A nursing care plan on syncope addresses sudden loss of consciousness due to reduced cerebral perfusion. Nurses assess vital signs, monitor cardiac status, prevent injury, and educate patients on hydration, posture changes, and medication adherence.
Syncope is referred to as a brief lapse in consciousness causing fainting which is related to insufficient blood flow to the brain. Syncope is not usually a cause for concern but can be a warning sign for other illnesses.
Common causes of syncope include the following:
- Cardiac Syncope – If syncope occurs frequently and suddenly it may be related to cardiac issues such as aortic dissection, arrhythmia, or aortic valve stenosis.
- Reflex Syncope – This condition is caused by a trigger that slows the heart or dilates the blood vessels, causing blood pressure to drop and decreasing blood flow to the brain.
- Vasovagal Syncope – This is the most common type of reflex syncope and is triggered by dehydration, sudden change to an upright position, and emotions.
- Situational Syncope – This type of reflex syncope occurs with coughing, chest pressure after exercise, and straining with defecation.
- Carotid Sinus Syncope – Syncope can occur when there is pressure applied to the carotid artery like a tight collar or hand pressure.
- Orthostatic Hypotension – This condition occurs because of low blood pressure when standing up, causing decreased blood flow to the brain.
Syncope can be benign or a symptom of an underlying health condition. It is critical to identify the cause of syncope to initiate appropriate and timely interventions. Diagnostic tests may be ordered including:
- Electrocardiogram (ECG)
- Exercise stress test
- Echocardiogram
- Tilt table test
- Electrophysiology study
- Holter monitor
Nursing Process
Identification and treatment of the underlying condition, reducing risk for injuries, and prevention of complications are the primary goals in the management of syncope. Nurses play an essential role in all phases of the treatment regimen for patients with syncope as they are responsible for the identification of at-risk patients through obtaining a comprehensive history as well as preparing for testing and preventing falls and complications.
Nursing Assessment
The initial evaluation of a patient presenting with syncope involves a detailed medical history and physical examination. Key aspects to assess include:
Medical History:
- Evaluate the patient’s history for risk factors such as cardiovascular disease, neurological conditions, or metabolic disorders.
- Inquire about the circumstances surrounding the syncopal event, including any potential triggers, duration of unconsciousness, and associated symptoms such as palpitations, chest pain, or shortness of breath.
- Ask about any family history of syncope, sudden cardiac death, or hereditary conditions that may predispose the patient to syncope.
Physical Examination:
- Perform a comprehensive physical examination focusing on cardiovascular, neurological, and respiratory systems.
- Check vital signs, including blood pressure and heart rate, both in supine and standing positions (orthostatic measurements) to identify orthostatic hypotension.
- Assess for signs of cardiac abnormalities, such as irregular heart rhythms or murmurs, and for neurological deficits that may indicate a central nervous system cause.
Laboratory Tests and Diagnostic Studies:
- Obtain baseline laboratory tests, including complete blood count (CBC), electrolyte levels, and blood glucose levels, to identify metabolic or hematologic causes of syncope.
- Conduct electrocardiography (ECG) to detect arrhythmias, ischemia, or other cardiac abnormalities that may contribute to syncope.
- Consider additional diagnostic studies, such as echocardiography, Holter monitoring, or tilt-table testing, based on the patient’s clinical presentation and initial findings.
Nursing Interventions
Nursing interventions play a crucial role in the effective management of syncope. By conducting thorough evaluations, implementing immediate and long-term interventions, and providing comprehensive patient education, nurses can significantly improve patient outcomes and quality of life.
Immediate Management
The immediate management of a patient who has experienced syncope focuses on ensuring patient safety and stabilizing their condition. Key interventions include:
- Position the patient supine with legs elevated to promote cerebral perfusion and prevent further episodes of syncope.
- Monitor vital signs and level of consciousness closely, and provide supplemental oxygen if needed.
- Administer intravenous fluids if the patient shows signs of dehydration or hypotension.
