Tuberculosis, which is caused by Mycobacterium Tuberculosis, is a chronic respiratory disease usually lasting for more than 3 months. It is commonly associated with poverty, malnutrition, overcrowding, substandard housing and inadequate healthcare.
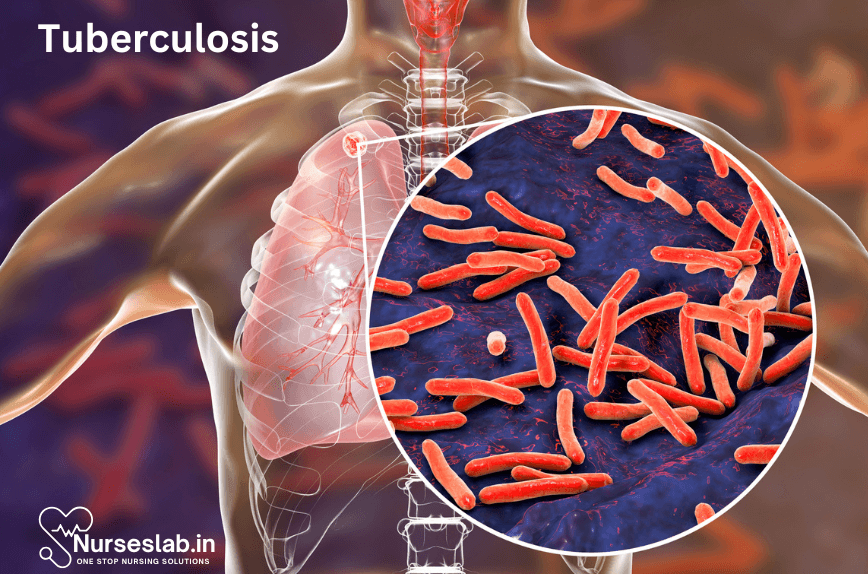
Tuberculosis is an infection which primarily affects the lung parenchyma, but it can also spread to other areas within the body, such as the meninges, kidneys, bones and lymph nodes.
Tuberculosis Pathophysiology
TB is a contagious bacterial infection caused by Mycobacterium tuberculosis. It primarily affects the lungs but can also spread to other organs. Understanding the pathophysiology of TB is crucial for developing effective treatment and prevention strategies.

Pathogen Characteristics
Mycobacterium tuberculosis is a slow-growing, rod-shaped bacterium with a unique cell wall containing mycolic acid, which makes it resistant to many common antibiotics. This bacterium is transmitted through airborne droplets when an infected person coughs, sneezes, or speaks.
Transmission and Initial Infection
When a person inhales TB bacteria, the bacilli travel down the respiratory tract and reach the alveoli of the lungs. Here, they are engulfed by alveolar macrophages. However, M. tuberculosis can survive and replicate within these cells due to its ability to inhibit phagosome-lysosome fusion. This allows the bacteria to evade the host’s immune response initially.
Immune Response
The immune system responds to TB infection through both innate and adaptive mechanisms. The initial innate response involves the recruitment of macrophages, dendritic cells, and neutrophils to the site of infection. These cells attempt to contain the infection by forming granulomas, which are aggregates of immune cells surrounding the bacteria.
The adaptive immune response is characterized by the activation of T-cells, particularly CD4+ T-helper cells. These cells release cytokines like interferon-gamma (IFN-γ), which activate infected macrophages to kill the bacteria. Despite these efforts, M. tuberculosis can persist in a dormant state within granulomas, leading to latent TB infection.
Latent TB Infection
In latent TB infection, the bacteria remain alive but inactive within the granulomas. Individuals with latent TB do not exhibit symptoms and are not contagious. However, the bacteria can reactivate if the person’s immune system becomes compromised, leading to active TB disease.
Reactivation and Active TB Disease
Reactivation of TB occurs when the immune system fails to maintain control over the latent infection. This can happen due to factors such as HIV infection, malnutrition, diabetes, or immunosuppressive therapy. During reactivation, the granulomas break down, releasing the bacteria into the alveoli and causing active TB disease.
