Depression is a mood disorder characterized by intense and persistent feelings of sadness and a loss of interest or enjoyment in things once loved. Major depressive disorder affects how you think and feel and can cause severe emotional symptoms and even thoughts that life isn’t worth living anymore.
Major depression can affect not only the emotional aspect of one’s life but the physical as well. Patients may stop caring for their hygiene, experience insomnia or sleep too much, overeat or barely eat leading to weight loss or gain.
Nursing Process
Nurses will encounter patients with depression that may be exacerbated by other chronic health conditions. Chronic pain and debilitating physical illnesses often lead to depression. Major depression requires the diagnosis and treatment of trained mental health providers, but nurses are important in offering a therapeutic relationship that allows patients to express their thoughts and feelings while supporting them holistically and maintaining their safety.
Nursing Assessment
Nurses should conduct a thorough assessment of patients with Major Depression to identify symptoms and their severity. This includes evaluating the patient’s emotional state, cognitive function, and physical health. The assessment should cover:
- Psychological symptoms such as persistent sadness, loss of interest, and feelings of hopelessness.
- Somatic complaints including changes in appetite, sleep disturbances, and fatigue.
- Cognitive symptoms like poor concentration and indecisiveness.

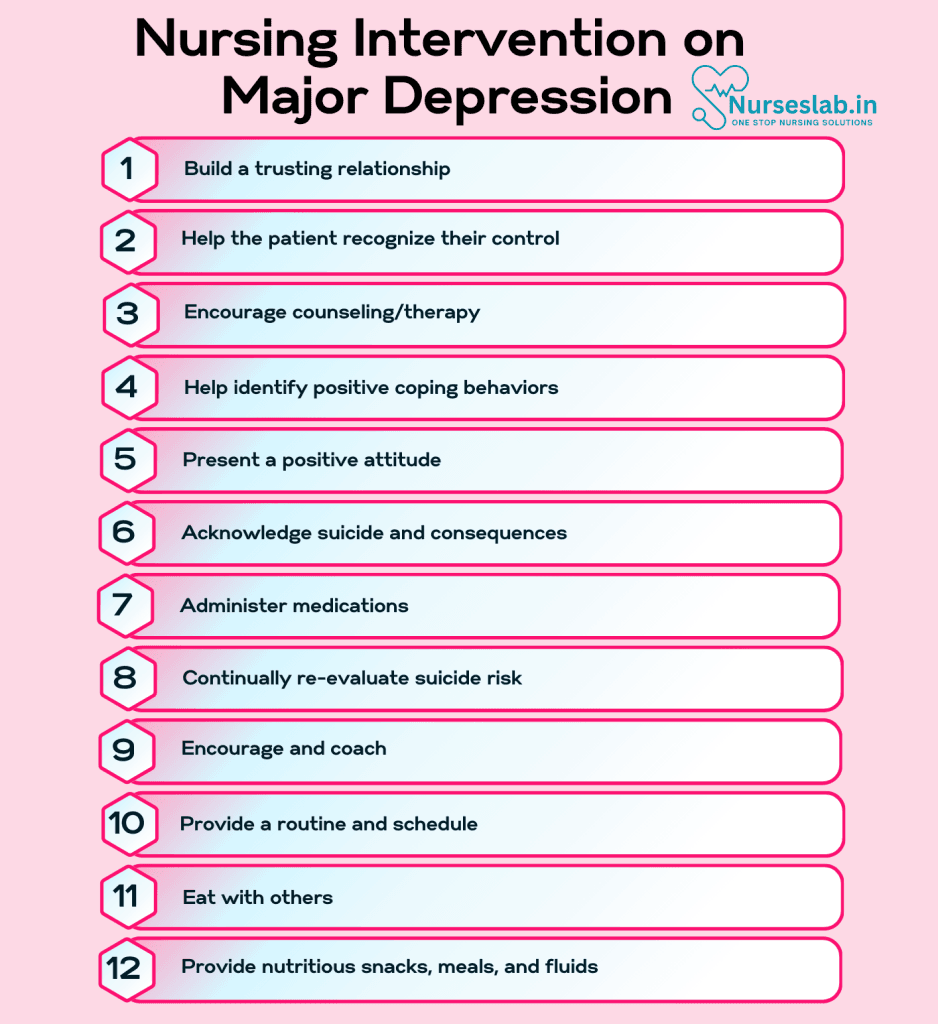
Nursing Intervention
Major Depression, also known as Major Depressive Disorder (MDD), is a serious mental health condition characterized by persistent feelings of sadness, hopelessness, and a lack of interest or pleasure in almost all activities. It can significantly impair a person’s ability to function in daily life. Nursing interventions play a crucial role in the management and treatment of Major Depression. The following are key nursing interventions for managing Major Depression:
Nursing Care Plans
Once the nurse identifies nursing diagnoses for major depression, nursing care plans help prioritize assessments and interventions for both short and long-term goals of care. In the following section, you will find nursing care plan examples for major depression.
