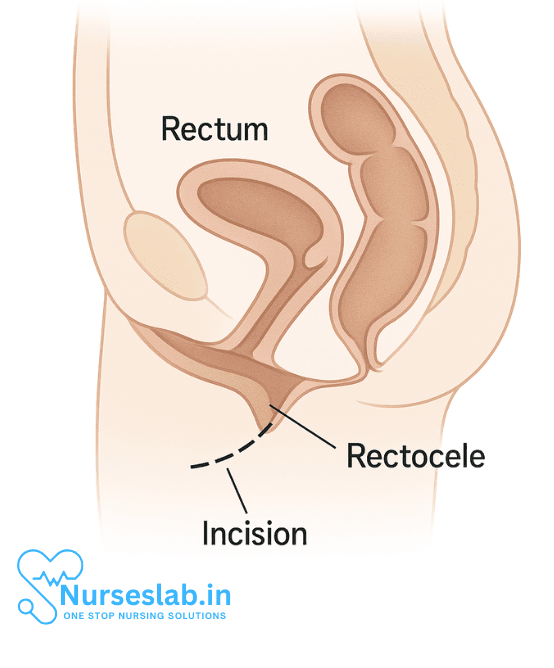
A rectocele is a bulging of the front wall of the rectum into the back wall of the vagina. This condition is a type of pelvic organ prolapse that occurs when the supportive tissue between the rectum and the vagina becomes weakened. Rectocele repair is a surgical procedure designed to correct this bulge, relieve associated symptoms, and restore normal anatomy and function. This comprehensive guide explores the causes, symptoms, diagnosis, surgical techniques, recovery, and potential risks of rectocele repair.
Understanding Rectocele
A rectocele develops when the rectovaginal fascia (the layer of connective tissue between the rectum and vagina) becomes thinned or torn, allowing the rectum to protrude into the vaginal canal. This weakening commonly arises due to factors that put pressure on the pelvic floor or cause tissue damage.
Causes and Risk Factors
Common causes and risk factors for rectocele include:
- Childbirth, especially vaginal deliveries and multiple pregnancies
- Chronic constipation and frequent straining during bowel movements
- Heavy lifting or repetitive strenuous activity
- Aging and menopause (due to declining estrogen levels and tissue elasticity)
- Previous pelvic surgery
- Obesity
- Connective tissue disorders (such as Ehlers-Danlos syndrome)
Symptoms
Rectocele may present with a variety of symptoms, varying in severity:
- A noticeable bulge or pressure in the vaginal area
- Difficulty with bowel movements, including the need to press on the vagina to help stool pass (splinting)
- Sensation of incomplete evacuation of stool
- Pelvic discomfort or pain
- Pain or discomfort during sexual intercourse
- Lower back pain (in some cases)
Some individuals may not experience symptoms, and the rectocele may be discovered during a routine pelvic examination.
Diagnosis
Diagnosis of rectocele typically involves:
- Medical history review
- Physical pelvic examination, often with the patient bearing down as if having a bowel movement
- Imaging tests, such as dynamic pelvic MRI or defecography, in selected cases to assess the extent of the prolapse and other pelvic floor disorders
Non-Surgical Management
Before considering surgery, conservative management may be recommended, particularly for mild cases or individuals who are not good surgical candidates.
Lifestyle and Medical Interventions
- Dietary changes: Increasing fiber and fluid intake to prevent constipation.
- Pelvic floor muscle training: Kegel exercises to strengthen the pelvic muscles supporting the rectum and vagina.
- Use of vaginal pessaries: A pessary is a device inserted into the vagina to provide additional support to the pelvic organs.
- Avoiding heavy lifting and straining: To reduce pressure on the pelvic floor.
If these approaches do not sufficiently relieve symptoms, or if the rectocele significantly impairs quality of life, surgical repair may be recommended.
