Kidney donation stands as one of the most profound acts of altruism, offering a chance at renewed life for thousands suffering from chronic kidney disease or end-stage renal failure. This document explores the multifaceted world of kidney donation—from its medical underpinnings and ethical considerations to the transformative impact it has on both donors and recipients.
Introduction to Kidney Donation
Kidneys are vital organs, responsible for filtering waste products from the blood, regulating fluid balance, and maintaining essential electrolyte levels. When kidneys fail, toxins accumulate, and the body loses its equilibrium, leading to life-threatening complications. For those facing irreversible kidney failure, transplantation becomes a beacon of hope, offering improved quality and length of life compared to lifelong dialysis.
Kidney donation can be categorised in two main ways: living donation and deceased donation. Both paths involve generous acts of giving, but their processes and implications differ.
The Need for Kidney Donation
Globally, millions are affected by kidney disease. According to the World Health Organization, chronic kidney disease ranks among the top causes of mortality, and the prevalence continues to rise due to factors such as diabetes, hypertension, and aging populations. Dialysis, while lifesaving, is not a cure—it is a demanding regimen that can restrict lifestyle and carries significant physical, emotional, and financial burden.
Transplantation offers the best chance for long-term survival and improved well-being. However, a stark shortage of donor kidneys persists, leaving countless patients on waiting lists for years. The gap between supply and demand underscores the critical importance of kidney donation.
Types of Kidney Donation
Living Donation
Living kidney donation involves a healthy individual voluntarily giving one of their two kidneys to someone in need—often a family member, friend, or, in rare cases, a stranger. Since humans can generally live healthy lives with a single kidney, living donation is a viable and increasingly common option.
Benefits of Living Donation:
- Shorter waiting times for recipients
- Better long-term outcomes compared to deceased donor kidneys
- Transplants can be scheduled, allowing for medical optimisation
- Immediate functioning of the transplant in most cases
Risks and Considerations:
- Surgical risks, such as infection, bleeding, or rare complications
- Potential effects on remaining kidney function over time
- Emotional impact and psychological adjustment for the donor
Living donation is highly regulated, ensuring the donor’s health and well-being remain paramount throughout the process.
Deceased Donation
Deceased kidney donation occurs when an individual, typically after brain death, has consented (or their family consents) to organ donation. After the donor has passed away, medical teams assess and retrieve organs, which are then matched and transplanted into recipients.
Benefits of Deceased Donation:
- Opportunity to save multiple lives through organ and tissue donation
- Expands the donor pool to those who are not living donors
- Often the only option for patients without compatible living donors
Challenges:
- Limited availability due to criteria for suitable donors
- Potential delays in organ retrieval and transplant
- Variable organ quality depending on donor health and cause of death
The Kidney Donation Process
Evaluation
Whether living or deceased, all potential donors undergo extensive medical evaluation to ensure suitability and safety. Living donors are assessed for physical health, kidney function, psychological readiness, and compatibility with recipients. Deceased donors are evaluated for infectious diseases, organ viability, and matching criteria.
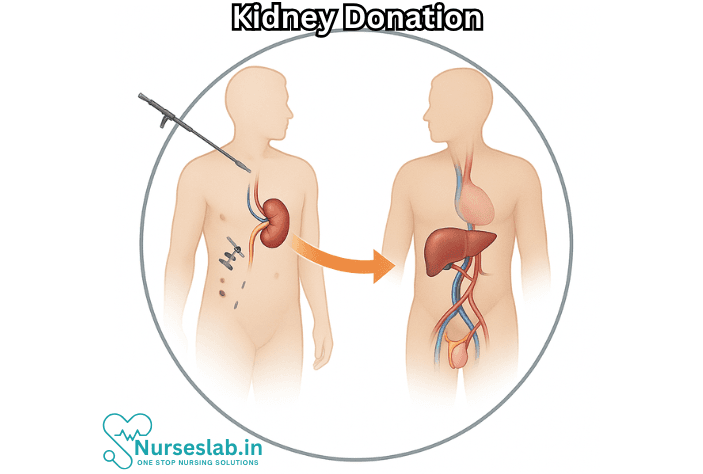
Surgical Procedure
For living donors, kidney removal is typically performed laparoscopically, minimising recovery time and scarring. The recipient’s surgery involves connecting the donated kidney to their blood vessels and urinary tract. The procedure lasts several hours, followed by a hospital stay for both donor and recipient.
Deceased donor kidneys are retrieved in sterile conditions and preserved before transplantation. Modern techniques and rapid transportation have increased success rates and reduced waiting times.
Recovery and Follow-Up
Living donors generally recover within weeks, resuming normal activities with minimal long-term impact. Lifelong monitoring is recommended to ensure ongoing kidney health. Recipients require immunosuppressive medication to prevent rejection and regular follow-up to monitor function and detect complications.
