Chronic hives, or chronic idiopathic urticaria, involve recurring itchy welts lasting more than six weeks with no identifiable trigger. Understanding symptoms, causes, diagnosis, and management is essential for patient education, nursing care, and clinical practice.
Introduction: What Are Chronic Hives?
Chronic hives, medically known as chronic urticaria, is a skin condition characterised by the recurrent appearance of itchy, raised welts or bumps on the skin. These welts, commonly referred to as hives, can vary in size, shape, and location, often appearing and disappearing unpredictably. Unlike acute hives, which typically resolve within hours or days, chronic hives persist for six weeks or longer, sometimes lasting for months or even years.
Chronic urticaria affects people of all ages, though it is more commonly seen in adults, with women being slightly more affected than men. The unpredictable nature of hives, their physical discomfort, and the impact on daily life make this condition a significant concern for patients, families, and healthcare providers alike.
Causes and Risk Factors
Common Triggers
The exact cause of chronic hives often remains elusive, leading to frustration for patients and caregivers. In many cases, no specific trigger can be identified. However, several factors and conditions have been associated with the development or worsening of chronic urticaria:
- Allergic Reactions: While allergies are a common cause of acute hives, they rarely explain chronic cases. However, certain foods, medications (such as antibiotics or painkillers), insect stings, or contact with chemicals may occasionally trigger chronic hives.
- Physical Factors: Some individuals experience hives due to physical stimuli, such as pressure, heat, cold, sunlight (solar urticaria), or water (aquagenic urticaria).
- Stress: Emotional stress and anxiety have been recognised as aggravating factors, potentially triggering or worsening outbreaks.
- Infections: Viral, bacterial, or parasitic infections can sometimes precede or accompany chronic hives, especially in children.
- Autoimmune Reactions: In a significant proportion of cases, chronic hives are linked to the immune system mistakenly attacking healthy tissues, leading to the release of histamine and other chemicals that cause hives.
Underlying Conditions
Chronic urticaria may sometimes be associated with other medical conditions, such as:
- Thyroid disorders (particularly autoimmune thyroid disease)
- Lupus or other autoimmune diseases
- Chronic infections
- Hormonal changes, such as those occurring during pregnancy or menopause
It is important for healthcare providers to consider these possibilities during evaluation, as treating the underlying condition may help manage hives.
Genetic and Environmental Factors
While chronic hives are not typically inherited, some people may have a genetic predisposition to allergic or autoimmune conditions. Environmental factors such as pollution, climate, and exposure to certain chemicals may also play a role in triggering or exacerbating the condition.
Symptoms of Chronic Hives
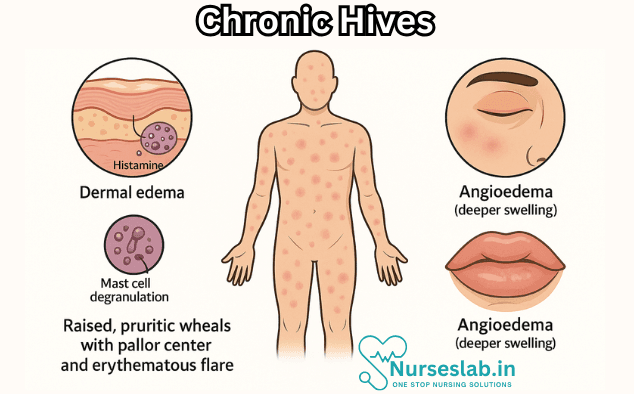
The primary symptom of chronic urticaria is the appearance of hives—raised, red or skin-coloured welts that can be itchy, painful, or cause a burning sensation. These welts may vary in size, ranging from a few millimetres to several centimetres, and often change shape or location within hours.
Physical Manifestations
- Itching and discomfort: The most common and distressing symptom is intense itching, which can interfere with sleep and daily activities.
- Swelling: Sometimes, deeper swelling occurs, known as angioedema, which affects the lips, eyelids, throat, or limbs and can be more serious.
- Colour and shape: Hives may be red, pink, or skin-toned, often surrounded by a pale halo. They can appear as individual bumps or merge into larger patches.
- Pattern and duration: Lesions typically last less than 24 hours in one spot but new ones can appear elsewhere, leading to a persistent course.
Severity and Patterns
The severity of symptoms varies greatly between individuals. Some may experience mild, intermittent itching, while others suffer from extensive, persistent hives and swelling. The unpredictable nature of outbreaks makes chronic hives particularly challenging to manage.
Diagnosis of Chronic Hives
Medical Evaluation
Diagnosing chronic urticaria involves a thorough medical history and physical examination. Healthcare providers will ask about the onset, duration, frequency, and characteristics of the hives, as well as any potential triggers, associated symptoms, and underlying health conditions.