Long-Term Management
Long-term management of syncope involves identifying and addressing the underlying cause, preventing recurrence, and providing patient education. Key aspects include:
Addressing Underlying Causes:
- Implement appropriate medical or surgical treatments for identified causes of syncope, such as arrhythmias, structural heart disease, or neurological conditions.
- Adjust medications that may contribute to syncope, under the guidance of a healthcare provider.
Patient Education:
- Educate patients and their families about the importance of adherence to prescribed treatments and lifestyle modifications to prevent recurrence of syncope.
- Teach patients to recognize early warning signs of syncope and to take preventive measures, such as sitting or lying down at the onset of symptoms.
- Encourage patients to avoid triggers that may precipitate syncope, such as dehydration, prolonged standing, or excessive heat exposure.
Follow-Up Care:
- Schedule regular follow-up appointments to monitor the patient’s condition, adjust treatment plans as needed, and reinforce patient education.
- Refer patients to specialists, such as cardiologists or neurologists, for further evaluation and management as appropriate.
Nursing Care Plans
Once the nurse identifies nursing diagnoses for syncope, nursing care plans help prioritize assessments and interventions for both short and long-term goals of care. In the following section, you will find nursing care plan examples for syncope.
Anxiety
Patients who have known episodes of syncope are often stressed and anxious about the recurrence of the attacks. Safety precautions must be initiated along with interventions that can help reduce episodes.
Nursing Diagnosis: Anxiety
Related to:
- Stressors
- Unfamiliar situations
- Recurrence of syncope episodes
- Risk of injury/falls
- Strong emotions
As evidenced by:
- Expresses anxiety about life event changes
- Expresses distress
- Expresses insecurity
- Expresses helplessness
Expected Outcomes:
- The patient will demonstrate techniques that help reduce anxiety
- The patient will report a reduced sense of anxiety and control over syncope
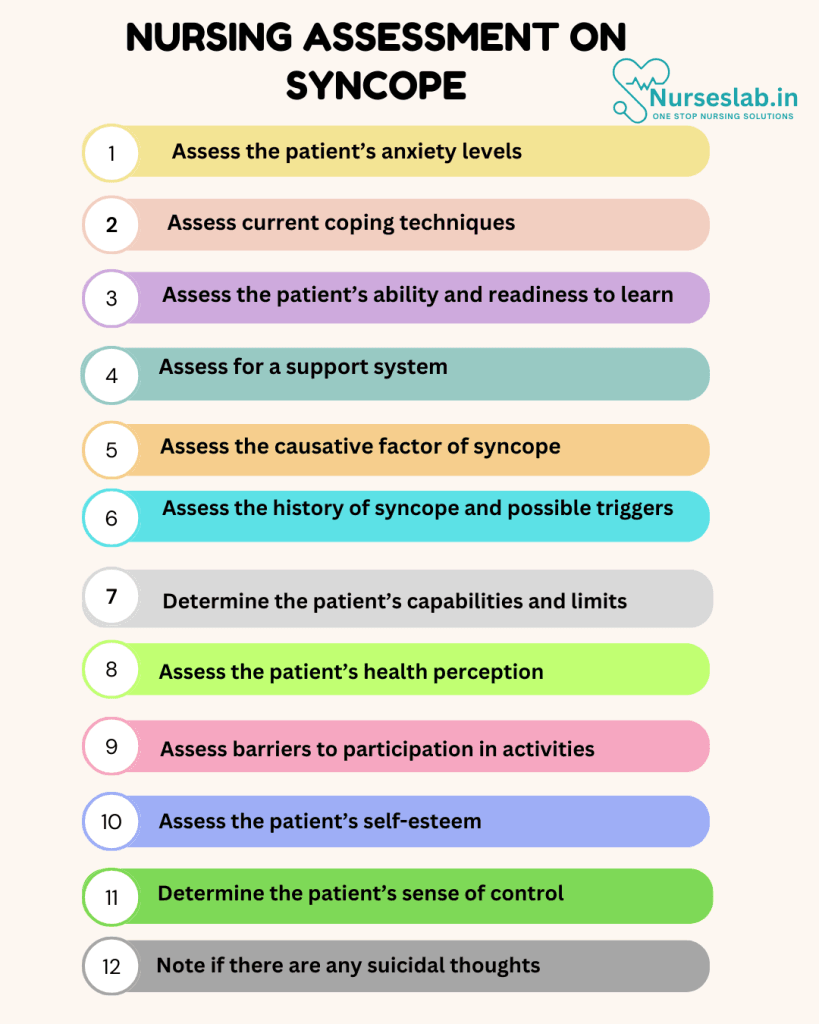
Assessment:
1. Assess the patient’s anxiety levels.
Anxiety can affect the patient’s functional ability along with adherence to treatment regimens. Assess if anxiety is preventing the patient from usual activities.
2. Assess current coping techniques.
Assessing how the patient is currently coping with anxiety related to syncope can help the nurse understand what may or may not help.
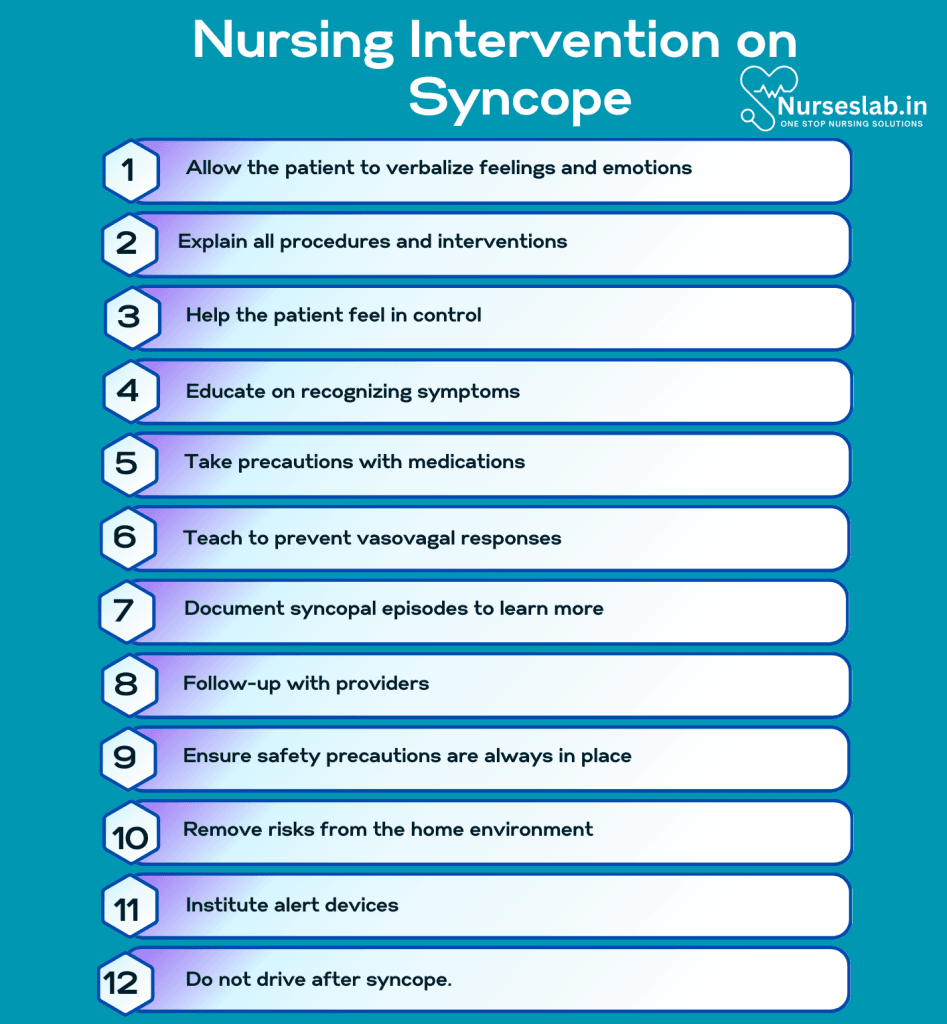
Interventions:
1. Allow the patient to verbalize feelings and emotions.
Establish trust and build a rapport so the patient feels comfortable discussing their anxiety.
