Candida albicans is a remarkably adaptable and resilient fungus, well known for its role in human health and disease. A common inhabitant of the human body, this microorganism can shift from a harmless commensal organism to a formidable pathogen, causing a wide spectrum of conditions—from mild superficial infections to life-threatening systemic illnesses.
Introduction to Candida Albicans
Candida albicans is a species of yeast, a type of fungus that exists as a normal part of the mucosal flora in the gastrointestinal tract, mouth, genitals, and skin of healthy humans. It is one of more than 150 species in the genus Candida, but is by far the most clinically significant. Under certain conditions, this normally innocuous organism can become pathogenic, leading to candidiasis.
Biology and Morphology
Candida albicans is a dimorphic fungus, meaning it can grow in two different forms: as single-celled yeast and as multicellular filamentous hyphae. This morphological flexibility is a key factor in its pathogenicity.
- Yeast Form: The round or oval yeast cells reproduce by budding, forming small colonies on mucosal surfaces.
- Hyphal Form: Under certain stimuli, Candida can elongate into hyphae or pseudohyphae, allowing it to invade tissues and evade immune responses.
This ability to switch between forms is called phenotypic switching and is central to the organism’s adaptability and virulence.
Ecology and Commensalism
In most individuals, C. albicans exists peacefully as a commensal organism. The body’s natural immune system and the competition from other microorganisms keep Candida populations in check. Its presence, in fact, can even be beneficial, as it helps maintain the balance of microbial communities in the human microbiome.
However, when the balance is disturbed—due to factors such as antibiotic use, immunosuppression, hormonal changes, or underlying health conditions—Candida can multiply rapidly and become pathogenic.
Pathogenicity and Virulence Factors
Candida albicans has evolved a suite of sophisticated tools to thrive both as a commensal and as a pathogen. Some of the primary virulence factors include:
- Adhesion Molecules: Proteins on the surface of Candida cells that facilitate attachment to host tissues.
- Enzyme Production: Candida secretes proteases, lipases, and phospholipases to break down host cells and tissues, aiding in invasion and nutrient acquisition.
- Biofilm Formation: C. albicans can form biofilms on medical devices like catheters and prosthetics. Biofilms are resistant to antifungal drugs and immune responses, making infections harder to treat.
- Phenotypic Switching: Ability to change form in response to environmental cues, enhancing survival and escape from immune detection.
Clinical Manifestations
Candidiasis is the term for diseases caused by Candida species. The clinical presentations are heterogeneous and depend on the site of infection and the immune status of the host.
Superficial Infections
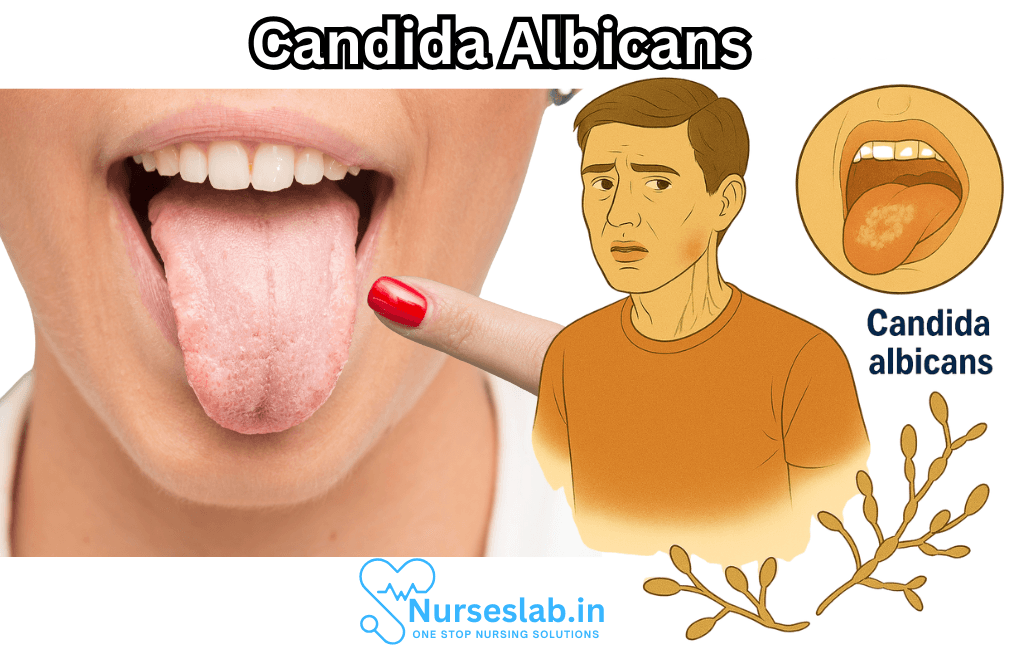
- Oral Candidiasis (Thrush): White patches on the tongue and oral mucosa, often found in infants, the elderly, and immunosuppressed individuals.