Tests and Investigations
There is no single test that can definitively diagnose chronic hives. However, certain investigations may be recommended to rule out underlying causes or related conditions:
- Blood tests to check for thyroid function, autoimmune markers, infection, or inflammation
- Allergy testing, although rarely useful for chronic cases, may be considered if food or drug allergy is suspected
- Skin biopsy, in rare cases, to exclude other skin diseases
Differential Diagnosis
Doctors must distinguish chronic hives from other conditions that cause similar symptoms, such as eczema, psoriasis, insect bites, or vasculitis. A careful evaluation ensures appropriate management and avoids unnecessary treatments.
Treatment Options for Chronic Hives
Medications
The primary goal of treatment is to control symptoms, improve quality of life, and minimise recurrences. Common medications include:
- Antihistamines: Non-sedating antihistamines are the first-line treatment, helping to block the action of histamine and reduce itching.
- Higher-dose antihistamines: If standard doses are ineffective, doctors may recommend higher doses under supervision.
- Corticosteroids: Short courses of oral steroids may be used for severe flare-ups, but long-term use is avoided due to side effects.
- Leukotriene antagonists: These medications may help some patients, particularly those with associated asthma or allergies.
- Immunomodulatory drugs: In resistant cases, drugs that modify the immune system, such as cyclosporine or omalizumab (an injectable antibody), may be prescribed.
Lifestyle Changes
Non-medication approaches are important for all patients and may reduce the frequency or severity of outbreaks:
- Avoiding known triggers, such as certain foods, medications, or environmental factors
- Wearing loose, comfortable clothing to reduce irritation
- Using mild, fragrance-free soaps and moisturisers
- Keeping cool and avoiding excessive heat or sweating
- Managing stress through relaxation techniques, yoga, or meditation
Alternative Therapies
Some patients seek relief through complementary therapies, such as Ayurveda, homoeopathy, acupuncture, or herbal remedies. While scientific evidence is limited, these approaches may provide comfort or support when used alongside conventional treatments. It is important to consult a qualified healthcare professional before starting alternative therapies.
Management Strategies: Living with Chronic Hives
Coping Mechanisms
Chronic hives can be emotionally and physically taxing. Developing coping strategies is vital for maintaining well-being:
- Keeping a symptom diary to track triggers and patterns
- Educating oneself about the condition to reduce anxiety and uncertainty
- Seeking support from family, friends, or patient groups
- Maintaining regular follow-up with a dermatologist or allergist
- Practising mindfulness and stress reduction
Prevention
While it may not be possible to completely prevent chronic hives, certain steps can minimise outbreaks:
- Avoiding known or suspected triggers
- Taking prescribed medications regularly
- Maintaining a healthy lifestyle, including balanced nutrition, adequate sleep, and regular exercise
- Protecting the skin from irritants, extremes of temperature, and trauma
Patient Education
Empowering patients with accurate information about chronic hives is crucial. Understanding the nature of the condition, realistic treatment goals, and available resources can help patients navigate their journey with confidence.
Impact on Quality of Life
Emotional Effects
Chronic urticaria often has a profound impact on mental health. Persistent itching, discomfort, and visible skin changes may lead to anxiety, depression, embarrassment, or social withdrawal. Patients may feel frustrated by the unpredictable nature of the condition and the lack of a clear cure.
Social and Occupational Effects
The visible appearance of hives and the need for frequent medical appointments can affect relationships, work performance, and participation in social activities. Some patients may avoid public places or professional settings due to self-consciousness or fear of flare-ups.
Nursing Care of Patients with Chronic Hives (Chronic Idiopathic Urticaria)
The term “idiopathic” refers to the unknown cause of the condition, which makes targeted treatment difficult and necessitates a holistic and patient-centered approach from nurses.
Nursing Assessment
A thorough nursing assessment forms the foundation of effective care.
- History Taking: Document onset, duration, frequency, and distribution of hives and any associated angioedema. Explore possible triggers, including medications, food, environment, stress, and infections. Record previous management efforts and their efficacy.
- Physical Examination: Inspect for active hives, noting size, color, and pattern. Assess for signs of angioedema, including airway involvement (stridor, difficulty speaking/swallowing), which should prompt immediate medical intervention.
- Impact on Daily Life: Investigate how symptoms affect sleep, work, social interactions, and emotional health.
- Medication Review: Identify current and past medications, including over-the-counter antihistamines, steroids, or alternative therapies.
- Risk Evaluation: Evaluate for signs of anaphylaxis or severe allergic responses, even though CIU rarely leads to life-threatening reactions.
Planning and Implementation of Nursing Care
Nursing care for CIU focuses on symptom management, patient education, and psychological support.
Symptom Management
Medication Administration:
- Administer prescribed non-sedating antihistamines (e.g., cetirizine, loratadine) as first-line therapy.
- Monitor for side effects and effectiveness; titrate dose per physician’s orders.
- In refractory cases, additional medications may be required (e.g., montelukast, omalizumab, cyclosporine), with vigilance around adverse effects.
- Educate patients on the importance of medication adherence despite fluctuations in symptom severity.
Skin Care:
- Advise gentle cleansing and avoidance of irritants (fragrances, strong soaps, hot water).
- Recommend emollients to soothe dry, itchy skin.
