A nursing care plan on myasthenia gravis addresses muscle weakness, fatigue, and risk for aspiration. Nurses monitor respiratory status, assist with mobility, and educate patients on medication timing, energy conservation, and signs of crisis—supporting safe, coordinated care.
Myasthenia gravis (MG) is an autoimmune disorder of the neuromuscular junction. This condition is characterized by fluctuating weakness of skeletal muscle groups that worsens with use and improves with rest.
MG involves an autoimmune process in which antibodies attack the ACh receptors (AChR), resulting in fewer AChR at the neuromuscular junction. When this occurs, ACh molecules are not able to attach to these receptors and stimulate muscle contractions.
The classic sign of MG is fluctuating weakness of the skeletal muscles. This condition affects multiple muscle groups including muscles used to move the eyes and eyelids, and muscles for chewing, breathing, and speaking. Muscle weakness typically occurs with continued activity and becomes prominent by the end of the day.
The course of this condition is highly variable. Some patients become stabilized while others will have short-term remission between flare-ups and others develop severe symptoms. Various conditions can exacerbate MG including pregnancy, trauma, illness, stress, extreme temperature changes, and hypokalemia.
Diagnosis of MG may be based on the patient’s history and physical examination. However, diagnostic tests like electromyography (EMG) or a tensilon test may be performed to confirm the diagnosis.
Nursing Process
Since MG is a chronic and progressive medical condition, nurses support patients through ongoing assessments, treatment interventions, and providing accurate patient education about the disease, prognosis, treatments, and prevention of complications.
Nursing Assessment
Nursing assessment for Myasthenia Gravis (MG) focuses on evaluating neuromuscular function, identifying complications, and ensuring patient safety. Here are key components:
Initial Evaluation
The initial evaluation of a patient with MG involves a comprehensive medical history and physical examination. Key aspects to assess include:
Medical History
Review the patient’s history for potential symptoms of MG, such as muscle weakness that worsens with activity and improves with rest, ptosis (drooping of the eyelids), dysphagia (difficulty swallowing), and double vision. Inquire about the onset, duration, and progression of symptoms, as well as any factors that exacerbate or alleviate them. Assess for a history of autoimmune disorders, thymoma (a tumor of the thymus gland), and any use of medications that may affect neuromuscular transmission.
Physical Examination
Conduct a thorough physical examination focusing on muscle strength, particularly in the eyes, face, and limbs. Assess for signs of ptosis, facial weakness, and fatigue. Evaluate speech and swallowing function. Perform specific tests such as the ice pack test (applying ice to the eyelids to temporarily improve ptosis) and the tensilon test (administering edrophonium to temporarily improve muscle strength).
Diagnostic Tests
Consider ordering diagnostic tests such as electromyography (EMG) to assess electrical activity in muscles, repetitive nerve stimulation tests to detect abnormal neuromuscular transmission, and blood tests to identify antibodies against acetylcholine receptors or muscle-specific kinase (MuSK). Imaging studies such as chest CT or MRI may be used to detect thymoma.
Nursing Intervention
Nursing interventions for Myasthenia Gravis (MG) focus on managing symptoms, preventing complications, and improving the patient’s quality of life. Here are some key interventions:
Medication Management
Medications play a central role in the management of MG. Nurses are responsible for administering and monitoring these medications to ensure their efficacy and manage potential side effects.
- Anticholinesterase Inhibitors: These medications, such as pyridostigmine, improve neuromuscular transmission and muscle strength. Monitor the patient for signs of cholinergic crisis, such as muscle twitching, increased salivation, and severe weakness.
- Immunosuppressants: Medications such as corticosteroids, azathioprine, and mycophenolate mofetil are used to suppress the immune response. Monitor the patient for side effects, including increased risk of infection, hypertension, and gastrointestinal issues.
- Intravenous Immunoglobulin (IVIG) and Plasmapheresis: These treatments are used for acute exacerbations. IVIG provides antibodies to modulate the immune response, while plasmapheresis removes antibodies from the blood. Monitor the patient for adverse reactions such as headache, fever, and allergic reactions.