Surgical Rectocele Repair
Rectocele repair aims to restore normal anatomy, relieve symptoms, and support the pelvic floor. Surgery can be performed via different approaches, and the optimal technique depends on the severity of the rectocele, patient preferences, overall health, and surgeon expertise.
Types of Surgery
- Posterior Colporrhaphy: This is the most common technique. The surgeon makes an incision in the vaginal wall, identifies the weakened or torn connective tissue, and repairs it by suturing and reinforcing the tissue. Excess vaginal wall tissue may be removed, and the vaginal wall is closed.
- Site-Specific Repair: In cases where the defect is localized, only the specific area of weakness is repaired, preserving more of the normal tissue.
- Use of Grafts or Mesh: Surgical mesh or biological grafts may be used to reinforce the repair, especially in cases of recurrent or severe rectocele. Due to concerns about complications, the use of synthetic mesh in vaginal prolapse repair has declined and is subject to regulatory guidelines in many countries.
- Laparoscopic or Robotic Repair: These minimally invasive techniques involve accessing the rectocele through small abdominal incisions. While less common for isolated rectocele, they may be chosen in complex or recurrent cases or when other pelvic repairs are needed.
- Transanal Repair: In rare cases, the repair may be performed through the anus, particularly when rectal symptoms predominate.
The Procedure
Surgery is usually performed under regional or general anesthesia. The steps typically include:
- Incision in the posterior vaginal wall
- Separation of the vaginal tissue from the rectum
- Identification and repair of the weakened connective tissue with sutures, and possible reinforcement with graft material
- Trimming of excess vaginal tissue if needed
- Closure of the vaginal wall with absorbable stitches
The operation usually takes about 1 to 2 hours and may be done on an outpatient basis or require a short hospital stay.
Risks and Complications
As with any surgical procedure, rectocele repair carries potential risks:
- Bleeding
- Infection
- Pain or discomfort during recovery
- Injury to surrounding organs (rectum, bladder, uterus)
- Urinary or fecal incontinence
- Constipation or difficulty with bowel movements
- Recurrence of rectocele or prolapse of other pelvic organs
- Pain during sexual intercourse (dyspareunia)
- Complications related to mesh (if used), such as erosion or infection
It is important to discuss all risks with your surgeon prior to surgery.
Recovery and Postoperative Care
Immediately After Surgery
- Most patients experience mild to moderate pain, which is managed with medication.
- Vaginal spotting or discharge may occur for several days.
- Bladder catheterization may be necessary for a short period, especially if there is swelling.
- Most patients can go home the same day or after a short hospital stay.
At Home
- Avoid heavy lifting, strenuous activity, and sexual intercourse for 6 to 8 weeks, or as advised by the surgeon.
- Follow a high-fiber diet, maintain adequate hydration, and use stool softeners if needed to prevent constipation and straining.
- Attend all scheduled follow-up visits to monitor healing and address any concerns.
- Gradually resume normal activities as tolerated.
Most people return to their usual activities within 4 to 6 weeks, but complete healing may take several months. Adherence to postoperative instructions is critical to minimize complications and optimize surgical outcomes.
Outcomes and Prognosis
Rectocele repair generally results in substantial improvement of prolapse symptoms and quality of life. Success rates vary, but most individuals report relief from vaginal bulging, easier bowel movements, and improved pelvic comfort. However, as with any pelvic floor surgery, recurrence can occur, particularly if underlying risk factors persist.
Factors Affecting Success
- Severity and size of the rectocele
- Type of repair technique used
- Patient age, tissue quality, and general health
- Adherence to postoperative care and lifestyle modifications
Long-term Considerations
Some individuals may require further interventions if symptoms return or if other types of pelvic organ prolapse develop. Ongoing pelvic floor exercises and management of factors like constipation remain important for prevention.
Nursing Care for Patients Undergoing Rectocele Repair
The role of nursing care is pivotal throughout the perioperative phase, ensuring optimal recovery, comfort, and patient education.