2. Explain all procedures and interventions.
Investigating syncope can provide answers to prevent further occurrences. Prepare the client for tests such as stress tests, tilt table tests, and wearing a Holter monitor.
3. Help the patient feel in control.
Losing consciousness can be frightening, especially if the patient sustained an injury from a past episode. Help the patient gain control of syncope by arming them with information about the types, triggers, and treatments.
4. Educate on recognizing symptoms.
Not all patients will have pre-syncopal symptoms, but instruct the patient that if they feel dizzy, light-headed, diaphoretic, or nauseous, that fainting could occur and they should prepare by sitting down or alerting someone.
Deficient Knowledge
Syncope may not always have a cause and may only occur once, but patient education is important to understand the condition and to be alert for possible underlying causes.
Nursing Diagnosis: Deficient Knowledge
Related to:
- Misinformation
- Inadequate information
- Inadequate interest in learning
- Inadequate participation in care planning
As evidenced by:
- Inaccurate follow-through of instructions
- Inaccurate statements about a topic
- Recurring syncopal episodes
Expected Outcomes:
- The patient will verbalize understanding of the disease process and appropriate interventions
- The patient will participate in tests to further investigate syncope
Assessment:
1. Assess the patient’s ability and readiness to learn.
The patient’s ability to comprehend and readiness to learn can contribute to the success or failure of patient education.
2. Assess for a support system.
Family members may also need to be educated on recognizing and intervening if pre-syncopal symptoms occur or what to do when the patient faints.
Interventions:
1. Take precautions with medications.
Diuretics and antihypertensives can cause dehydration or worsen orthostatic hypotension. Ensure the patient understands the side effects of their medications.
2. Teach to prevent vasovagal responses.
Since vasovagal syncope is the most common type of syncope, educate the patient on avoiding triggers such as the sight of blood, standing up too quickly, standing too long, and intense fear or stress.
3. Document syncopal episodes to learn more.
If syncope is recurring, have the patient or family member document events surrounding the episode, where it occurred, the time of day, how long it lasted, and how the patient felt afterward. This information can identify triggers or underlying conditions.
4. Follow-up with providers.
Instruct the patient to adhere to discharge instructions such as following up with a cardiologist if syncope is suspected to be related to a cardiac event.
Risk for Injury
Syncope can occur suddenly with or without warning. Patients suffering from syncope have an increased risk of injury and falls.
Nursing Diagnosis: Risk for Injury
Related to:
- Altered psychomotor performance
- A sudden decrease in blood pressure
- Decreased blood flow to the brain
- Disease processes
- Transient loss of consciousness
- Falls
- Altered sensory perception
As evidenced by:
A risk diagnosis is not evidenced by signs and symptoms, as the problem has not occurred yet and nursing interventions are directed at the prevention of symptoms.
Expected Outcomes:
- The patient will verbalize an understanding of risks and demonstrate precautions to avoid falls or injuries
- The patient will remain free of injury
Assessment:
1. Assess the causative factor of syncope.
Syncope can be benign or a symptom of an underlying health condition. Identifying a possible causative factor can direct treatment and prevent further episodes.
2. Assess the history of syncope and possible triggers.
Assess how frequently episodes of syncope or dizziness occur to determine possible triggers.
Interventions:
1. Ensure safety precautions are always in place.
Safety precautions like keeping side rails up and keeping the bed in the lowest position with the call bell within reach will help reduce falls.
2. Remove risks from the home environment.
Reduce the risk of injury and falls by not navigating stairs and using assistive devices.
