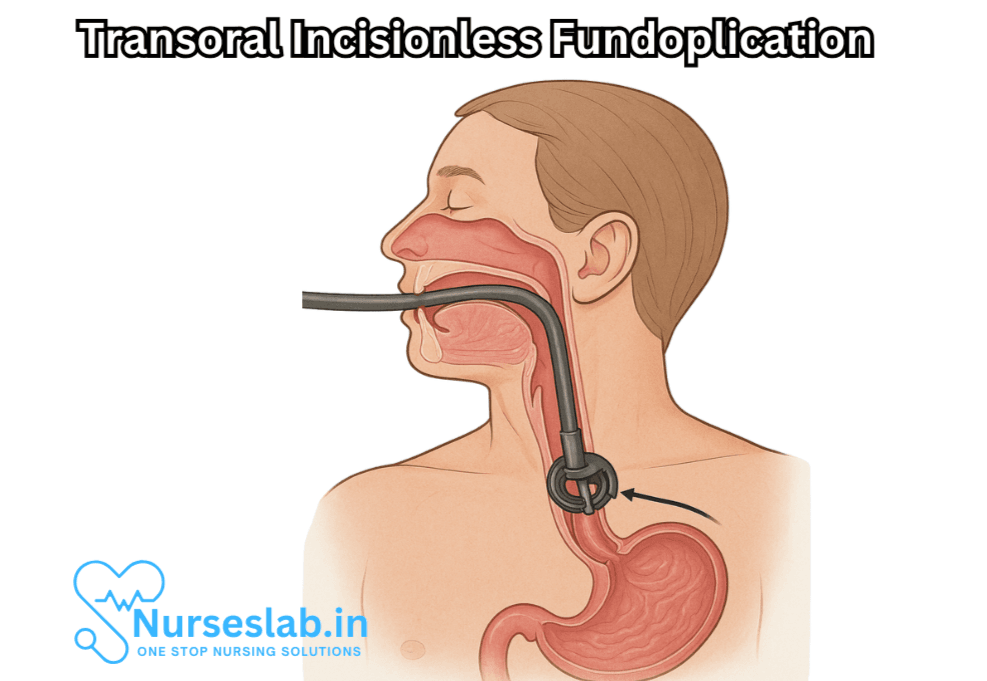
TIF Procedure (Transoral Incisionless Fundoplication) is a minimally invasive endoscopic procedure used to treat gastroesophageal reflux disease (GERD). It reconstructs the valve between the esophagus and stomach to prevent acid reflux—without surgical incisions.
Introduction
Gastroesophageal reflux disease (GERD) is a prevalent and chronic digestive disorder characterized by the abnormal reflux of stomach contents into the esophagus, resulting in symptoms such as heartburn, regurgitation, chest pain, and difficulty swallowing. While lifestyle modifications and medications like proton pump inhibitors (PPIs) form the initial line of treatment, many patients continue to experience persistent or severe symptoms. For those who seek an alternative to lifelong medication or wish to avoid conventional surgery, the Transoral Incisionless Fundoplication (TIF) procedure offers a minimally invasive, effective, and durable solution.
Understanding GERD and Its Challenges
GERD develops when the lower esophageal sphincter (LES), a ring of muscle at the junction of the esophagus and stomach, becomes weakened or relaxes inappropriately. This allows gastric acids and other contents to flow back into the esophagus, irritating the lining and causing discomfort. Long-term, uncontrolled GERD can lead to complications such as esophagitis, strictures, Barrett’s esophagus, and even esophageal cancer.
Managing GERD often begins with lifestyle interventions, including dietary changes, weight loss, and avoiding triggers like caffeine, alcohol, and spicy foods. Medications, especially PPIs, reduce the production of stomach acid and offer symptomatic relief. However, ongoing medication may not address the underlying anatomical defect, and some patients experience breakthrough symptoms or adverse effects from long-term use.
The Evolution of Anti-Reflux Surgery
For patients with persistent GERD symptoms, surgical intervention has traditionally involved fundoplication, in which the upper part of the stomach (the fundus) is wrapped around the LES to reinforce it and prevent reflux. The most common technique, laparoscopic Nissen fundoplication, requires multiple small incisions in the abdomen. While highly effective, this procedure carries surgical risks, potential for complications, and may involve a lengthy recovery period.