- Vulvovaginal Candidiasis: Characterized by itching, irritation, and discharge. Common in women, especially after antibiotic use or hormonal changes.
- Candida Intertrigo: Rash and inflammation in skin folds, caused by overgrowth in warm, moist areas.
- Onychomycosis: Fungal nail infections, sometimes caused by Candida.
Systemic and Invasive Infections
Systemic candidiasis can be life-threatening and usually occurs in immunocompromised individuals, such as patients undergoing chemotherapy, transplant recipients, or those with HIV/AIDS.
- Candidemia: Presence of Candida in the bloodstream, often associated with indwelling devices or prolonged hospitalization.
- Deep Tissue Candidiasis: Infections can spread to organs like the heart, brain, eyes, kidneys, and liver.
The mortality rate of invasive candidiasis remains high, despite advances in antifungal therapy.
Risk Factors
Individuals with certain risk factors are more susceptible to Candida infections:
- Antibiotic or corticosteroid use
- Compromised immune system (due to HIV, cancer, diabetes, organ transplantation, etc.)
- Poorly controlled diabetes mellitus
- Pregnancy
- Use of medical devices (catheters, dentures, prostheses)
- Poor oral hygiene
- Infancy or advanced age
Diagnosis
Diagnosis of Candida infections involves a combination of clinical assessment and laboratory tests. These may include:
- Microscopic examination of tissue samples or swabs
- Culturing the organism on selective media
- Blood cultures for suspected systemic infection
- Molecular methods such as PCR for species identification
Timely and accurate diagnosis is vital, especially in immunocompromised patients, as delayed treatment can have serious consequences.
Treatment and Management
Treatment strategies depend on the site and severity of infection.
- Topical Antifungals: Used for superficial infections like oral thrush and vaginal candidiasis (e.g., nystatin, clotrimazole, miconazole).
- Systemic Antifungals: For more severe or invasive infections (e.g., fluconazole, echinocandins, amphotericin B).
- Removal of Underlying Factors: Controlling diabetes, limiting antibiotic use, and removing infected medical devices are crucial components.
Resistance to antifungal drugs is an emerging concern, especially with widespread use of azoles like fluconazole. Multidrug-resistant Candida strains pose a challenge for clinicians and emphasize the need for ongoing research and new therapies.
Prevention
Preventing candidiasis involves minimizing risk factors and maintaining healthy immune function. Good hygiene, judicious use of antibiotics, managing chronic illnesses, and regular monitoring in high-risk patients are important measures. In hospital settings, strict protocols for catheter care and sterilization help reduce the risk of nosocomial infections.
Nursing Care of a Patient with Candida Albicans Infection
Nursing care for patients with Candida albicans infection requires a multifaceted approach, encompassing careful assessment, administration of appropriate antifungal therapies, patient education, and preventive strategies to minimize recurrence and complications.
Assessment and Early Identification
Comprehensive Patient Assessment
- History Taking: Elicit a detailed medical and surgical history, with attention to immunosuppression (e.g., diabetes, HIV/AIDS, chemotherapy), recent antibiotic or steroid use, and presence of indwelling medical devices.
- Physical Examination: Inspect common sites of infection: mouth (white patches, soreness), skin folds (erythema, maceration), genital area (itching, discharge), and, in hospitalized patients, intravenous catheter sites.
- Laboratory Investigations: Support diagnosis with KOH stain, fungal culture, or PCR, especially in ambiguous or systemic cases. Monitor blood cultures in severely immunocompromised individuals.
Planning and Implementation
Administering Antifungal Therapy
- Pharmacological Management:
- Topical antifungals (e.g., nystatin, clotrimazole) for localized skin or mucosal infections.
- Oral or intravenous antifungals (e.g., fluconazole, amphotericin B, echinocandins) for systemic or severe infections.
Monitor for Adverse Effects: Assess for signs of drug toxicity (hepatic, renal, gastrointestinal) and allergic reactions. Educate patients about possible side effects such as nausea, abdominal discomfort, or skin rashes.
Dosage Compliance: Reinforce the importance of completing the full course of prescribed antifungal therapy to prevent resistance or recurrence.