Patients with active TB disease typically present with symptoms such as a persistent cough, weight loss, fever, night sweats, and hemoptysis (coughing up blood). The disease can also disseminate to other organs, causing extrapulmonary TB, which can affect the lymph nodes, bones, kidneys, and central nervous system.
Pathological Changes
The pathological changes in TB-affected tissues are characterized by caseating necrosis, which is a form of tissue death that results in a cheese-like appearance. This occurs due to the immune response and the release of toxic substances by the bacteria and immune cells. The necrotic tissue can form cavities in the lungs, which facilitate the spread of bacteria to other parts of the body and other individuals.
Tuberculosis Classification Based on CDC
| Class | Description |
| Class 0 | No TB exposure, not infected (no history of exposure, negative reaction to tuberculin skin test). |
| Class 1 | TB exposure, no evidence of infection (history of exposure, negative reaction to tuberculin skin test). |
| Class 2 | TB infection, no disease (positive reaction to tuberculin skin test, negative bacteriologic studies, no clinical or radiographic evidence of active TB). |
| Class 3 | TB, clinically active (M. tuberculosis cultured, clinical, bacteriologic, or radiographic evidence of active TB). |
| Class 4 | TB, not clinically active (history of TB, abnormal but stable radiographic findings, positive reaction to tuberculin skin test, negative bacteriologic studies, no clinical or radiographic evidence of active TB). |
| Class 5 | TB suspect (diagnosis pending, should not be in this classification for more than 3 months). |
Tuberculosis Causes
Pathogen: Mycobacterium Tuberculosis
The primary cause of TB is the bacterium Mycobacterium tuberculosis. This pathogen is a slow-growing, aerobic organism that thrives particularly well in areas of the body with high oxygen levels, such as the lungs. The bacterium has a waxy cell wall due to the presence of mycolic acid, which contributes to its resistance to many disinfectants and its ability to survive in harsh conditions.
Modes of Transmission
Airborne Transmission
TB is primarily transmitted through airborne particles known as droplet nuclei. When an individual with active pulmonary or laryngeal TB coughs, sneezes, speaks, or sings, they expel these droplet nuclei into the air. Another person can inhale these particles, which then travel to the lungs, potentially leading to infection.
Close Contact
Prolonged and close contact with someone who has active TB increases the risk of transmission. This is particularly common in households, workplaces, and other settings where people spend extended periods together.
Risk Factors
Several factors can increase the risk of developing TB. These factors can be broadly categorized into environmental, genetic, and health-related factors.
Environmental Factors
Overcrowding: Living in crowded conditions, such as in refugee camps, prisons, or urban slums, can facilitate the spread of TB due to the increased likelihood of close contact with infected individuals.
Poor Ventilation: Environments with inadequate ventilation allow droplet nuclei to remain airborne for longer periods, increasing the risk of inhalation by others.
Socioeconomic Status: Poverty can contribute to malnutrition, poor living conditions, and limited access to healthcare, all of which can elevate the risk of TB infection and progression.
Genetic Factors
Genetic susceptibility plays a role in determining an individual’s risk of developing TB. Certain genetic variants can affect the immune system’s ability to recognize and respond to Mycobacterium tuberculosis, making some people more vulnerable to the disease.
Health-Related Factors
HIV/AIDS: Individuals with HIV/AIDS are at a significantly higher risk of developing TB due to their weakened immune systems. TB is a leading cause of death among people living with HIV.
Diabetes: Diabetes can impair the immune system, making it more difficult for the body to fight off infections, including TB.
Malnutrition: Malnourished individuals have compromised immune systems, which can make them more susceptible to TB infection and progression.
Substance Abuse: Drug and alcohol abuse can weaken the immune system and increase the risk of TB infection.
Pre-existing Lung Conditions: Conditions such as silicosis, chronic obstructive pulmonary disease (COPD), and lung cancer can increase the risk of TB by damaging the lungs and making them more susceptible to infection.