Ethical and Legal Considerations
Kidney donation navigates complex ethical terrain. Informed consent is essential, ensuring donors understand risks, benefits, and alternatives. Coercion, financial incentives, and organ trafficking are strictly prohibited and monitored by international guidelines and national legislation.
Deceased donation relies on clear consent—either through registration, donor cards, or family discussions. Many countries invest in awareness campaigns and legal frameworks to encourage organ donation and protect all parties involved.
Impact on Donors and Recipients
Donors
Living donors describe a profound sense of satisfaction and fulfillment, knowing they’ve changed or saved a life. Some face emotional challenges, such as anxiety or adjustment to their new physical state. Support systems, counseling, and peer networks help donors navigate these complexities.
Recipients
For recipients, a successful transplant means freedom from dialysis, restoration of energy, and renewed hope for the future. Quality of life improves dramatically, and many return to work, family life, and personal pursuits. However, ongoing challenges remain—medication side effects, risk of rejection, and the psychological journey of living with a transplanted organ.
Barriers and Solutions
Despite the life-changing potential, barriers to kidney donation persist. Misinformation, cultural taboos, lack of awareness, and fear of medical procedures deter potential donors. Health inequities mean that some communities have less access to transplantation services.
To overcome these obstacles, education campaigns, policy initiatives, and community outreach play pivotal roles. Sharing donor and recipient stories, clarifying misconceptions, and highlighting the safety and impact of donation foster greater willingness to participate.
Innovations in Kidney Donation
Medical advances continue to revolutionise kidney transplantation. Paired kidney exchanges allow incompatible donor-recipient pairs to swap kidneys with others, increasing the chance of suitable matches. Research into artificial kidneys, xenotransplantation (animal to human), and regenerative medicine holds promise for future solutions.
International collaborations, improved organ tracking, and advances in immunosuppression have all contributed to higher success rates and better patient outcomes.
How to Become a Donor
Anyone interested in becoming a kidney donor should start by consulting healthcare professionals and learning about local regulations. Living donation requires comprehensive medical screening and counseling. Deceased donation can be arranged by registering with national organ donor registries or discussing wishes with family.
Simple steps to start:
- Reach out to transplant centers or advocacy groups for supportstyle after donation. This positively impacts their overall health.
- Inform yourself about risks, benefits, and the donation process
- Talk to your family about your decision
- Register as an organ donor if possible
Nursing Care of Patients with Kidney Donation: A Gift of Life
Nursing care plays a pivotal role throughout this journey, from preoperative assessment and education to postoperative recovery and long-term well-being. This document explores the multifaceted responsibilities and compassionate interventions nurses provide to patients involved in kidney donation.
Preoperative Nursing Care
Before surgery, the nurse’s role centers on assessment, education, and preparation—both physically and emotionally.
Assessment and Screening
- Comprehensive Health Evaluation: Nurses assist in gathering the donor’s medical history, conducting physical assessments, and coordinating laboratory and diagnostic tests.
- Psychosocial Screening: Evaluation of mental health and social circumstances is critical to ensure donors are emotionally prepared and supported.
Patient Education
- Procedure Explanation: Nurses provide clear information about the surgical process, potential risks, and expected outcomes.
- Postoperative Expectations: Education includes anticipated pain, mobility limitations, wound care, and possible complications.
- Lifestyle Adjustments: Guidance on post-donation lifestyle, diet, exercise, and follow-up care helps donors make informed choices.
Emotional Support
- Active Listening: Nurses encourage donors to express fears, doubts, and expectations, fostering trust and emotional safety.
- Family Involvement: Providing education and support to the donor’s family helps create a holistic support network.
Perioperative Nursing Care
During the surgical period, nurses work alongside the medical team to ensure donor safety, comfort, and dignity.
Preoperative Preparation
- Physical Preparation: Ensures the patient is ready for anesthesia and surgery, including fasting, hygiene, and medication review.
- IV Access and Monitoring: Establishing intravenous lines, monitoring vital signs, and assessing baseline data.
- Psychological Preparation: Calm reassurance and distraction techniques help to reduce anxiety before entering the operating theater.
Intraoperative Support
- Patient Advocacy: Nurses act as patient advocates, ensuring the donor’s concerns and needs are communicated to the surgical team.
- Sterile Technique and Safety: Maintaining a sterile environment and monitoring for any emergent complications.
Immediate Postoperative Care
- Observation: Close monitoring of vital signs, pain, fluid balance, and wound condition.
- Pain Management: Administration of prescribed analgesics, assessment of pain levels, and use of non-pharmacological comfort measures.
- Prevention of Complications: Monitoring for signs of infection, bleeding, deep vein thrombosis, and pulmonary issues.
- Early Mobilization: Encouraging gentle movement and exercises to prevent complications such as blood clots and pneumonia.