Symptom Management
Effective symptom management is essential to improve the patient’s quality of life and prevent complications.
- Energy Conservation: Educate the patient on energy conservation techniques, such as taking frequent rest breaks, planning activities during peak energy times, and avoiding strenuous activities.
- Swallowing and Aspiration Precautions: Implement strategies to prevent aspiration, such as providing a soft diet, encouraging small, frequent meals, and positioning the patient upright during and after meals. Monitor for signs of aspiration, such as coughing, choking, and changes in voice quality.
- Eye Care: Provide eye care to manage symptoms of ptosis and diplopia. Encourage the use of lubricating eye drops, taping the eyelids at night, and using eyepatches to manage double vision.
Patient Education
Patient education is a vital component of MG management, empowering patients to take an active role in their care.
- Medication Adherence: Educate the patient on the importance of adhering to their medication regimen and the potential consequences of missed doses. Provide information on how to manage side effects and when to seek medical attention.
- Recognizing Exacerbations: Teach the patient to recognize early signs of MG exacerbations, such as increased muscle weakness, difficulty swallowing, and respiratory distress. Provide instructions on when to seek emergency care.
- Lifestyle Modifications: Encourage the patient to adopt a healthy lifestyle, including a balanced diet, regular exercise, and stress management techniques. Educate them on the importance of avoiding triggers, such as infections, stress, and certain medications.
Community Integration
Facilitating community integration helps patients with MG reintegrate into society and maintain a sense of normalcy.
Access to Resources
Assist patients in accessing community resources such as support groups, recreational activities, and vocational training programs. Provide information on available services and how to utilize them effectively.
Collaboration with Social Workers
