Pyeloplasty: Surgical Treatment for Ureteropelvic Junction Obstruction
Pyeloplasty is a reconstructive surgical procedure performed to correct ureteropelvic junction (UPJ) obstruction, a condition where the flow of urine from the renal pelvis into the ureter is blocked or impaired. This obstruction can result in hydronephrosis—swelling of the kidney due to the accumulation of urine—and can cause pain, infection, and eventual loss of kidney function if left untreated. Pyeloplasty is most commonly performed in children but can also be indicated in adults. This document provides a detailed exploration of pyeloplasty, including indications, preoperative evaluation, surgical techniques, postoperative care, risks, and outcomes.
Indications for Pyeloplasty
Pyeloplasty is primarily indicated in patients diagnosed with UPJ obstruction, a condition that may be congenital or acquired. Congenital UPJ obstruction arises due to intrinsic narrowing or the presence of abnormal fibrous tissue at the junction between the renal pelvis and ureter. Acquired causes include scarring from previous surgery, trauma, kidney stones, or external compression by blood vessels (such as an aberrant renal artery).
Patients may present with a variety of symptoms, including:
- Flank pain
- Recurrent urinary tract infections
- Hematuria (blood in urine)
- Nausea and vomiting
- Palpable abdominal mass (in infants)
- Impaired renal function or decline on imaging studies
Diagnosis is typically confirmed through imaging studies, such as ultrasound, CT scan, magnetic resonance urography, or a nuclear renal scan (MAG3 or DTPA) to assess drainage and differential kidney function.
Preoperative Evaluation
A thorough preoperative evaluation is essential to determine the appropriateness of pyeloplasty and to tailor the surgical approach to each patient. Steps include:
- Detailed history and physical examination
- Imaging studies to confirm UPJ obstruction and assess anatomy
- Renal function tests to evaluate the degree of impairment
- Assessment for associated abnormalities (e.g., crossing vessels, duplicated collecting systems)
- Evaluation for infection and optimization of urinary tract health prior to surgery
Preoperative counseling is also conducted to educate the patient and their family about the nature of UPJ obstruction, surgical options, expected outcomes, and potential risks.
Surgical Techniques
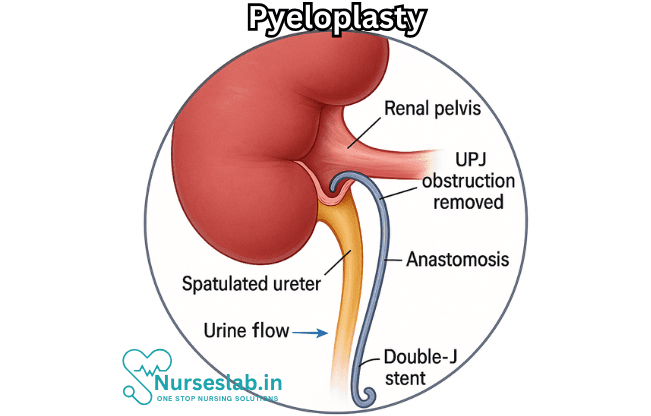
The goal of pyeloplasty is to relieve the obstruction by reconstructing the UPJ, ensuring a patent and functional connection between the renal pelvis and ureter. The two main approaches are open pyeloplasty and minimally invasive techniques, which include laparoscopic and robot-assisted pyeloplasty.
Open Pyeloplasty
Open pyeloplasty, specifically the Anderson-Hynes dismembered pyeloplasty, is considered the gold standard. The procedure involves:
- Making an incision in the flank or abdomen to access the kidney
- Identifying and dissecting the UPJ and renal pelvis
- Excising the narrowed segment of the UPJ
- Reconstructing the junction with a tension-free, watertight anastomosis between the renal pelvis and ureter
- Placement of a ureteral stent to facilitate healing and drainage
Open pyeloplasty offers excellent success rates but is associated with longer hospital stays and more postoperative discomfort compared to minimally invasive approaches.
Laparoscopic Pyeloplasty
Laparoscopic pyeloplasty employs small incisions and specialized instruments to perform the same reconstructive steps as open surgery, offering advantages such as:
- Reduced postoperative pain
- Shorter hospital stays
- Faster recovery
- Minimal scarring
Laparoscopic pyeloplasty requires advanced surgical skills, especially in intracorporeal suturing. It is suitable for both children and adults and has comparable success rates to open surgery.
Robot-Assisted Pyeloplasty
Robotic surgery has revolutionized pyeloplasty, particularly in pediatric populations. Using systems like the da Vinci Surgical System, the surgeon controls robotic arms with enhanced precision and dexterity, enabling high-definition visualization and fine suturing. Advantages include:
- Superior ergonomics for the surgeon
- Even shorter recovery times
- Low complication rates
Robotic pyeloplasty has become increasingly popular due to its reproducibility and favorable outcomes.
Alternative Techniques
Other surgical options include endopyelotomy (incision of the UPJ via endoscopic approach) and balloon dilation. These are less invasive but typically reserved for select adult patients with favorable anatomy and less severe obstruction, as their success rates are lower compared to formal pyeloplasty.