Recognizing the need for less invasive options, medical innovators developed the Transoral Incisionless Fundoplication (TIF) procedure, which replicates the principles of traditional fundoplication without external incisions.
What is the TIF Procedure?
Transoral Incisionless Fundoplication (TIF) is an endoscopic surgical technique designed to treat GERD by restoring the natural valve between the esophagus and stomach. TIF is performed entirely through the mouth, eliminating the need for external incisions. The procedure utilizes the EsophyX device, a specialized surgical tool that enables the surgeon to create a partial or full-thickness wrap at the gastroesophageal junction, thereby augmenting the LES.
How the TIF Procedure Works
- Anesthesia: The patient is placed under general anesthesia for optimal comfort and safety.
- Endoscopic Access: The surgeon inserts the EsophyX device and an endoscope through the mouth and into the esophagus. The endoscope provides real-time visualization of the surgical area.
- Creating the Valve: The surgeon uses the EsophyX device to fold and fasten tissue at the top of the stomach, creating a new anti-reflux valve. This mimics the effect of traditional fundoplication but without the need for abdominal incisions.
- Securing the Tissue: Multiple fasteners (or anchors) are deployed to secure the tissue in place, ensuring a durable and effective barrier against reflux.
- Completion: The devices are withdrawn, and the newly formed valve is left to heal and function as a strengthened LES.
Advantages of TIF Over Traditional Surgery
The TIF procedure represents a significant advancement in minimally invasive surgery for GERD. Its advantages include:
- No External Incisions: As the name implies, TIF is performed entirely through the mouth, leaving no visible scars or wounds.
- Reduced Pain and Faster Recovery: Patients typically experience less postoperative pain and resume normal activity more quickly compared to conventional laparoscopic surgery.
- Low Risk of Complications: The risk of infection, bleeding, and other surgical complications is minimized due to the absence of external incisions and the minimally invasive approach.
- Preservation of Anatomical Integrity: The procedure maintains the stomach’s natural structure and function, which reduces the likelihood of side effects such as gas bloat syndrome and difficulty belching or vomiting.
Who is a Candidate for TIF?
TIF is most suitable for patients with chronic GERD who:
- Continue to experience symptoms despite optimal medical therapy.
- Are seeking an alternative to lifelong medication use.
- Have a small or no hiatal hernia (typically less than 2 cm).
- Do not have significant esophageal motility disorders.
Not all patients are ideal candidates. Those with large hiatal hernias, severe esophageal motility disorders, or advanced esophageal disease may require traditional surgical approaches.
Outcomes and Effectiveness
Multiple clinical studies have demonstrated the safety, durability, and effectiveness of the TIF procedure. Most patients report significant improvement or complete resolution of GERD symptoms, including heartburn and regurgitation, within weeks of the procedure.
Key outcomes observed:
- Up to 80% of patients can discontinue or significantly reduce their acid-suppressive medications after TIF.
- High patient satisfaction rates, due to decreased symptoms and improved quality of life.
- Long-term durability, with studies showing sustained symptom relief at 3- to 5-year follow-ups.
Potential side effects, such as sore throat, mild chest discomfort, or bloating, are generally mild and resolve quickly.
The TIF Procedure: Step-by-Step
The procedure can be summarized in the following stages:
- Preparation: The patient undergoes preoperative evaluation, including an upper endoscopy, esophageal pH testing, and manometry to confirm GERD and assess suitability.
- Anesthesia: The procedure is performed under general anesthesia, typically lasting 45-60 minutes.
- Device Insertion: The EsophyX device and endoscope are advanced through the mouth and into the esophagus.
- Valve Creation: The surgeon manipulates the device to create a 270-degree (partial wrap) or 360-degree (complete wrap) anti-reflux valve at the gastroesophageal junction.
- Deployment of Fasteners: Once the desired valve configuration is achieved, tissue fasteners are placed to secure the new valve.
- Completion and Recovery: The devices are withdrawn, and the patient is monitored in a recovery area. Most patients return home the same or next day.
Recovery and Postoperative Care
Patients typically experience a rapid recovery after the TIF procedure. There may be mild throat soreness or chest discomfort, which usually resolves within days. Most individuals resume light activities within a few days and return to work within a week.
Dietary recommendations post-procedure:
- Start with clear liquids for the first 24-48 hours.