Work with social workers to provide financial assistance, connect patients with community services, and advocate for their needs. Address any barriers to accessing care, such as transportation or insurance issues.
School and Workplace Collaboration
Collaborate with school personnel and employers to ensure that patients with MG receive the necessary support and accommodations. Participate in Individualized Education Program (IEP) meetings and advocate for appropriate educational services. Work with employers to provide reasonable workplace accommodations, such as flexible work hours and modified job duties.
Nursing Care Plans
Once the nurse identifies nursing diagnoses for myasthenia gravis, nursing care plans help prioritize assessments and interventions for both short and long-term goals of care. In the following section, you will find nursing care plan examples for myasthenia gravis.
Fatigue
Myasthenia gravis is associated with muscle weakness and rapid fatigue in voluntary muscle groups.
Nursing Diagnosis: Fatigue
Related to:
- Disease process
- Muscle weakness
As evidenced by:
- Decreased gait velocity
- Difficulty maintaining usual physical activity
- Difficulty maintaining usual routines
- Ptosis
- Diplopia
- Weak facial expressions
- Expresses tiredness
- Expresses weakness
- Inadequate role performance
- Lethargy
- Falls
Expected outcomes:
- The patient will demonstrate increased activity levels and participate in desired activities
- The patient will participate in supportive therapy to improve fatigue and muscle strength
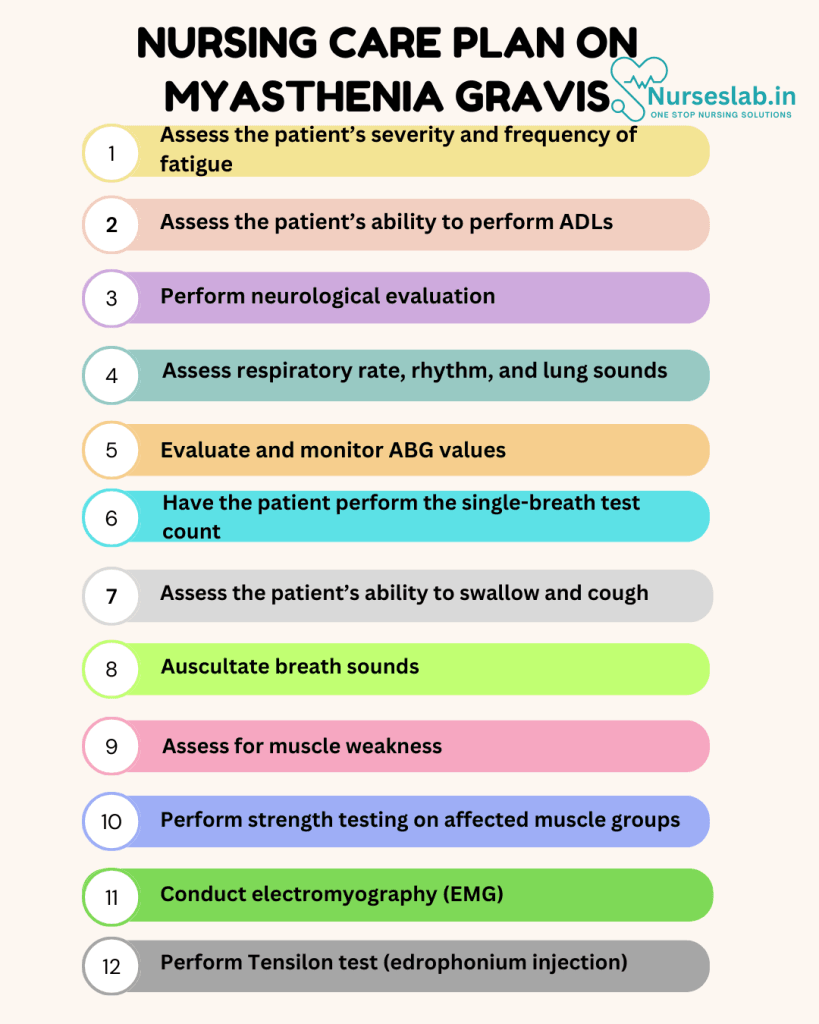
Assessment:
1. Assess the patient’s severity and frequency of fatigue.
Assessing fatigue severity and frequency can help formulate the most appropriate treatment plan for the patient. Fatigue can lead to falls, injuries, and poor quality of life if not properly evaluated.
2. Assess the patient’s ability to perform ADLs.
This will help determine the degree of assistance that the patient will require in performing self-care and other activities of daily living.
3. Perform neurological evaluation.
The nurse should perform a neurological assessment to determine fatigue of the eyes, face, and reflexes.
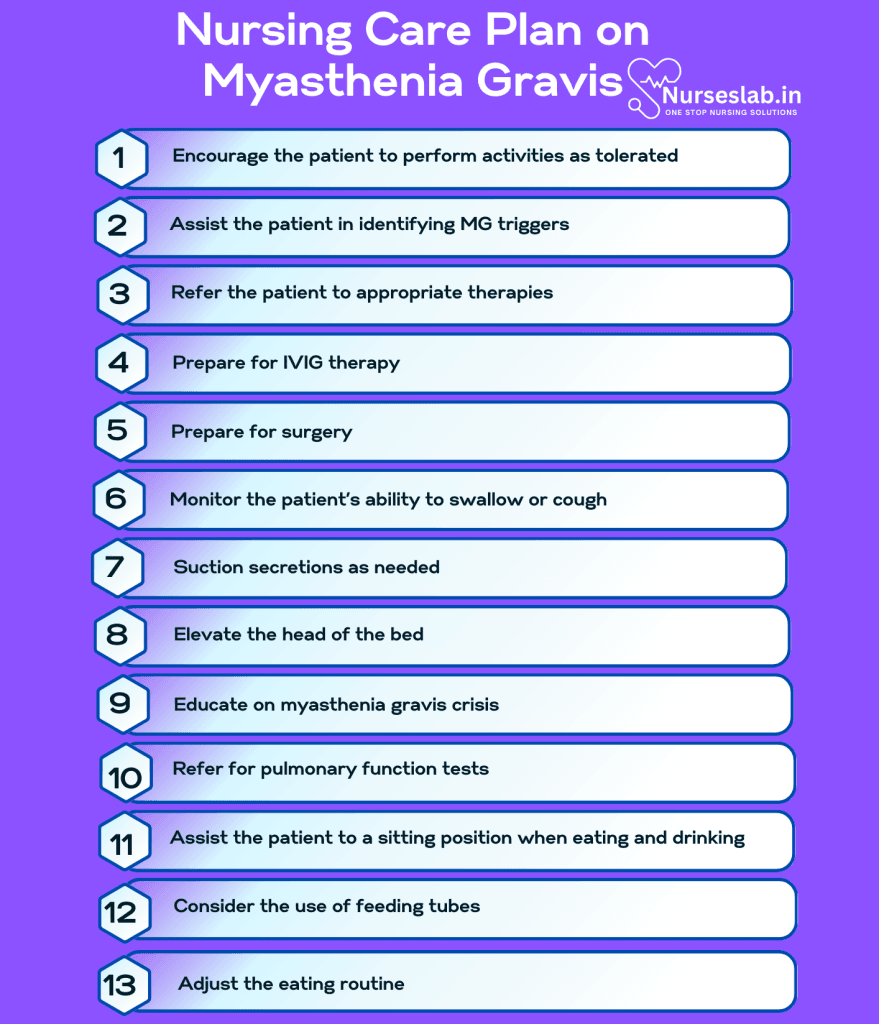
Interventions:
1. Encourage the patient to perform activities as tolerated.
Allowing the patient to perform activities of daily living with adequate rest periods in between will promote a sense of control and independence.
2. Assist the patient in identifying MG triggers.
A patient can prevent an MG flare by understanding their triggers. Common triggers include illness/infections, inadequate sleep, some medications, extreme temperatures, menstruation, alcohol, and stress.
3. Refer the patient to appropriate therapies.
Physical therapy and occupational therapy can assist with motor strength exercises and recommend strategies and equipment to assist with ADLs.
4. Prepare for IVIG therapy.
Intravenous immunoglobulin (IVIG) is a transfused blood product that is believed to destroy damaged antibodies through healthy donor antibodies. A nurse can administer the transfusion in a medical office or the patient’s home. This treatment can be given for an MG crisis, to prevent an impending crisis, or as a treatment to stabilize the patient prior to surgery.
5. Prepare for surgery.
For some patients, the thymus gland itself or a tumor in the thymus gland (known as a thymoma) may contribute to MG. In an attempt to reduce symptoms, and in some cases cure patients, a thymectomy is performed.
Ineffective Airway Clearance
Myasthenia gravis is associated with muscle weakness usually affecting the muscles that control the eyes, throat, mouth, and limbs that worsen with activity. Weakness in the upper airway muscles can result in upper airway obstruction and respiratory failure.
Nursing Diagnosis: Ineffective Airway Clearance
Related to:
- Disease process
- Weak oropharyngeal muscle contractions
- Decreased ability to cough and swallow
As evidenced by:
- Absent or ineffective cough
- Adventitious breath sounds
- Altered respiratory rhythm
- Rapid, shallow breathing
- Cyanosis
- Difficulty verbalizing
- Nasal flaring
Expected outcomes:
- The patient will demonstrate effective coughing, clear breath sounds, and clear airways without respiratory distress symptoms
- The patient will verbalize one strategy to maintain airway strength and support
Assessment:
1. Assess respiratory rate, rhythm, and lung sounds.
Diminished lung sounds or the presence of adventitious lung sounds can indicate a blocked airway. Alterations in respiratory rate and rhythm are present when there is an attempt to compensate for ineffective airway clearance and breathing.
2. Evaluate and monitor ABG values.
Alterations in the patient’s ABG levels can indicate worsening respiratory failure. Do not rely on this information for treatment as abnormal values may not be obvious until respiratory failure is occurring.
3. Have the patient perform the single-breath test count.
This test has the patient inhale a maximal breath and then count out loud as long as they can before taking another breath. The ability to count to 50 indicates normal breathing. A count of less than 15 signals respiratory muscle weakness.
Interventions:
1. Monitor the patient’s ability to swallow or cough.
Since the primary symptom of MG is muscle weakness, it is important to monitor the patient’s ability to swallow or cough. This can help determine the progression of the disease and the need for additional interventions to protect the patient’s airway.
2. Suction secretions as needed.
Suctioning secretions help patients with MG who are unable to cough or swallow.
3. Elevate the head of the bed.
Elevating the head of the bed improves lung expansion and makes breathing easier.