Postoperative Care
Postoperative management focuses on ensuring smooth healing, monitoring for complications, and preserving renal function.
- Patients usually remain in the hospital for several days after open surgery, but may be discharged sooner after minimally invasive procedures.
- Pain is managed with analgesics, and antibiotics are prescribed to prevent infection.
- A ureteral stent or nephrostomy tube may be left in place temporarily to ensure patency and facilitate urine drainage.
- Follow-up imaging, typically via ultrasound or diuretic renogram, is performed to confirm resolution of obstruction and improvement in kidney function.
- Patients are monitored for fever, pain, hematuria, and signs of urinary leak or infection.
Stents are usually removed a few weeks after surgery. Long-term follow-up is essential to monitor kidney health and detect any recurrence of obstruction.
Risks and Complications
Pyeloplasty is generally safe, with high success rates, but all surgical procedures carry potential risks:
- Bleeding during or after surgery
- Infection
- Urinary leakage from the anastomosis
- Injury to surrounding organs or tissues
- Failure to relieve obstruction, requiring repeat surgery
- Stricture at the site of repair
- Anesthetic risks
The risk of recurrence is low, occurring in less than 5-10% of cases following open or minimally invasive pyeloplasty.
Outcomes and Prognosis
Pyeloplasty provides definitive relief of UPJ obstruction in the majority of patients. Success rates exceed 90-95%, with restoration or preservation of renal function and resolution of symptoms. Minimally invasive and robotic techniques have matched or surpassed the outcomes of open surgery, with the added benefits of faster recovery and less morbidity.
Early intervention—especially in children diagnosed prenatally or during infancy—can prevent irreversible kidney damage and promote normal growth and development. Adults who undergo pyeloplasty for acquired UPJ obstruction also experience marked improvement in symptoms and kidney function.
Nursing Care of a Patient Undergoing Pyeloplasty
Nursing care plays a vital role in the perioperative, intraoperative, and postoperative management to ensure optimal outcomes for patients.
Preoperative Nursing Care
1. Patient Assessment
- Medical History: Gather comprehensive information regarding previous urinary tract infections, history of kidney stones, pain episodes, hematuria, and prior interventions.
- Physical Assessment: Assess for signs of infection (fever, chills), abdominal/flank pain, palpable masses, and signs suggestive of renal dysfunction (edema, hypertension).
- Laboratory and Imaging: Review results of renal function tests (serum creatinine, BUN), urinalysis, urine cultures, and imaging studies (ultrasound, CT urography, MAG3/renogram) to evaluate kidney function and extent of obstruction.
2. Patient Education
- Explain the purpose and procedure of pyeloplasty, expected outcomes, and possible postoperative experiences.
- Discuss the importance of preoperative fasting, medication adjustments, and cessation of certain drugs (e.g., anticoagulants as per physician’s order).
- Address anxiety by providing emotional support, answering questions, and introducing the surgical and nursing team.
3. Preoperative Preparations
- Ensure informed consent has been obtained.
- Administer preoperative antibiotics as ordered to prevent infection.
- Assist with bowel preparation if prescribed, particularly for open surgeries.
- Implement preoperative fasting guidelines, typically NPO after midnight.
- Initiate IV access for fluids and medications.
- Monitor and document baseline vital signs, urine output, and overall hydration status.
Intraoperative Nursing Care
- Positioning: Assist with patient positioning to prevent pressure injuries and facilitate surgical access (usually lateral or modified flank position).
- Aseptic Technique: Ensure strict aseptic measures to minimize infection risk.
- Surgical Safety Checklist: Confirm identity, procedure, site, and allergies as part of the surgical safety protocol.
- Monitoring: Continuously monitor vital signs, fluid balance, and blood loss.
- Support: Provide reassurance and maintain communication with the surgical team regarding patient status.
Postoperative Nursing Care
1. Immediate Postoperative Phase
- Airway and Breathing: Ensure airway patency and monitor respiratory status, especially in patients recovering from general anesthesia.
- Circulation: Monitor heart rate, blood pressure, oxygen saturation, and peripheral perfusion.
- Pain Management: Administer analgesics as prescribed using appropriate pain assessment tools (e.g., Numeric Rating Scale, FLACC for children). Employ non-pharmacological interventions such as positioning, relaxation, and cold packs if appropriate.
- Fluid Balance: Closely monitor IV fluids, urine output (via Foley catheter or nephrostomy tube if present), and drain outputs. Assess for signs of dehydration or fluid overload.
- Wound Care: Inspect surgical site for bleeding, swelling, infection, or excessive drainage. Maintain aseptic dressing changes as per protocol.
- Catheter and Drain Management: Ensure patency of urinary catheters, nephrostomy tubes, or surgical drains. Monitor for leakage, obstruction, or infection.
- Infection Prevention: Monitor temperature, white blood cell count, and wound characteristics. Adhere to hand hygiene and infection control protocols.
- Early Mobilization: Encourage movement and ambulation as soon as feasible to reduce risk of thromboembolism and facilitate recovery.