3. Institute alert devices.
Patients who experience a syncopal episode may end up falling. Ensure they can call for help by using a Life Alert bracelet/necklace or other emergency system.
4. Do not drive after syncope.
Instruct the patient not to drive or participate in risky activities such as using dangerous equipment or ladders after syncope.
Nursing Diagnoses and Rationales for Syncope
1. Risk for Injury
Rationale: Patients experiencing syncope are at a heightened risk for injury due to sudden loss of consciousness and subsequent falls. Implementing fall prevention strategies, such as ensuring a safe environment, using assistive devices, and educating patients on the importance of rising slowly from a seated or lying position, can mitigate this risk.
2. Decreased Cardiac Output
Rationale: Syncope can be a result of decreased cardiac output due to various cardiovascular conditions. Monitoring vital signs, assessing for signs of heart failure, and promoting adherence to prescribed cardiovascular medications can help manage and prevent episodes of syncope.
3. Anxiety
Rationale: The unpredictability of syncope episodes can lead to significant anxiety and fear in patients. Providing emotional support, offering information about the condition, and teaching relaxation techniques can help alleviate anxiety and improve the patient’s quality of life.
4. Activity Intolerance
Rationale: Patients with syncope may experience limitations in their activity levels due to the fear of experiencing an episode during exertion. Assessing activity tolerance, developing a gradual exercise plan, and providing education on safe activity practices can enhance physical endurance and confidence.
5. Knowledge Deficit
Rationale: Patients may lack understanding of the causes, triggers, and management of syncope. Educating patients about their condition, including potential triggers and lifestyle modifications, can empower them to manage their health more effectively and prevent future episodes.
6. Ineffective Tissue Perfusion
Rationale: Syncope may occur due to inadequate tissue perfusion, particularly in cases of neurocardiogenic syncope. Monitoring for signs of poor perfusion, such as pallor and delayed capillary refill, and promoting interventions to improve circulation, such as adequate hydration and vasovagal maneuver techniques, are essential components of care.
REFERENCES
- ACCN Essentials of Critical Care Nursing. 3rd Edition. Suzanne M. Burns, MSN, RRT, ACNP, CCRN, FAAN, FCCM, FAANP. 2014. McGraw Hill Education.
- Medical-Surgical Nursing: Concepts for Interprofessional Collaborative Care. 9th Edition. Donna D. Ignatavicius, MS, RN, CNE, ANEF. 2018. Elsevier, Inc.
- Johnson, M., & Bulechek, G. (2023). Nursing Outcomes Classification (NOC). Elsevier Health Sciences.
- Herdman, T. H., & Kamitsuru, S. (2023). NANDA International Nursing Diagnoses: Definitions & Classification 2024-2026. Thieme.
- Brignole, M., et al. (2023). 2023 ESC Guidelines for the diagnosis and management of syncope. European Heart Journal, 44(30), 2603-2690.
- Sun, B. C., & Costantino, G. (2023). Syncope Risk Stratification in the Emergency Department. Circulation, 147(10), 784-797.
- Kenny, R. A., & McNicholas, T. (2024). The management of syncope in older adults: A practical approach. Age and Ageing, 53(1), afad245.
- Sheldon, R. S., & Grubb, B. P. (2023). Contemporary management of syncope: A comprehensive guide. Journal of the American Heart Association, 12(2), e027789.
- Syncope. Cleveland Clinic. Updated May 14, 2019. From: https://my.clevelandclinic.org/health/diseases/17536-syncope
- Syncope (Fainting). American Heart Association. Last Reviewed: Jun 30, 2017. From: https://www.heart.org/en/health-topics/arrhythmia/symptoms-diagnosis–monitoring-of-arrhythmia/syncope-fainting
- Syncope. Grossman SA, Badireddy M. [Updated 2022 Jun 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK442006/
- Syncope. Morag, MD, FACEP. The Heart.org. Medscape. Updated: Jan 13, 2017. From: https://emedicine.medscape.com/article/811669-overview
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.







