An In-Depth Guide to Principles, Procedure, and Clinical Applications
Introduction
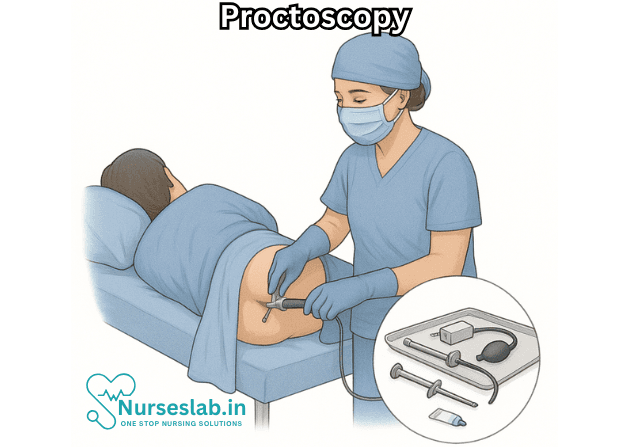
Proctoscopy, often referred to as rigid sigmoidoscopy, is a diagnostic and therapeutic procedure that allows direct visual examination of the anal canal, rectum, and the lower segment of the sigmoid colon. It is performed using a rigid, straight, tubular instrument called a proctoscope or sigmoidoscope. This procedure has long played a pivotal role in the investigation and management of various lower gastrointestinal tract disorders. Although flexible endoscopy has become more prevalent in modern clinical practice, rigid sigmoidoscopy remains an essential tool in certain settings due to its simplicity, accessibility, and diagnostic utility.
Historical Perspective
The origins of proctoscopy can be traced back to the late 19th and early 20th centuries, when physicians sought effective means to visualize and diagnose diseases of the distal colon. Early iterations of the proctoscope were basic, consisting of a metal or glass tube with a light source attached. Over time, advances in optics, lighting, and instrument design have made the procedure safer, more comfortable, and more effective.
Anatomical Areas Visualized
Proctoscopy is specifically designed to inspect the following regions:
- Anal canal
- Rectum (typically up to 15 cm from the anal verge)
- Distal sigmoid colon (in some cases, depending on the length of the instrument and the patient’s anatomy)
During the procedure, the examiner can assess the mucosa for color, vascular pattern, lesions, bleeding, polyps, masses, ulcerations, and other abnormalities.
Indications
Proctoscopy (rigid sigmoidoscopy) is indicated in a variety of clinical scenarios:
- Evaluation of rectal bleeding (hematochezia)
- Assessment of anorectal pain, discharge, or pruritus
- Investigation of suspected masses, polyps, or neoplasms
- Diagnosis of anorectal diseases (hemorrhoids, fissures, fistulas, proctitis)
- Follow-up of previously detected lesions or malignancies
- Screening in high-risk populations for colorectal cancer
- Therapeutic interventions (biopsy, polypectomy, control of minor bleeding)
- Evaluation of foreign bodies in the anorectal region
Contraindications
While generally safe, proctoscopy may not be appropriate in certain situations:
- Acute severe anal or rectal pain
- Known or suspected perforation of the colon
- Acute peritonitis
- Severe anal stenosis
- Acute severe inflammation or infection (e.g., perianal abscess)
- Severe coagulopathy or bleeding disorders (relative contraindication; must be corrected before the procedure)
Preparation for the Procedure
Proper preparation is crucial for an effective and safe proctoscopy. The following steps are typically undertaken:
- Patient Information and Consent: The purpose, risks, and benefits of the procedure should be explained, and informed consent obtained.
- Bowel Preparation: A simple rectal enema is often sufficient to clear the distal bowel of fecal material. Extensive bowel preparation is not usually required.
- Positioning: The patient is typically positioned in the left lateral (Sims’) position, with hips and knees flexed. This allows for optimal access and comfort.
- Local Anesthetic: Not routinely necessary, but a local anesthetic gel may be applied to reduce discomfort, particularly in sensitive individuals.
- Privacy and Dignity: The patient’s privacy should be maintained throughout the procedure, with appropriate draping and explanation.
The Proctoscope: Instrumentation
A proctoscope is a rigid, cylindrical tube, generally 10–20 cm in length and 2–3 cm in diameter. It consists of:
- Outer sheath: The main tube inserted into the rectum
- Obturator: A blunt-tipped inner instrument that facilitates smooth introduction
- Light source: Either built-in or external, to illuminate the lumen
Some models include channels for biopsy forceps or suction.
Procedure: Step-by-Step
The typical course of a proctoscopy includes the following steps:
- Preparation: After appropriate positioning and draping, the operator dons gloves and lubricates the proctoscope.
- Digital Rectal Examination: A preliminary digital examination is performed to exclude obstruction, severe pain, or masses, and to assess sphincter tone.