- Gradually advance to a soft diet for about two weeks.
- Return to a regular diet after 2-3 weeks, as tolerated.
Patients are advised to avoid vigorous exercise, heavy lifting, and strenuous activities for at least two weeks. Follow-up appointments are scheduled to monitor healing and assess the effectiveness of the procedure.
Risks and Considerations
While TIF is generally safe and well-tolerated, as with any medical procedure, there are potential risks:
- Bleeding or injury to the esophagus or stomach
- Infection
- Difficulty swallowing (dysphagia)
- Rarely, need for repeat intervention or conversion to traditional surgery
Careful patient selection and an experienced surgical team can minimize these risks.
Comparing TIF with Other Anti-Reflux Treatments
TIF offers a unique middle ground between medical therapy and conventional surgery. Compared to medications, TIF directly addresses the anatomical cause of GERD rather than just controlling symptoms. When compared to laparoscopic fundoplication, TIF provides similar efficacy for appropriately selected patients but with fewer complications, no external scars, and a faster recovery.
Cost and Insurance Coverage
The cost of TIF depends on factors such as location, hospital fees, and insurance coverage. Many insurance providers in North America and Europe now recognize TIF as an established treatment for GERD and cover the procedure when certain criteria are met. Patients are encouraged to consult with their healthcare provider and insurance company for personalized information.
Future Directions and Innovations
As technology continues to advance, the TIF procedure is likely to become even more accessible, efficient, and effective. Ongoing research focuses on refining devices, improving patient selection, and expanding indications. The promise of incisionless endoscopic surgery represents a broader movement in medicine toward less invasive and more patient-friendly solutions.reduce or discontinue using their medications.
Nursing Care of Patients Undergoing Transoral Incisionless Fundoplication (TIF) Procedure
Nurses play a critical role in ensuring the safety, comfort, and optimal outcomes for patients who undergo TIF. This document details the comprehensive nursing care required before, during, and after the procedure.
Pre-procedure Nursing Care
1. Patient Assessment
- Medical History: Review the patient’s history of GERD symptoms, previous treatments, current medications (e.g., proton pump inhibitors), allergies, comorbidities, and prior surgeries.
- Physical Assessment: Conduct baseline vital signs, respiratory assessment, and a focused gastrointestinal evaluation.
- Laboratory and Diagnostic Review: Verify completion and results of required preoperative labs (CBC, electrolytes, coagulation profile) and imaging (endoscopy, pH studies, manometry).
2. Patient Preparation and Education
- Procedure Explanation: Educate the patient about the nature and purpose of TIF, the expected benefits, potential risks, and the steps involved in the procedure.
- Fasting: Instruct the patient to remain nil per os (NPO) for at least 6–8 hours before the procedure to minimize aspiration risk.
- Medication Management: Advise the patient which medications to continue or withhold before the procedure (e.g., anticoagulants, antiplatelets, diabetes medications).
- Consent: Ensure informed consent is obtained and documented.
- Psychosocial Support: Address patient and family concerns, alleviate anxiety, and provide emotional support.
3. Preparation of Equipment
- Verify availability and functionality of endoscopic and monitoring equipment.
- Prepare resuscitation equipment for emergencies (e.g., airway management supplies, suction).
Intra-procedure Nursing Care
1. Monitoring and Safety
- Assist with patient positioning (usually left lateral or supine), ensuring comfort and safety.
- Monitor vital signs (heart rate, blood pressure, oxygen saturation, respiratory rate) continuously.
- Observe for signs of aspiration, airway compromise, bleeding, or hemodynamic instability.
- Ensure proper administration of sedation or anesthesia as prescribed, and monitor for adverse effects.
2. Assisting the Healthcare Team
- Assist the endoscopist or surgeon during the TIF procedure by managing instruments, suction, and patient needs.
- Maintain strict aseptic technique.
- Document intra-procedure findings, medication administration, and events.
Post-procedure Nursing Care
1. Immediate Post-procedure Monitoring
- Transfer the patient to the recovery area and position appropriately (typically head elevated).
- Monitor vital signs and oxygen saturation frequently until stable.
- Assess airway patency and level of consciousness as the patient recovers from anesthesia or sedation.
- Observe for complications such as bleeding, perforation, aspiration, chest pain, or respiratory distress.
