptoms (if cerebral vessels are involved)
- Weak or absent pulse in one arm or leg compared to the other
- Signs of shock (hypotension, sweating, pallor)
- Paralysis or limb ischemia
Because the dissection can disrupt blood flow to any branch of the aorta, the symptoms may mimic those of a heart attack, stroke, or even gastrointestinal issues, which complicates rapid diagnosis.
Diagnosis
Due to the high mortality rate—especially in the first 48 hours—rapid diagnosis is crucial. The following steps and tools are used:
History and Physical Examination
A detailed history and physical exam can reveal important clues, such as characteristic pain or differences in blood pressure between limbs. Pulse deficits or a new heart murmur may be detected if the dissection involves the aortic valve.
Imaging Modalities
- Computed Tomography Angiography (CTA): The gold standard due to its speed, accuracy, and widespread availability. It provides detailed images of the aorta and major branches.
- Transesophageal Echocardiography (TEE): Useful, especially in unstable patients or where CTA is unavailable. Provides real-time images of the aorta through the esophagus.
- Magnetic Resonance Angiography (MRA): Highly accurate but less used in emergencies due to longer acquisition times.
- Chest X-ray: May show a widened mediastinum, but not reliable for diagnosis.
Blood tests (e.g., D-dimer) may aid in ruling out other causes but are not diagnostic.
Management
Treatment approaches depend on the type and extent of dissection.
Initial Stabilization
Immediate interventions focus on reducing blood pressure and the force of cardiac contractions (shear stress) to limit further tearing. Typical steps include:
- IV antihypertensives (e.g., beta-blockers, nitroprusside)
- Pain control (often with opioids)
- Close monitoring in an intensive care setting
Surgical and Endovascular Intervention
- Type A Dissection: Surgical emergency. Open heart surgery is usually required to replace the affected segment of the aorta, repair or replace the aortic valve, and prevent rupture or cardiac tamponade.
- Type B Dissection: Usually managed medically unless there are complications (persistent pain, organ ischemia, rupture). Complicated cases may require endovascular stent-grafting or surgery.
Long-term Management and Follow-up
Survivors require life-long monitoring, aggressive blood pressure control, and regular imaging to detect complications or recurrence. Medications commonly include beta-blockers, ACE inhibitors, or angiotensin receptor blockers.
Complications
Aortic dissection can result in several life-threatening complications, including:
- Aortic rupture (often fatal within minutes)
- Cardiac tamponade (compression of the heart by blood in the pericardial sac)
- Aortic valve insufficiency
- Stroke
- Myocardial infarction (heart attack)
- Organ ischemia (kidneys, intestines, spinal cord)
- Limb ischemia
Prognosis
The mortality rate of untreated aortic dissection is extremely high: approximately 1–2% per hour in the first 24 hours for Type A dissections. Even with treatment, in-hospital mortality remains significant, but early intervention dramatically improves outcomes.
Prevention
- Preventive strategies focus on controlling risk factors:
- Prompt medical attention for any suspicious symptoms
- Strict blood pressure control
- Management of connective tissue disorders
- Regular screening for those at high risk
- Smoking cessation
- Avoidance of stimulant drugs
Nursing Care of Patients with Aortic Dissection
Interventions
Blood Pressure Control:
- Administer antihypertensive medications as prescribed (e.g., beta-blockers, vasodilators) to maintain systolic BP 100–120 mmHg.
- Avoid sudden drops in blood pressure to prevent organ hypoperfusion.
- Monitor for side effects of medications, such as bradycardia or hypotension.
Pain Management:
- Administer prescribed analgesics (e.g., morphine) for severe chest or back pain.
- Reassess pain frequently and adjust medications as needed.
Oxygen Therapy:
- Administer supplemental oxygen to maintain SpO2 >94% if hypoxaemia is present.
Positioning:
- Keep the patient in a semi-Fowler’s or supine position to reduce aortic wall stress unless contraindicated.
IV Access and Fluid Management:
- Establish large-bore intravenous access for medication and fluid administration.
- Avoid fluid overload; administer fluids cautiously as per the doctor’s advice.
Preparation for Diagnostic and Surgical Interventions:
- Prepare the patient for imaging studies (such as CT angiography or echocardiography).
- Ensure the patient is ready for possible surgical or endovascular repair, including fasting and preoperative checklists.
Monitoring for Complications
- Signs of aortic rupture: sudden increase in pain, hypotension, loss of consciousness
- Organ ischemia: chest pain, neurological deficits, abdominal pain, limb weakness or coldness
- Renal failure: decreased urine output, elevated creatinine
- Cardiac tamponade: jugular venous distension, muffled heart sounds, hypotension
Patient and Family Education
- Explain the nature of aortic dissection, treatment plan, and importance of adherence to therapy.
- Educate about signs and symptoms of complications that require immediate medical attention.
- Discuss lifestyle modifications, such as blood pressure control, smoking cessation, and regular follow-up visits.
- Provide psychological support and address anxiety or fear related to the illness.
Documentation
- Record all assessments, interventions, and patient responses accurately.
- Document vital signs, pain scores, medication administration, and any changes in patient condition.
- Note communication with the healthcare team and family.
- Can significantly contribute to improved outcomes and patient safety.
REFERENCES
- American Heart Association. Your Aorta: The Pulse of Life. https://www.heart.org/en/health-topics/aortic-aneurysm/your-aorta-the-pulse-of-life. Last reviewed 1/30/2024.
- Heart Foundation (N.Z.). Aortic dissection. https://www.heartfoundation.org.nz/your-heart/heart-conditions/aortic-dissection.
- Ferri FF. Aortic dissection. In: Ferri’s Clinical Advisor 2021. Elsevier; 2021. https://www.clinicalkey.com.
- Levy D, Goyal A, Grigorova Y, et al. Aortic Dissectio.. https://pubmed.ncbi.nlm.nih.gov/28722992/. 2023 Apr 23. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan.
- AskMayoExpert. Thoracic aortic aneurysm (adult). Mayo Clinic; 2020.
- Merck Manual (Consumer Version). Aortic Dissection. https://www.merckmanuals.com/home/heart-and-blood-vessel-disorders/aneurysms-and-aortic-dissection/aortic-dissection. Last revised 7/2023.
- Roselli EE, Idrees JJ, Bakaeen FG, et al. Evolution of Simplified Frozen Elephant Trunk Repair for Acute DeBakey Type I Dissection: Midterm Outcomes. https://pubmed.ncbi.nlm.nih.gov/29217087/. Ann Thorac Surg. 2018 Mar;105(3):749-755.
- Roselli EE, Loor G, He J, et al. Distal aortic interventions after repair of ascending dissection: the argument for a more aggressive approach. https://pubmed.ncbi.nlm.nih.gov/25726073/. J Thorac Cardiovasc Surg. 2015 Feb;149(2 Suppl):S117-24.e3.
- Sellke F, Coselli J, Sundt TM, et al., eds. Aortic Dissection and Acute Aortic Syndromes. 1st ed. 2021; Springer.
- Vekstein A, Elgharably H, Roselli EE. Chapter 56; Aortic Dissection. In: Glenn N. Levine, ed. Cardiology Secrets. 5th ed. 2018; Elsevier.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