4. Educate on myasthenia gravis crisis.
An MG crisis occurs when the respiratory muscles weaken and result in respiratory failure. This can be life-threatening and requires emergency assistance. Educate the client to seek assistance if they notice dyspnea, accessory muscle use, and a weak cough.
5. Refer for pulmonary function tests.
PFTs can assist in diagnosing MG as well as monitoring the progression of the disease. Not all patients will experience respiratory muscle involvement, but routine assessment can help prevent a crisis or other complications.
Risk for Aspiration
Dysphagia or swallowing difficulties are common in patients diagnosed with MG, making the risk for aspiration high. Silent aspiration can also occur in MG due to weak oropharyngeal muscle contractions, resulting in myasthenic crisis and aspiration pneumonia.
Nursing Diagnosis: Risk for Aspiration
Related to:
- Disease process
- Weak oropharyngeal muscle contractions
- Depressed gag reflex
As evidenced by:
A risk diagnosis is not evidenced by signs and symptoms, as the problem has not occurred yet and nursing interventions are directed at the prevention of symptoms.
Expected outcomes:
- The patient will maintain a patent airway and demonstrate clear breath sounds
- The patient will demonstrate strategies to safely swallow
Assessment:
1. Assess the patient’s ability to swallow and cough.
Assessing the patient’s swallow and gag reflexes is necessary to reduce the risk of aspiration and maintain clear airways.
2. Auscultate breath sounds.
Breath sounds assess the patient’s pulmonary status. Coarse crackles are often heard during auscultation with aspiration.
Interventions:
1. Assist the patient to a sitting position when eating and drinking.
Keeping the patient in an upright position while eating or drinking, and for 30 minutes following meals, can help prevent aspiration.
2. Consider the use of feeding tubes.
In severe cases of MG, a nasogastric feeding tube may be required for dysphagia until the client recovers from their MG flare.
3. Administer medications as indicated.
Medications like pyridostigmine are prescribed to help alleviate symptoms of MG.
4. Adjust the eating routine.
Educate the patient to eat when they have optimal muscle strength. Take time to chew, and focus on smaller meals. Choosing softer foods will require less chewing.
5. Consult with speech therapy.
A speech therapist can perform swallowing assessments and determine foods that are safe or unsafe to eat. They can also work with the client on strengthening their mouth and throat muscles.
Nursing Diagnoses and Rationales for Myasthenia Gravis
1. Ineffective Airway Clearance
Rationale: Patients with Myasthenia Gravis (MG) often experience weakness of the respiratory muscles, which can lead to difficulty in clearing airway secretions. Ensuring proper airway management through techniques like chest physiotherapy, suctioning, and monitoring respiratory status is crucial. Educating patients and caregivers on signs of respiratory distress and emergency procedures can also be beneficial.
2. Impaired Physical Mobility
Rationale: Muscle weakness and fatigue are hallmark symptoms of MG, significantly impacting a patient’s ability to move and perform daily activities. Encouraging rest periods, providing assistive devices, and creating a safe environment can help manage mobility issues. Physical therapy may also be recommended to maintain muscle strength and function.
3. Risk for Activity Intolerance
Rationale: Due to the fluctuating nature of muscle strength in MG, patients may experience activity intolerance. Establishing a balanced activity schedule, pacing activities, and monitoring for signs of fatigue can prevent overexertion. Educating patients on energy conservation techniques and the importance of rest is also vital.
4. Impaired Swallowing
Rationale: Weakness of the bulbar muscles can cause dysphagia, increasing the risk of aspiration and malnutrition. Assessing swallowing function, modifying food texture, and providing small, frequent meals can aid in safe swallowing. Close collaboration with speech-language pathologists may be necessary for individualized swallowing therapy.
5. Disturbed Sensory Perception
Rationale: Diplopia and ptosis are common ocular manifestations of MG, leading to visual disturbances. Providing eye protection, using eye patches, and ensuring adequate lighting can help manage these symptoms. Regular ophthalmologic evaluations are important to monitor and address changes in vision.