- Discourage scratching, as it can worsen lesions and increase infection risk.
Itch Relief Strategies:
- Suggest cool compresses and loose, comfortable clothing.
- Teach relaxation techniques to reduce perception of itch.
Angioedema Monitoring:
- Observe for any progression to swelling of the airway; initiate emergency protocols if respiratory compromise is suspected.
- Provide reassurance and rapid access to emergency medications (e.g., epinephrine) if indicated.
Patient Education
Empowering patients through education is crucial for self-management and reducing anxiety.
- Condition Information: Explain the nature of CIU, emphasizing that it is not contagious and often lacks a clear trigger.
- Trigger Avoidance: Help patients identify and avoid known aggravators, even though most cases are idiopathic. Keep a symptom diary to track possible patterns.
- Medication Education: Review the proper use, timing, and potential side effects of prescribed drugs. Stress the importance of adhering to treatment even in periods of remission.
- When to Seek Help: Clearly outline symptoms of severe reactions (breathing difficulty, widespread swelling) that require urgent medical attention.
- Lifestyle Adjustments: Encourage stress management, balanced nutrition, and regular exercise to support overall health.
- Coping Strategies: Discuss ways to manage itch and discomfort during flare-ups.
Psychosocial Support and Advocacy
Living with CIU can be frustrating and emotionally taxing. Nurses play an essential role in providing emotional support and connecting patients to appropriate resources.
- Empathetic Listening: Offer a safe space for patients to express concerns and frustrations about the unpredictability of their condition.
- Support Groups: Encourage participation in support groups, either locally or online, where individuals can share advice and experiences.
- Referral to Mental Health Services: Identify signs of anxiety, depression, or social isolation and refer to counseling if needed.
- Education for Family and Caregivers: Provide family members with information about CIU so they can support the patient effectively.
Monitoring and Follow-Up
Continuous monitoring is essential for assessing response to therapy and detecting complications.
- Schedule regular follow-ups to review symptoms, medication effects, and quality of life.
- Document changes in the pattern, severity, or frequency of hives and angioedema.
- Monitor for adverse drug reactions or complications of long-term medication use.
- Maintain open communication with the healthcare team to adjust the care plan as needed.
Special Considerations in Nursing Care
Pediatric Patients
- Adapt educational materials and approaches for age and cognitive level.
- Support families in coping with the stress of a chronic condition and in advocating for their child at school and social settings.
Older Adults
- Monitor for polypharmacy and increased vulnerability to medication side effects.
- Assess for skin fragility and increased risk of secondary infection.
Pregnancy and Lactation
- Coordinate care with the healthcare provider to ensure the safety of medications during pregnancy and breastfeeding.
- Monitor for hormonal changes that may influence symptom severity.
Documentation
Accurate and thorough documentation is vital for continuity of care.
- Record assessment findings, interventions, patient education, and response to therapy.
- Use standardized tools to track symptom severity and functional status.
- Document patient concerns and psychosocial needs.
Common Nursing Diagnoses in CIU
- Ineffective Skin Integrity related to the presence of hives and scratching
- Impaired Comfort due to pruritus and swelling
- Risk for Anxiety connected to unpredictability of symptoms and impact on social life
- Deficient Knowledge regarding chronic urticaria and its management
- Disturbed Sleep Pattern related to nocturnal itching
REFERENCES
- American Academy of Dermatology. 10 Ways to Get Relief from Chronic Hives. https://www.aad.org/public/diseases/a-z/hives-chronic-relief.
- Hives (urticaria). American College of Allergy, Asthma, and Immunology. http://acaai.org/allergies/types/skin-allergies/hives-urticaria.
- Bracken SJ Abraham S, MacLeod AS. Autoimmune theories of chronic spontaneous urticaria. https://pubmed.ncbi.nlm.nih.gov/30984191/. Front Immunol. 2019 March 29;10:627.
- Chen Y, Wu C, Shen J, Chen T, Chang Y. Cancer risk in patients with chronic urticaria: A population-based cohort study. https://jamanetwork.com/journals/jamadermatology/fullarticle/1105196. Arch Dermatol. 2012;148(1):103–108.
- Hives (urticaria). American College of Allergy, Asthma, and Immunology. http://acaai.org/allergies/types/skin-allergies/hives-urticaria.
- Khan S. Urticaria in patients with diabetes: Adverse drug reaction or relapse of underlying autoimmune urticaria?. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6607826/ Indian J Med Res. 2019;149(3):423-425.
- Merck Manual (Consumer Version). Hives. https://www.merckmanuals.com/home/skin-disorders/itching-and-dermatitis/hive.
- Kelly AP, et al., eds. Drug eruptions. In: Taylor and Kelly’s Dermatology for Skin of Color. 2nd ed. McGraw Hill; 2016. https://accessmedicine.mhmedical.com.
- Sachdeva S, Gupta V, Amin SS, Tahseen M. Chronic urticaria. Indian J Dermatol. 2011;56(6):622-628.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