- Monitor for abdominal pain, nausea, vomiting, dysphagia, or signs of infection.
- Assess and document pain using appropriate scales, and administer analgesics as ordered.
2. Diet and Nutrition Management
- Initially, keep the patient nil per os (NPO) until fully alert and able to swallow safely.
- Advance diet as per protocol, typically starting with clear liquids, then progressing to full liquids, pureed foods, and soft solids over several weeks.
- Educate the patient to avoid carbonated drinks, caffeine, alcohol, spicy and acidic foods during the initial recovery period.
- Encourage small, frequent meals to reduce pressure on the gastroesophageal junction.
3. Activity and Mobility
- Encourage early mobilization as tolerated to prevent venous thromboembolism and aid recovery.
- Advise the patient to avoid strenuous activity, heavy lifting, or bending for at least 2–4 weeks post-procedure.
4. Medication Management
- Continue prescribed medications, including pain relief and antiemetics, as ordered.
- Monitor for side effects and ensure medication reconciliation at discharge.
- Gradual reduction or discontinuation of reflux medications may occur under physician guidance.
5. Patient Education and Discharge Planning
- Instruct the patient on recognizing and reporting warning signs: severe chest or abdominal pain, fever, difficulty swallowing, persistent vomiting, hematemesis, melena, or respiratory symptoms.
- Educate on the gradual dietary progression and the importance of adhering to restrictions during healing.
- Emphasize the need for regular follow-up appointments for symptom assessment and outcome evaluation.
- Provide written and verbal instructions regarding wound care if applicable, medication regimen, activity, and return-to-work guidelines.
- Offer contact information for questions or emergencies.
Potential Complications and Nursing Interventions
- Bleeding: Monitor for hematemesis, melena, tachycardia, hypotension; report promptly and support interventions as needed.
- Perforation: Observe for severe chest or abdominal pain, subcutaneous emphysema, dyspnea, fever; initiate emergency protocols if suspected.
- Infection: Monitor vital signs, inspect for fever, chills, local tenderness, or discharge; administer antibiotics as ordered.
- Respiratory Complications: Maintain airway patency, monitor oxygenation, provide supplemental oxygen if indicated, and report signs of aspiration or distress.
- Dysphagia or Obstruction: Assess swallowing ability and dietary tolerance; alert provider to persistent issues.
Psychosocial Aspects and Support
- Provide reassurance regarding recovery expectations and outcomes.
- Offer support for anxiety, particularly regarding dietary modifications and lifestyle adjustments.
- Involve family members or caregivers in education to ensure continuity of care at home.
Documentation
- Accurately record all assessments, interventions, patient responses, and education provided.
- Document any complications, provider notifications, and related actions taken.
REFERENCES
- Fass R. An Overview of Transoral Incisionless Fundoplication and Magnetic Sphincter Augmentation for GERD. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5390325/. Gastroenterol Hepatol (N Y). 2017 Jan;13(1):50-52.
- Håkansson B, et al. Randomised clinical trial: Transoral incisionless fundoplication vs. sham intervention to control chronic GERD. Alimentary Pharmacology and Therapeutics. 2015;42:1261.
- Shen S, Yu G, Guo X, Zong G, Wang C, et al. The long-term efficacy of transoral incisionless fundoplication with Medigus Ultrasonic Surgical Endostapler (MUSE) for gastroesophageal reflux disease. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10234897/. Esophagus. 2023 Jul;20(3):581-586.
- Mahfouz M, et al. (2021). Advances in endoscopic management of GERD: A brief review on TIF procedure.
https://practicalgastro.com/wp-content/uploads/2021/02/Adler-January-2021.pdf - Testoni PA, Mazzoleni G, Testoni SG. Transoral incisionless fundoplication for gastro-esophageal reflux disease: Techniques and outcomes. World J Gastrointest Pharmacol Ther. 2016 May 6;7(2):179-89.
- Testoni PA, et al. (2019). Transoral incisionless fundoplication with EsophyX for gastroesophageal reflux disease: Clinical efficacy is maintained up to 10 years.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6497496/ - Gisi C, et al. (2020). Efficacy and patient satisfaction of single-session transoral incisionless fundoplication and laparoscopic hernia repair.
https://link.springer.com/article/10.1007/s00464-020-07796-x
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