Signs and Symptoms of Tuberculosis
Tuberculosis (TB) is a contagious and potentially life-threatening infectious disease caused by the bacterium Mycobacterium tuberculosis. It primarily affects the lungs but can also affect other parts of the body. Recognizing the signs and symptoms of TB is crucial for early diagnosis and treatment, which can help prevent the spread of the disease and improve patient outcomes.
1.Primary Symptoms of Pulmonary Tuberculosis
Persistent Cough
One of the most common symptoms of pulmonary TB is a persistent cough that lasts for three weeks or longer. This cough may produce sputum (phlegm) and can sometimes be bloody.
Chest Pain
Individuals with TB may experience chest pain, which can worsen with coughing or breathing deeply. This pain is often due to inflammation of the lungs and surrounding tissues.
Shortness of Breath
As the disease progresses, it can cause difficulty breathing and shortness of breath, particularly during physical activity.
2.General Symptoms of Tuberculosis
Fever
A low-grade fever that persists over time is a common symptom of TB. Fever is the body’s natural response to infection and inflammation.
Night Sweats
People with TB often experience night sweats, which can be severe and result in soaked bedclothes and sheets.
Weight Loss
Unintentional weight loss is a significant symptom of TB. The disease can lead to a loss of appetite and increased metabolism due to the body’s efforts to fight the infection.
Fatigue
TB can cause extreme tiredness and fatigue, even with adequate rest. This is due to the body’s prolonged effort to combat the infection.
3.Extrapulmonary Tuberculosis Symptoms
TB can also affect other parts of the body, leading to a range of symptoms depending on the organs involved.
Lymph Nodes
Swollen and tender lymph nodes, particularly in the neck or armpits, can be a sign of TB.
Spine
Tuberculosis of the spine, known as Pott’s disease, can cause back pain and, in severe cases, lead to neurological deficits.
Kidneys and Urinary Tract
TB can infect the kidneys and urinary tract, causing symptoms such as blood in the urine, frequent urination, and lower back pain.
Brain and Central Nervous System
TB meningitis, an infection of the membranes covering the brain and spinal cord, can cause severe headaches, confusion, and neurological symptoms.
Tuberculosis Prevention
Tuberculosis (TB) is a contagious bacterial infection primarily affecting the lungs but can also impact other parts of the body. It is caused by Mycobacterium tuberculosis and spreads through airborne particles from an infected person. Preventing TB is critical in reducing its global burden and ensuring public health safety. This document outlines various strategies and measures for the prevention of tuberculosis.
Vaccination
The Bacillus Calmette-Guérin (BCG) vaccine is the only available vaccine for TB. It is administered to infants in countries with a high prevalence of TB to provide protection against severe forms of the disease, such as TB meningitis and miliary TB. While the BCG vaccine is not entirely effective in preventing pulmonary TB in adults, it remains a crucial tool in the global fight against tuberculosis.
Screening and Early Detection
Regular screening and early detection are vital in preventing the spread of TB. High-risk groups, such as healthcare workers, people living with HIV, and those in close contact with TB patients, should undergo regular TB testing. Early diagnosis allows for prompt treatment, reducing the likelihood of transmission and complications.
Tuberculin Skin Test (TST)
The Tuberculin Skin Test, also known as the Mantoux test, involves injecting a small amount of tuberculin purified protein derivative (PPD) into the skin. A positive reaction, characterized by a raised bump at the injection site, indicates TB infection.
Interferon-Gamma Release Assays (IGRAs)
Interferon-Gamma Release Assays are blood tests that measure the immune response to TB bacteria. IGRAs are particularly useful for individuals who have received the BCG vaccine, as they do not produce false-positive results like the TST.
Infection Control Measures
Implementing stringent infection control measures in healthcare settings and communities is essential to prevent TB transmission.
Isolation of Infected Individuals
Individuals diagnosed with active TB should be isolated until they are no longer contagious. This can involve hospitalization or home isolation, depending on the severity of the disease and the risk of transmission.
Use of Protective Equipment
Healthcare workers and caregivers should use personal protective equipment (PPE) such as N95 respirators and surgical masks to reduce the risk of inhaling TB bacteria.
Ventilation
Improving ventilation in healthcare facilities, homes, and public spaces can help disperse airborne TB particles, reducing the risk of transmission.