2. Ongoing Postoperative Care
- Renal Function Monitoring: Monitor urine output meticulously (color, clarity, amount) and note any changes indicating obstruction or bleeding. Track laboratory renal markers.
- Nutrition: Reinstitute oral intake as per recovery progress, starting with clear fluids and advancing to solids as tolerated. Emphasize a balanced, kidney-friendly diet, especially if there is pre-existing renal impairment.
- Medication Administration: Continue prescribed antibiotics, analgesics, and other supportive medications. Monitor for adverse drug reactions.
- Patient Positioning: Assist with turning and positioning to prevent pressure ulcers, particularly if mobility is limited.
- Psychosocial Support: Offer reassurance, listen to concerns, and involve family in care and education. Identify signs of postoperative anxiety or depression and provide support or referral as needed.
3. Complication Surveillance
- Hemorrhage: Watch for signs of internal or external bleeding (tachycardia, hypotension, pallor, decreasing hemoglobin).
- Infection: Monitor for fever, redness, swelling, or pus at the incision site, and for symptoms of urinary tract infection.
- Urinary Leakage/Obstruction: Observe for decreased or absent urine output, abdominal distension, or discomfort—promptly report to the surgical team.
- Thromboembolism: Assess for calf pain, swelling, erythema, or shortness of breath, and implement preventative measures such as compression stockings or anticoagulants.
- Impaired Renal Function: Be vigilant for rising creatinine, declining urine output, or electrolyte disturbances.
Discharge Planning and Patient Education
1. Home Care Instructions
- Educate on wound and drain care, indications of infection, and when to seek medical help.
- Explain the importance of adequate hydration, regular voiding, and monitoring urine color and volume.
- Discuss medication regimens, emphasizing completion of antibiotic courses and adherence to prescribed pain management plans.
- Provide dietary guidelines to promote kidney health and overall recovery.
- Advise on activity restrictions, gradual resumption of daily activities, and avoidance of strenuous exertion until cleared by the physician.
2. Follow-up Care
- Schedule appointments for follow-up imaging (e.g., ultrasound, renogram) to assess surgical success and kidney function.
- Arrange for suture or staple removal as needed.
- Establish a line of communication for questions or concerns after discharge.
Special Considerations
1. Pediatric Patients
- Family-Centered Care: Involve parents/guardians in care planning and education.
- Age-Appropriate Communication: Use language and teaching tools suitable for the child’s developmental stage.
- Play Therapy: Incorporate play and distraction techniques to reduce anxiety and promote cooperation.
2. Patients with Pre-existing Conditions
- Adjust care plans for those with chronic kidney disease, diabetes, or cardiovascular disorders.
- Coordinate closely with multidisciplinary teams (nephrology, cardiology, nutrition) as needed.
Documentation and Communication
- Maintain thorough and timely documentation of assessments, interventions, patient responses, and education provided.
- Communicate effectively with the surgical and multidisciplinary team to ensure continuity and safety of care.
REFERENCES
- Alizadeh F, Haghdani S, Seydmohammadi B. Minimally invasive open pyeloplasty in children: Long-term follow-up. https://pubmed.ncbi.nlm.nih.gov/32449670/ Turk J Urol. 2020 Sep;46(5):393-397.
- Carpenter CP, Tolley E, Tourville E, Sharadin C, Giel DW, Gleason JM. Hydronephrosis After Pyeloplasty: “Will It Go Away?”. https://pubmed.ncbi.nlm.nih.gov/30125645/ Urology. 2018 Nov;121:158-163.
- Mendrek M, Vögeli TA, Bach C. Recent advances in urologic surgical techniques for pyeloplasty. F1000Res. 2019 Mar 15;8:F1000 Faculty Rev-295. doi: 10.12688/f1000research.15866.1. PMID: 30906534; PMCID: PMC6426100.
- Isoyama T, Iwamoto H, Inoue S, et al. Hydronephrosis after retroperitoneal laparoscopic dismembered Anderson-Hynes pyeloplasty in adult patients with ureteropelvic junction obstruction: A longitudinal analysis. https://pubmed.ncbi.nlm.nih.gov/24982795/ Cent European J Urol. 2014;67(1):101-5.
- Seo IY, Oh TH, Lee JW. Long-term follow-up results of laparoscopic pyeloplasty. https://pubmed.ncbi.nlm.nih.gov/25324948/. Korean J Urol. 2014 Oct;55(10):656-9.
- Värelä S, Omling E, Börjesson A, Salö M. Resolution of hydronephrosis after pyeloplasty in children. https://pubmed.ncbi.nlm.nih.gov/33218882/ J Pediatr Urol. 2021 Feb;17(1):102.e1-102.e7.
- Wickramasekara N, Ignatius J, Lamahewage A. Sonographic follow-up after pyeloplasty: a large, retrospective cohort analysis. https://pubmed.ncbi.nlm.nih.gov/36808250/ Pediatr Surg Int. 2023 Feb 18;39(1):132.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