Hopelessness
A patient with major depression may feel no sense of purpose and no way out of their pessimistic state of mind.
Nursing Diagnosis: Hopelessness
Related to:
- Social Isolation
- Long-term stress
- Loss of spiritual beliefs
- Depressed cognitive functions (thinking, decision making)
As evidenced by:
- Verbalized belief that nothing can be changed and no reason to do so
- Passivity
- No response to positive or negative stimuli
- Decreased affect
- Lack of initiative
- Loss of interest in life
- Increased or decreased sleep
- Sighing, not making eye contact, no verbalization
- Substance abuse
- Self-harm
- Suicidal ideation
Expected Outcomes:
- Patient will verbalize their feelings regarding hopelessness
- Patient will identify coping mechanisms to improve feelings of hopelessness
- Patient will set short and long-term goals to develop and maintain a positive outlook
Assessment:
1. Assess additional causes beyond depression.
Depression compounded by job loss, relationship strains, legal concerns, financial stress, and other chronic health conditions can worsen hopelessness and may require their own specific interventions.
2. Assess for negative coping mechanisms.
These can include increasing sleep, drug use, risky sexual behaviors, avoiding responsibility, self-sabotaging progress, and self-harm.
3. Determine spiritual beliefs.
Determine if the patient has a strong sense of spirituality and if it has recently changed or become a source of hopelessness. Religious beliefs can be a source of hope but also cause added stress and inadvertently harm the patient’s mental health.
Interventions:
1. Build a trusting relationship.
A trusting, supportive rapport will allow the patient a safe space to address their thoughts and feelings.
2. Help the patient recognize their control.
The patient may have a skewed understanding of what is or isn’t in their control. Help the patient recognize misconceptions and accept only what is within their ability to change.
3. Encourage counseling/therapy.
Major depression requires the interventions of a trained mental health professional. Psychologists can help with acceptance and adaption to life changes, help set realistic goals, and help develop skills to cope.
4. Help identify positive coping behaviors.
Assist the patient in identifying coping behaviors they have used in the past that were effective or activities they once enjoyed that can help now. Examples include journaling, music, dance, sports, traveling, spending time outside, or playing with a pet.
Risk For Suicide
Patients with major depression that is not controlled may experience greater feelings of hopelessness which is associated with suicidal thoughts.
Nursing Diagnosis: Risk for Suicide
Related to:
- Feelings of hopelessness
- History of previous suicide attempt
- Stockpiling medications
- Giving away possessions
- Sudden euphoric recovery from major depression
- A change in behavior or attitude
- Threats to kill oneself or a desire to die
- Living alone or lack of a support system
Note: A risk diagnosis is not evidenced by signs and symptoms as the problem has not yet occurred and the goal of nursing interventions is aimed at prevention.
Expected Outcomes:
- Patient will remain safe from suicide or self-injury
- Patient will identify factors contributing to thoughts of suicide
- Patient will participate in therapy sessions and willingly attempt to change depression symptoms
Assessment:
1. Assess for a suicide plan.
A patient should be directly asked if they want to kill themself and if they have a specific plan to do so to determine intent.
2. Note the use of drugs or alcohol.
Assess if a patient is using drugs or alcohol or abusing prescribed medications. Easy access to pain medication, benzodiazepines, and anti-depressants can be dangerous for a suicidal patient.
Interventions:
1. Present a positive attitude.
Structure statements and actions in a positive “can do” way instead of “do not.” An example is “You can go for a walk today” or “You get to see your family tomorrow.”
2. Acknowledge suicide and consequences.
The nurse can acknowledge suicide as an option while also discussing the reality of that option and its consequences. Inquire about how suicide will solve the patient’s problems and offer alternatives.
3. Administer medications.
Medications such as anti-depressants, benzodiazepines, and antipsychotics should be given in a controlled and monitored setting.
4. Promote safety.
If on an inpatient behavioral health unit, the patient may require 1:1 supervision to ensure safety. Items that could be used to harm themselves such as clothing items, cords, and sharp objects should be removed.
5. Continually re-evaluate suicide risk.
Especially after mood changes and at discharge as a patient who is feeling better is at the highest risk for suicide because they may now have the energy to carry out their suicide.