Public Education and Awareness
Raising public awareness about TB symptoms, transmission, and prevention is crucial in the global fight against the disease. Educational campaigns can inform people about the importance of early detection, adherence to treatment, and the need for regular testing in high-risk groups.
Preventive Treatment
Preventive treatment, also known as latent TB infection (LTBI) treatment, involves administering antibiotics to individuals with latent TB to prevent the progression to active disease. This is particularly important for high-risk populations, such as people living with HIV, those with compromised immune systems, and close contacts of TB patients.
Isoniazid Preventive Therapy (IPT)
Isoniazid is an antibiotic commonly used in preventive therapy for latent TB. A typical regimen involves daily administration for six to nine months, significantly reducing the risk of developing active TB.
Rifapentine and Isoniazid Regimen
A combination of rifapentine and isoniazid administered weekly for three months (3HP) has been shown to be effective in preventing active TB. This shorter regimen improves adherence and reduces the risk of drug resistance.
Tuberculosis Complications
- Respiratory Failure
- Pneumothorax
- Pneumonia (one of the most fatal complications of TB since it may cause infection all over the lungs, leading to TB Pneumonia)
Assessment & Diagnostic Findings
- Sputum Culture – positive result for Mycobacterium Tuberculosis during the active TB stage (no longer contained by macrophages)
- Mantoux Test – positive reaction indicates a history of infection; it is not a direct indication of active TB (reaction in a healthy person usually indicates dormant TB, while a reaction in a clinically ill patient indicates that active TB cannot be dismissed as a diagnostic possibility
- Chest X-ray – shows evidence of scar /fibrotic tissue
- Bronchoscopy – shows evidence of inflammation; also allows sputum sample collection if needed for further testing
- Needle Biopsy of Lung Tissue – provides positive testing for TB granulomas
- Pulmonary Function Studies – indicates decreased vital capacity (caused by inflammation of the lungs that leads to difficulty in expelling air from the lungs), increased dead space (areas not involved in gaseous exchange), decreased oxygen saturation (TB affects gaseous exchange in the lungs leading to less oxygen saturation), and increased ratio of residual air vs total lung capacity (due to respiratory distress) – can also be indicative of other respiratory conditions so this isn’t used alone to diagnose TB
- TB Blood Test
Tuberculosis Medical Management
TB is primarily treated with antituberculosis agents for 6-12 months…
First Line Agents:
- Isoniazid (INH) – Side Effects include Peripheral Neuritis (nerve inflammation), Hepatitis (inflammation of the liver) and Hypersensitivity to the drug eg. rash, fever, SOB following medication intake.
- Rifampin (RIF) – Side Effects include turning body secretions (eg. urine) into orange or red coloured secretions, Hepatitis, Fever, Purpura (small bruises forming on skin), Nausea and Vomiting.
- Ethambutol (EMB) – Side Effects include Optic Neuritis (inflammation of the optic nerve) and Skin Rash; use with caution in patients with renal disease
- Pyrazinamide – Side Effects include Hyperuricaemia (increased uric acid in the blood), Hepatotoxicity (damage in the liver), Skin Rash, Arthralgias (joint pain) and GI distress.
In adults with Active TB, treatment consists of all 4 drugs (this avoids the microorganism from becoming resistant to the antibiotic) usually administered daily for 2 months, followed by 4 months of INH and RIF.
In adults with Latent TB, treatment with INH is usually administered daily for 9 months.
Nursing Care of Patient with Tuberculosis
Tuberculosis (TB) remains a significant global health challenge, affecting millions of individuals worldwide. Effective management of TB requires a comprehensive approach that encompasses early diagnosis, appropriate treatment, continuous monitoring, supportive care, infection control, and prevention strategies. Nurses play a critical role in the care of patients with TB, ensuring that they receive the necessary medical and psychosocial support to achieve successful outcomes.

1.Initial Assessment and Diagnosis
The first step in nursing care for a patient with TB is a thorough initial assessment and diagnosis. This involves:
- Medical History: Collecting detailed information about the patient’s symptoms, exposure history, and previous TB infections.