- Insertion: The lubricated proctoscope, with obturator in place, is gently introduced through the anus along the longitudinal axis of the anal canal. The obturator is then removed, allowing for direct visualization.
- Inspection: The examiner inspects the mucosa as the scope is slowly advanced. Any lesions, polyps, bleeding points, or abnormalities are noted. Biopsies or therapeutic interventions may be performed as indicated.
- Withdrawal: The instrument is slowly withdrawn, enabling further inspection of the mucosa and detection of lesions that may have been missed on insertion.
- Completion: The findings are documented, and the patient is provided with appropriate aftercare instructions.
Complications and Safety
Proctoscopy is considered a safe procedure when performed by trained personnel, with complications being rare and generally minor. Potential complications include:
- Mild discomfort or pain
- Rectal bleeding, particularly if biopsy or polypectomy is performed
- Mucosal injury or, very rarely, perforation of the bowel wall
- Vasovagal syncope (fainting)
- Infection (extremely rare)
The risk of serious adverse events is extremely low, especially compared to procedures involving deeper insertion into the colon.
Advantages and Limitations
Advantages:
- Simple and rapid to perform; no sedation typically required
- Readily available in most outpatient, emergency, and surgical settings
- Excellent for direct visualization of distal rectal and anal pathology
- Allows for biopsy and minor procedures in real time
Limitations:
- Limited examination depth (only up to about 15–20 cm from the anal verge)
- May not detect more proximal colonic lesions or pathology
- Can be uncomfortable for some patients
Comparison with Flexible Sigmoidoscopy and Colonoscopy
Flexible sigmoidoscopy and colonoscopy allow for visual assessment of a much larger portion of the colon, including the entire sigmoid and descending colon (flexible sigmoidoscopy) or the entire colon (colonoscopy). They also have a broader role in screening for colorectal cancer and evaluating generalized colonic symptoms. However, rigid sigmoidoscopy remains valuable for targeted assessment of distal lesions, particularly in emergency or outpatient settings where rapid diagnosis is needed.
Clinical Applications
Proctoscopy is used for both diagnostic and therapeutic purposes. Common clinical applications include:
- Diagnosis of hemorrhoids, anal fissures, and rectal tumors
- Detection of proctitis (inflammation of the rectum)
- Assessment and removal of foreign bodies
- Biopsy of suspicious lesions or masses
- Treatment of minor rectal bleeding through cautery or injection
- Monitoring previously diagnosed anorectal diseases
Aftercare and Patient Education
After a proctoscopy, most patients can resume normal activities immediately. Minor rectal bleeding or discomfort may occur, especially if a biopsy was taken, but these symptoms usually resolve quickly. Patients should be educated to report any persistent pain, heavy bleeding, fever, or signs of infection, though such complications are rare.
Nursing Care of Patients Undergoing Proctoscopy (Rigid Sigmoidoscopy)
This examination is vital for diagnosing a range of anorectal disorders such as hemorrhoids, polyps, tumors, rectal bleeding, or inflammation. While the procedure is typically brief and considered safe, it requires diligent nursing care before, during, and after to ensure patient comfort, safety, and accurate results.
Pre-Procedural Nursing Care
Patient Assessment
- Obtain a comprehensive history, including presenting symptoms, allergies, recent bowel habits, current medications, and comorbid conditions (e.g., bleeding disorders, cardiac illness).
- Assess for contraindications such as acute severe anal pain, suspected bowel perforation, or active rectal bleeding.
- Measure baseline vital signs: blood pressure, pulse, respiratory rate, and temperature.
Patient Education and Psychological Preparation
- Explain the nature, purpose, and steps of the proctoscopy procedure in clear, simple language.
- Address patient concerns, fears, or misconceptions. Reassure the patient about pain management, privacy, and the brief duration of the procedure.
- Discuss the possibility of minor discomfort or the urge to defecate during the examination.
Physical Preparation
- Diet: Generally, a light meal is permitted before the procedure. However, institutional protocols may require fasting for a few hours.
- Bowel Preparation: Ensure the lower bowel is free of fecal matter for optimal visualization. This may include:
- Administering a rectal enema (e.g., saline or glycerin suppository) approximately 1–2 hours before the procedure.
- Instructing the patient to empty their bladder before the examination to promote comfort.
- Arrange for appropriate hospital gowning to ensure comfort and privacy.
- Obtain informed consent as per institutional policy.
Preparation of the Environment and Equipment
- Ensure the examination room is clean, well-lit, and private.
- Gather all necessary equipment:
- Rigid proctoscope or sigmoidoscope with appropriate sized obturators
- Light source and connecting cables
- Lubricant (e.g., water-soluble jelly)
- Gloves (sterile/non-sterile as per protocol)
- Rectal swabs, biopsy forceps if required
- Disposable tissues, incontinence pads
- Kidney tray for soiled instruments
- Local anesthetic gel if needed
Nursing Care During the Procedure
Patient Positioning
- Assist the patient to lie in the left lateral (Sim’s) position with knees flexed towards the chest. This position provides optimal access and comfort.