Postoperative Nursing Care
Recovery after kidney donation encompasses physical healing, emotional adjustment, and education for long-term health.
Physical Recovery
- Wound Care: Nurses teach and assist with proper wound cleaning, dressing changes, and infection recognition.
- Fluid and Electrolyte Balance: Monitoring urine output, hydration status, and electrolyte levels as the single remaining kidney adapts.
- Medication Management: Providing instructions on any new or continued medications, and observing for side effects.
- Activity Guidelines: Graduated increases in physical activity are encouraged, avoiding heavy lifting and strenuous exercise for several weeks.
- Nutrition: Guidance on a balanced diet with adequate protein, vitamins, and minerals to support healing and kidney function.
Psychosocial Recovery
- Support Groups: Nurses can connect donors with peer support groups, reducing feelings of isolation and fostering shared experiences.
- Counseling: Referral to mental health professionals for donors needing assistance coping with body image, identity changes, or anxiety.
- Adjustment and Acceptance: Nurses help donors adapt to changes, celebrate milestones, and recognize the significance of their gift.
Follow-Up Care
- Regular Checkups: Scheduled follow-up visits to monitor kidney function, blood pressure, and overall health.
- Long-Term Health Maintenance: Ongoing education about the signs of kidney-related problems and when to seek medical help.
- Lifestyle Support: Continued encouragement for healthy living: avoiding smoking, moderating alcohol, and maintaining an active lifestyle.
Special Considerations in Nursing Care
Kidney donors are unique patients whose care requires sensitivity and tailored approaches.
- Individualized Plans: Nurses develop personalized care plans based on the donor’s physical, emotional, and social needs.
- Cultural Competence: Respecting cultural beliefs and practices around donation and organ loss.
- Ethical Support: Navigating the complexities of autonomy, informed consent, and donor rights with compassion and respect.
Potential Risks and Complications
While kidney donation is generally safe for most healthy adults, nursing vigilance is essential to detect and address potential complications.
- Surgical Risks: Infection, bleeding, blood clots, or reactions to anesthesia.
- Long-Term Risks: Slightly increased risk of high blood pressure or reduced kidney function in rare cases.
- Psychological Impact: Donors may experience regret, anxiety, or depression, underscoring the need for ongoing support.
Promoting the Donor’s Legacy
Nurses play a significant role in honoring and affirming the donor’s decision, celebrating their altruism, and supporting their lifelong health journey.
- Celebrating the Gift: Recognizing the donor’s contribution to another person’s life and sharing positive stories of recovery and hope.
- Educational Initiatives: Nurses may participate in community education, encouraging awareness and respect for organ donation.
- Advocacy: Nurses advocate for donor health rights, psychosocial support, and access to quality medical care.
REFERENCES
- Ghelichi-Ghojogh M, Ghaem H, Mohammadizadeh F, et al. Graft and Patient Survival Rates in Kidney Transplantation, and Their Associated Factors: A Systematic Review and Meta-Analysis https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8643514/. Iran J Public Health. 2021 Aug;50(8):1555-1563.
- Merck Manual Consumer Version. Kidney Transplantation https://www.merckmanuals.com/home/immune-disorders/transplantation/kidney-transplantation. Last reviewed 8/2022.
- Grams ME, et al. Kidney-failure risk projection for the living kidney-donor candidate. The New England Journal of Medicine. 2016; doi:10.1056/NEJMoa1510491.
- National Health Service (U.K.). Kidney Transplant (https://www.nhs.uk/conditions/kidney-transplant/).
- National Institute on Aging (U.S.). Frequently Asked Questions about Organ Donation for Older Adults https://www.nia.nih.gov/health/frequently-asked-questions-about-organ-donation-older-adults. Last reviewed 2/28/2022.
- National Institute of Diabetes and Digestive and Kidney Diseases (U.S.). Solitary or Single-Functioning Kidney https://www.niddk.nih.gov/health-information/kidney-disease/solitary-kidney. Last reviewed 10/2020.
- National Kidney Foundation (U.S.). Multiple pages reviewed for this article (https://www.kidney.org/).
- Yu ASL, et al., eds. Considerations in living kidney donation. In: Brenner & Rector’s The Kidney. 11th ed. Elsevier; 2020. https://www.clinicalkey.com.
- National Kidney Registry (U.S.). Does Donating a Kidney Shorter Your Life (https://www.kidneyregistry.org/for-donors/kidney-donation-blog/does-donating-a-kidney-shorten-your-life/)? Updated 3/7/2023. 7/11/2024.
- National Library of Medicine (U.S.). Kidney Removal. https://medlineplus.gov/ency/article/003001.htm). Reviewed 1/1/2023.
- Lentine KL, et al. Risks of living kidney donation: Current state of knowledge on outcomes important to donors. Clinical Journal of the American Society of Nephrology. 2019; doi:10.2215/CJN.11220918.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