- Physical Examination: Performing a comprehensive physical examination to identify signs and symptoms of TB, such as persistent cough, weight loss, night sweats, and fever.
- Diagnostic Tests: Facilitating diagnostic tests, including sputum microscopy, culture, and chest X-rays, to confirm the presence of TB and determine the extent of the disease.
2.Treatment and Medication Management
Effective treatment of TB involves a combination of antibiotics taken over an extended period. Nurses are responsible for:
- Medication Administration: Ensuring that patients adhere to their prescribed medication regimen, which may include drugs such as isoniazid, rifampicin, ethambutol, and pyrazinamide.
- Monitoring Side Effects: Regularly assessing patients for potential side effects of TB medications, such as liver toxicity, vision changes, and gastrointestinal disturbances.
- Directly Observed Therapy (DOT): Implementing DOT programs, where healthcare providers observe patients taking their medication to ensure compliance and prevent the development of drug-resistant TB.
3.Ongoing Monitoring and Support
Continuous monitoring and support are essential for patients undergoing TB treatment. This includes:
- Monthly Check-Ups: Assessing the patient’s clinical status, adherence to treatment, and any side effects.
- Repeat Sputum Tests: Conducting sputum microscopy and culture at regular intervals to confirm bacterial clearance.
- Chest X-Rays: Periodic imaging to monitor lung healing and detect any residual disease.
4.Supportive Care
Supportive care is crucial in addressing the physical, emotional, and social needs of patients with TB. Nurses should focus on:
- Nutrition: Providing dietary counseling to ensure patients receive adequate nutrition to support their recovery and overall health.
- Mental Health: Offering psychological support and counseling to help patients cope with the stress and stigma associated with TB.
- Education: Educating patients and their families about TB, its transmission, treatment, and the importance of adherence to the medication regimen.
5.Infection Control
Preventing the spread of TB within healthcare settings and the community is a priority. Nurses play a key role in infection control by:
- Isolation Precautions: Implementing appropriate isolation precautions for patients with active TB to prevent transmission to others.
- Personal Protective Equipment (PPE): Ensuring that healthcare providers use PPE, such as masks and gloves, when caring for patients with TB.
- Environmental Controls: Maintaining proper ventilation and implementing measures to reduce the risk of airborne transmission in healthcare facilities.
6.Prevention Strategies
Preventing TB involves both individual and community-level interventions, including:
- BCG Vaccination: Administering the Bacillus Calmette-Guérin (BCG) vaccine to infants in high-risk areas.
- Screening and Prophylaxis: Identifying and treating latent TB infections in high-risk populations to prevent progression to active disease.
- Public Health Initiatives: Implementing awareness campaigns, improving living conditions, and addressing social determinants of health.
Discharge Planning
- provide patient with written instructions regarding scheduling of medications and follow-up sputum testing following therapy
- teach patient about symptoms which should be reported to healthcare if present eg. haemoptysis, chest pain, fever and dyspnoea
- emphasise importance of a high protein high carbohydrate diet and adequate fluid intake
- provide information about side effects of treatments being given on discharge
- encourage smoking cessation and alcohol cessation
REFERENCES
- American Lung Association. Multiple pages were reviewed for this article. Learn About Tuberculosis (http://www.lung.org/lung-health-and-diseases/lung-disease-lookup/tuberculosis/learn-about-tuberculosis.html).
- Centers for Disease Control and Prevention. Multiple pages were reviewed for this article. Tuberculosis (TB) (https://www.cdc.gov/tb/).
- Merck Manuals Consumer Version. Multiple pages were reviewed for this article. Quick Facts: Tuberculosis and Leprosy: Tuberculosis (https://www.merckmanuals.com/home/quick-facts-infections/tuberculosis-and-leprosy/tuberculosis-tb).
- The Truth About TB. Multiple pages were reviewed for this article. TB Treatment (https://www.thetruthabouttb.org/treatment/).
- World Health Organization. Multiple pages were reviewed for this article. Tuberculosis. https://www.who.int/health-topics/tuberculosis.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