Preoperative Nursing Care
Assessment
- Comprehensive Patient History: Evaluate the patient’s medical, surgical, and obstetric history, including symptoms such as pelvic pressure, bowel issues, or urinary changes.
- Physical Examination: Assess for associated pelvic organ prolapses and overall pelvic floor function.
- Psychosocial Assessment: Identify anxiety, body image concerns, and expectations regarding the procedure.
- Laboratory and Diagnostic Tests: Ensure completion of necessary investigations, such as blood tests, urinalysis, and imaging studies if indicated.
Patient Education
- Procedure Explanation: Clearly explain the surgical process, its purpose, expected outcomes, and potential risks.
- Preoperative Preparations: Advise on fasting, bowel preparation, and cessation of certain medications as instructed by the healthcare provider.
- Postoperative Expectations: Discuss anticipated discomfort, mobility restrictions, and the importance of pelvic rest.
- Consent: Ensure the patient understands the procedure and signs the informed consent form.
Physical Preparation
- Bowel Preparation: Administer enemas or laxatives as ordered to reduce fecal load and minimize risk during surgery.
- Skin and Hygiene: Encourage showering and perineal care prior to the procedure to reduce infection risk.
- Venous Thromboembolism Prophylaxis: Apply compression stockings and encourage leg exercises if appropriate.
- Medication Review: Confirm medication reconciliation and administration of preoperative antibiotics if ordered.
Immediate Postoperative Nursing Care
Monitoring and Assessment
- Vital Signs: Monitor temperature, heart rate, blood pressure, and respiratory rate frequently during the immediate recovery period.
- Pain Management: Assess pain level regularly using standardized scales and administer analgesics as prescribed.
- Surgical Site Assessment: Inspect the perineal incision for signs of bleeding, hematoma, swelling, or infection.
- Urinary Function: Monitor voiding patterns, assess for urinary retention, and manage indwelling catheters according to protocol.
- Bowel Function: Observe for early signs of constipation, ileus, or difficulty with defecation.
Pain and Comfort Measures
- Positioning: Assist the patient to maintain a comfortable position, often semi-Fowler’s, to reduce pressure on the surgical area.
- Cold Application: Apply ice packs to the perineal area as ordered to minimize swelling and discomfort.
- Oral Medications: Administer prescribed analgesics and anti-inflammatory agents.
- Emotional Support: Provide reassurance and emotional support, addressing concerns about pain, mobility, and body image.
Wound Care
- Perineal Hygiene: Teach and assist with gentle cleaning of the perineal area, especially after voiding or defecation.
- Dressing Changes: Perform dressing changes using sterile technique as ordered, monitoring for signs of infection.
- Observation: Report any abnormal discharge, severe pain, or separation of wound edges to the surgical team promptly.
Prevention of Complications
- Infection Prevention: Administer antibiotics as prescribed, encourage hand hygiene, and educate patient about symptoms of infection.
- Thromboembolism Prevention: Reiterate the importance of leg exercises and early ambulation as tolerated.
- Constipation Prevention: Encourage adequate fluid intake, balanced nutrition, and use of stool softeners as prescribed.
- Bladder Dysfunction: Monitor catheter patency and urine output; provide education on avoiding urinary retention.
- Hemorrhage Surveillance: Frequently assess for excessive bleeding or hematoma formation, particularly in the initial postoperative hours.
Ongoing Postoperative Nursing Care
Mobility and Activity
- Early Ambulation: Encourage gradual movement with assistance to prevent venous stasis and promote healing.
- Activity Restrictions: Advise the patient to avoid heavy lifting, strenuous exercise, and sexual activity until cleared by the surgeon (often for 6 weeks).
- Pelvic Floor Exercises: Initiate gentle pelvic floor muscle training under guidance, as per physician approval.
Nutrition and Hydration
- Balanced Diet: Encourage high-fiber foods, adequate protein, and vitamins to promote tissue healing and prevent constipation.
- Fluid Intake: Remind the patient to drink sufficient water to maintain hydration and ease bowel movements.