Self-Care Deficit
Major depression can affect the patient’s motivation and energy in completing self-care tasks.
Nursing Diagnosis: Self-Care Deficit
Related to:
- Lack of motivation
- Lack of energy
- Loss of interest
- Insomnia or oversleeping
- Preoccupation with thoughts
- Anxiety
- Severe fatigue
As evidenced by:
- Altered sleep schedules (sleeping very late or not enough)
- Poor appearance, body odor, disheveled clothing
- Weight loss from eating inconsistently
- Cluttered or messy living environment
Expected Outcomes:
- Patient will bathe at least every other day and dress in clean clothing daily
- Patient will drink at least 5 glasses of water and eat 2-3 nutritious meals daily
- Patient will improve sleep habits by instituting a set bedtime and wake time
Assessment:
1. Assess barriers to self-care.
Depression itself is a barrier but the nurse can delve further into the causes of the patient’s poor self-care. The patient may lack the energy, time, assistance, or may feel the tasks are unimportant.
2. Assess for a support system.
The patient may not necessarily need physical help with tasks, though that should be assessed as well. A support person can mentally and emotionally encourage the depressed patient to participate in their self-care.
3. Assess medication regimen.
The depressed patient likely takes anti-depressants as well as anti-anxiety and sleep aids. These all have relaxing effects and increase drowsiness. Assess how the patient is taking these medications to ensure they are not over-using.
Interventions:
1. Encourage and coach.
A patient with depression has a slower, clouded thought process and difficulty concentrating. They may need step-by-step guidance to complete even simple tasks.
2. Provide a routine and schedule.
Setting a specific sleep/wake schedule and routine for eating, grooming, and dressing can help motivate the patient.
3. Eat with others.
Encourage the patient to eat with family and friends or other patients if applicable to increase socialization.
4. Provide nutritious snacks, meals, and fluids.
The patient with depression may lack an appetite and the energy to prepare meals. Ensure the patient is drinking plenty of water and provide nutritious snacks such as fruit, nut butters, yogurt, or granola that are easily accessible with minimal preparation.
Nursing Diagnoses and Rationales
1. Ineffective Coping
Rationale: Patients with Major Depression often struggle with ineffective coping mechanisms, leading to increased stress, anxiety, and feelings of hopelessness. Providing education on healthy coping strategies, such as cognitive-behavioral techniques and stress management, can help patients develop resilience and improve their mental health.
2. Disturbed Sleep Pattern
Rationale: Insomnia or hypersomnia is a common symptom of Major Depression. Poor sleep can exacerbate depressive symptoms and negatively impact overall well-being. Nurses can educate patients on sleep hygiene practices and collaborate with healthcare providers to manage sleep disturbances effectively.
3. Imbalanced Nutrition: Less Than Body Requirements
Rationale: Major Depression can lead to appetite changes and poor nutrition, resulting in weight loss and nutritional deficiencies. Nurses can assess nutritional status, provide dietary recommendations, and refer patients to dietitians for further support.
4. Risk for Suicide
Rationale: Patients with Major Depression are at an increased risk of suicidal ideation and behavior. Nurses must conduct thorough risk assessments, provide a safe environment, and implement crisis intervention strategies to ensure patient safety.
5. Social Isolation
Rationale: Depressive symptoms often lead to withdrawal from social interactions, resulting in social isolation and loneliness. Nurses can encourage patients to engage in social activities, connect with support groups, and foster supportive relationships.
6. Self-Care Deficit
Rationale: Major Depression can impair the ability to perform daily self-care activities, such as personal hygiene, grooming, and household tasks. Nurses can assist patients in developing a structured routine, setting achievable goals, and providing practical support to enhance self-care abilities.
REFERENCES
- Depression (major depressive disorder) – Symptoms and causes. (2018, February 3). Mayo Clinic. Retrieved March 17, 2022, from https://www.mayoclinic.org/diseases-conditions/depression/symptoms-causes/syc-20356007
- Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2008). Nurse’s Pocket Guide Diagnoses, Prioritized Interventions, and Rationales (11th ed.). F. A. Davis Company.
- Mufson, L., Bufka, L., & Wright, C. V. (2016, October 1). Overcoming depression: How psychologists help with depressive disorders. American Psychological Association. Retrieved March 17, 2022, from https://www.apa.org/topics/depression/overcoming
- Smith, M., Robinson, L., & Segal, J. (2021, October). Coping with Depression. HelpGuide.org. Retrieved March 17, 2022, from https://www.helpguide.org/articles/depression/coping-with-depression.htm
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.