6. Fatigue
Rationale: Chronic fatigue is a significant concern for patients with MG. Assessing fatigue levels, encouraging rest periods, and promoting a balanced diet can help manage fatigue. Patient education on the importance of medication adherence and possible side effects is also essential.
7. Anxiety
Rationale: Living with a chronic and unpredictable illness like MG can cause significant anxiety. Providing emotional support, facilitating open communication, and involving mental health professionals can help alleviate anxiety. Relaxation techniques and stress management strategies can also be beneficial.
8. Deficient Knowledge
Rationale: Patients and families may lack knowledge about MG and its management. Providing comprehensive education on the disease, treatment options, and coping strategies can empower patients and families. Involvement in support groups and access to reliable resources can enhance understanding and support.
9. Risk for Aspiration
Rationale: Due to weakness of the throat muscles, patients with MG are at risk for aspiration during eating and drinking. Implementing swallowing assessments, modifying diet consistency, and teaching patients safe swallowing techniques can reduce this risk. Continuous monitoring during meals is essential for early detection of aspiration signs.
10. Impaired Social Interaction
Rationale: The physical limitations and fatigue associated with MG can hinder social interaction and participation in activities. Encouraging involvement in social activities within comfortable limits, providing emotional support, and arranging for community resources can help improve social engagement and quality of life.
REFERENCES
- ACCN Essentials of Critical Care Nursing. 3rd Edition. Suzanne M. Burns, MSN, RRT, ACNP, CCRN, FAAN, FCCM, FAANP. 2014. McGraw Hill Education.
- Medical-Surgical Nursing: Concepts for Interprofessional Collaborative Care. 9th Edition. Donna D. Ignatavicius, MS, RN, CNE, ANEF. 2018. Elsevier, Inc.
- Myasthenia Gravis Fact Sheet. NIH: National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/myasthenia-gravis-fact-sheet
- Gilhus, N. E., & Verschuuren, J. J. (2015). Myasthenia gravis: subgroup classification and therapeutic strategies. The Lancet Neurology, 14(10), 1023-1036.
- Hehir, M. K., & Silvestri, N. J. (2018). Generalized Myasthenia Gravis: Classification, Clinical Presentation, Natural History, and Epidemiology. Neurologic Clinics, 36(2), 253-260.
- Melzer, N., Ruck, T., Fuhr, P., Gold, R., Hohlfeld, R., Marx, A., … & Wiendl, H. (2016). Clinical features, pathogenesis, and treatment of myasthenia gravis: a supplement to the Guidelines of the German Neurological Society. Journal of Neurology, 263(8), 1473-1494.
- Norwood, F., Dhanjal, M., Hill, M., James, N., Jungbluth, H., Kyle, P., … & Hilton-Jones, D. (2014). Myasthenia in pregnancy: best practice guidelines from a UK multispecialty working group. Journal of Neurology, Neurosurgery & Psychiatry, 85(5), 538-543.
- Sanders, D. B., Wolfe, G. I., Benatar, M., Evoli, A., Gilhus, N. E., Illa, I., … & Kaminski, H. J. (2016). International consensus guidance for management of myasthenia gravis: Executive summary. Neurology, 87(4), 419-425.
- Wendell, L. C., & Levine, J. M. (2011). Myasthenic crisis. The Neurohospitalist, 1(1), 16-22.
- Myasthenia Gravis. Johns Hopkins Medicine. 2022. From: https://www.hopkinsmedicine.org/health/conditions-and-diseases/myasthenia-gravis
- Myasthenia gravis. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/myasthenia-gravis/symptoms-causes/syc-20352036
- Myasthenia Gravis. Medscape. Abbas A Jowkar, MBBS. https://emedicine.medscape.com/article/1171206-overview
- Myasthenic crisis. Neurohospitalist. Wendell LC, Levine JM. 2011 Jan;1(1):16-22. doi: 10.1177/1941875210382918. PMID: 23983833; PMCID: PMC3726100.
- Myasthenia gravis. NHS. https://www.nhs.uk/conditions/myasthenia-gravis/
- Nursing care of the patient with myasthenia gravis. Donohoe KM. Neurol Clin. 1994 May;12(2):369-85. PMID: 8041347.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.