- Ensure that the patient is adequately draped to maintain privacy and dignity.
Assisting the Physician
- Hand over the required instruments to the physician in a sterile manner.
- Provide adequate lighting and adjust as necessary for optimal visualization.
- Apply lubricating jelly to the tip of the proctoscope before insertion.
Monitoring and Support
- Observe the patient’s facial expressions and body language for signs of distress, discomfort, or pain. Notify the physician if the patient experiences excessive pain.
- Offer reassurance throughout the procedure, keeping the patient informed about each step.
- Monitor vital signs, especially in patients with comorbidities.
- Be alert for symptoms of vasovagal response (pallor, sweating, bradycardia, hypotension) and manage accordingly.
Specimen Handling (if indicated)
- If tissue biopsies or rectal swabs are collected, ensure proper labeling and handling as per institutional protocols.
- Document the nature and site of specimens accurately.
Post-Procedural Nursing Care
Immediate Care
- Assist the patient in removing soiled garments and in cleaning the anal area with disposable tissues or wipes.
- Help the patient return to a comfortable position, either sitting or supine, as preferred.
- Monitor for any immediate complications such as rectal bleeding, abdominal pain, faintness, or signs of perforation (rare).
- Reassess vital signs, particularly in patients with underlying health conditions or those who experienced symptoms during the procedure.
Patient Observation
- Observe for delayed complications such as persistent rectal bleeding, severe pain, fever, or signs of infection.
- Encourage the patient to report any concerning symptoms promptly.
Documentation
- Record the date, time, and type of procedure performed.
- Note the patient’s response, level of tolerance, and any adverse reactions.
- Document all specimens collected, including site, type, and destination.
- Include any patient education or instructions given post-procedure.
Patient Education and Discharge Instructions
- Inform the patient about the expected outcomes and minor side effects (e.g., mild anal discomfort, minor bleeding with the first stool).
- Instruct the patient to watch for and immediately report symptoms such as heavy rectal bleeding, severe abdominal pain, fever, or persistent dizziness.
- Reassure that normal activities can usually be resumed immediately unless sedation was used or complications occurred.
- Provide written instructions and contact information for urgent follow-up if needed.
Special Considerations
Care for Pediatric and Elderly Patients
- Pediatric patients may require additional psychological support and simplified explanations. The presence of a parent or guardian may be beneficial.
- Elderly patients may be more sensitive to discomfort and may have mobility issues; gentle handling and extra assistance are essential.
Infection Control
- Use appropriate personal protective equipment (PPE) to prevent cross-infection.
- Ensure all reusable instruments are cleaned and sterilized after the procedure.
- Discard single-use materials as per biomedical waste protocols.
Potential Complications and Nursing Management
- Rectal bleeding: Usually minor and self-limiting. Monitor and document. If persistent or heavy, inform the physician immediately.
- Perforation: Rare but serious. Watch for sudden severe abdominal pain, distention, or shock. Initiate emergency protocols if suspected.
- Infection: Maintain aseptic technique to minimize risk. Educate the patient about signs of infection post-procedure.
- Vasovagal response: Recognize symptoms and assist the patient to a safe position. Monitor vital signs and provide fluids as required.
Role of the Nurse in Holistic Care
- Provide empathetic support and reassurance to reduce patient anxiety throughout the process.
- Ensure privacy and dignity at all times.
- Educate the patient and family members about the importance and safety of the procedure.
- Participate in interprofessional collaboration with physicians, technicians, and support staff for optimal patient outcomes.
REFERENCES
- National Cancer Institute (U.S.). Endoscopies. https://training.seer.cancer.gov/diagnostic/endoscopies.html.
- Tanaka A, Sadahiro S, Suzuki T, Okada K, Saito G. Comparisons of Rigid Proctoscopy, Flexible Colonoscopy, and Digital Rectal Examination for Determining the Localization of Rectal Cancers. https://pubmed.ncbi.nlm.nih.gov/29337775/. Dis Colon Rectum. 2018;61(2):202-206.
- Steven, M., McGrogan, P. (2013). E3 Proctoscopy and Rigid Sigmoidoscopy. In: Carachi, R., Agarwala, S., Bradnock, T.J., Lim Tan, H., Cascio, S. (eds) Basic Techniques in Pediatric Surgery. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-20641-2_74
- Zelhart MD, Kann BR (2022). Endoscopy. In: Steele SR, Hull TL, Hyman N, Maykel JA, Read TE, Whitlow CB, eds. The ASCRS Textbook of Colon and Rectal Surgery. 51–77. Springer, Cham.
- Mayo Clinic Staff. (2018). Flexiblesigmoidoscopy.
https://www.mayoclinic.org/tests-procedures/flexible-sigmoidoscopy/about/pac-20394189
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