Patient Education for Self-Care
- Hygiene Instruction: Teach proper perineal care to minimize infection risk, including wiping techniques and frequency of cleaning.
- Medication Compliance: Review prescribed medications, such as pain relievers and stool softeners, and stress the importance of adherence.
- Observation for Complications: Empower the patient to recognize signs of complications, such as fever, severe pain, abnormal discharge, or difficulty voiding.
- Activity Guidance: Explain when normal activities may be resumed and the importance of gradual return to exercise.
- Follow-Up Appointments: Stress the necessity of attending scheduled follow-ups for wound assessment and recovery progress.
Psychosocial Support
- Emotional Wellbeing: Provide a safe space for the patient to express concerns regarding body image, sexual health, and recovery expectations.
- Support Groups: Recommend support groups or resources for patients recovering from pelvic organ prolapse surgeries.
Discharge Planning
Home Care Instructions
- Wound Management: Demonstrate dressing changes and hygiene techniques to be continued at home.
- Symptom Monitoring: Advise on monitoring for fevers, redness, swelling, and report any concerning changes to the healthcare provider.
- Diet and Bowel Care: Reinforce the importance of fluids, fiber, and avoidance of straining during bowel movements.
- Activity Resumption: Outline a gradual plan for increasing physical activity, emphasizing rest and avoidance of heavy tasks.
Follow-Up Care
- Outpatient Visits: Ensure the patient has appointments scheduled for ongoing wound checks and progress assessment.
- Continuity of Care: Coordinate with the healthcare team for ongoing support, referrals to physical therapy if needed, and access to additional resources.
Special Considerations
Care for Older Adults
- Assessment of Comorbidities: Pay close attention to other chronic diseases or cognitive issues that may impact recovery.
- Medication Management: Watch for polypharmacy interactions and ensure understanding of medication regimens.
- Fall Prevention: Implement safety measures and educate on home modifications if needed.
Care for Patients with Limited Support Systems
- Social Services Referral: Provide access to home health nurses or rehabilitation services if family support is limited.
- Community Resources: Connect patient to local resources for transportation, meal delivery, or additional caregiving if required.
REFERENCES
- American Society of Colon and Rectal Surgeons (ASCRS). Rectocele Expanded Information. https://fascrs.org/patients/diseases-and-conditions/a-z/rectocele-expanded-information.
- Aubert M, Mege D, Le Huu Nho R, Meurette G, Sielezneff I. Surgical management of the rectocele – An update. https://pubmed.ncbi.nlm.nih.gov/33495108/. J Visc Surg. 2021 Apr;158(2):145-157.
- Noé GK. Genital Prolapse Surgery: What Options Do We Have in the Age of Mesh Issues?. https://pubmed.ncbi.nlm.nih.gov/33450901/ J Clin Med. 2021 Jan 13;10(2):267
- Fathy M, et al. (2021). Literature review of the outcome of and methods used to improve transperineal repair of rectocele.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8462077/ - Nüssler E, Granåsen G, Nüssler EK, Bixo M, Löfgren M. Repair of recurrent rectocele with posterior colporrhaphy or non-absorbable polypropylene mesh-patient-reported outcomes at 1-year follow-up. https://pubmed.ncbi.nlm.nih.gov/30627830. Int Urogynecol J. 2019 Oct;30(10):1679-1687.
- Murphy AM, et al. Surgical management of vaginal prolapse: Current surgical concepts. The Canadian Journal of Urology: International Supplement. 2021; https://www.canjurol.com/abstract.php?ArticleID=&version=1.0&PMID=34453425.
- Gershenson DM, et al. Pelvic organ prolapse, abdominal hernias and inguinal hernias: Diagnosis and management. In: Comprehensive Gynecology. 8th ed. Elsevier; 2022. https://www.clinicalkey.com.
- Nussler E, et al. (2022). Long-term outcome after routine surgery for pelvic organ prolapse — A national register-based cohort study.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9270303/
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