Maintaining Skin Integrity and Hygiene
- Skin Care: Keep affected skin areas clean and dry. Gently cleanse with mild soap and water and pat dry, especially in skin folds.
- Avoid Irritants: Advise against use of harsh soaps, perfumed products, or tight-fitting clothing that traps moisture.
- Barrier Creams: Apply barrier ointments or powders to prevent further skin breakdown, especially in incontinent or bedbound patients.
Oral and Genital Candidiasis Care
- Oral Hygiene: Encourage regular oral care. Instruct patients to rinse their mouth after inhaled corticosteroids and remove dentures at night, cleaning thoroughly.
- Dietary Modifications: Advise avoidance of sugary foods that promote yeast growth. Promote balanced nutrition to support immune function.
- Genital Care: Advise on wearing loose, breathable cotton underwear and maintaining genital cleanliness. Provide patient-specific instructions on topical or suppository antifungal applications.
Patient Education and Health Promotion
Recognizing Symptoms and When to Seek Help
- Signs of Infection: Educate patients to recognize signs such as persistent itching, redness, white patches, pain, or discharge, and to report new or worsening symptoms promptly.
- Risk Factors: Provide information about risk factors—uncontrolled diabetes, immunosuppression, long-term antibiotics, poor hygiene—and strategies to minimize these risks.
Lifestyle and Environmental Modifications
- Personal Hygiene: Emphasize regular bathing and proper drying of skin folds. Teach effective hand hygiene practices to reduce cross-contamination.
- Clothing Choices: Recommend loose-fitting, moisture-wicking clothing to reduce sweating and promote ventilation.
- Diet and Nutrition: Encourage a diet low in refined sugars and high in fiber, vitamins, and minerals to support immune health.
- Probiotics: Discuss the potential benefit of probiotics, such as live-culture yogurt, to restore healthy flora, particularly following antibiotic use (under medical guidance).
Prevention of Recurrence
- Antibiotic Stewardship: Advise patients and caregivers on the judicious use of antibiotics to prevent disruption of normal flora.
- Chronic Illness Management: Support optimal control of chronic illnesses like diabetes, which predispose to recurrent infections.
- Regular Follow-up: Schedule follow-up appointments to monitor for recurrence or complications, and reinforce preventive measures.
Special Considerations
Immunocompromised and Hospitalized Patients
- Heightened Vigilance: In immunocompromised individuals, candidiasis can progress rapidly to systemic infection. Monitor for fever, hypotension, organ dysfunction, and sepsis.
- Infection Control: Adhere strictly to infection control protocols, including hand hygiene, sterile technique for invasive devices, and routine surveillance cultures as indicated.
- Central Line and Device Care: Regularly assess intravenous and urinary catheters for signs of infection. Promptly remove unnecessary indwelling devices.
- Multidisciplinary Collaboration: Collaborate with infectious disease specialists, pharmacists, and dietitians for comprehensive management.
Pediatric and Geriatric Care
- Pediatrics: Infants are prone to oral thrush and diaper dermatitis. Educate parents on gentle cleaning, frequent diaper changes, and recognizing early signs.
- Geriatrics: Older adults may have decreased immunity and mobility. Assess for signs of candidiasis in dependent or bedbound seniors and implement preventative skin care regimens.
Documentation and Legal/Ethical Considerations
- Accurate Record-Keeping: Document assessment findings, nursing interventions, patient responses, education provided, and coordination with other healthcare professionals.
- Patient Privacy: Maintain confidentiality regarding the patient’s diagnosis and treatment plan in line with institutional policies and ethical standards.
REFERENCES
- British Society for Immunology. Candida albicans. https://www.immunology.org/public-information/bitesized-immunology/pathogens-disease/candida-albicans. .
- Centers for Disease Control and Prevention (U.S.). Candidiasis Basics. https://www.cdc.gov/candidiasis/about/index.html. Last updated 4/24/2024.
- Richardson JP. Candida albicans: A Major Fungal Pathogen of Humans. Pathogens. 2022 Apr 11;11(4):459. doi: 10.3390/pathogens11040459. PMID: 35456133; PMCID: PMC9025087.
- Poulain D. Candida albicans, plasticity and pathogenesis. https://pubmed.ncbi.nlm.nih.gov/23962107/. Crit Rev Microbiol. 2015; 208–217. Accessed 5/10/2022.
- Talapko J, Juzbašić M, Matijević T, et al. Candida albicans-The Virulence Factors and Clinical Manifestations of Infection. https://pmc.ncbi.nlm.nih.gov/articles/PMC7912069/. J Fungi (Basel). 2021 Jan 22;7(2):79.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





