Introduction
Laser lithotripsy represents a significant advancement in the treatment of urinary tract stones, particularly those found in the kidneys and ureters. As a minimally invasive procedure, it harnesses the precision and energy of laser technology to fragment stones that would otherwise require surgical intervention. Over the past few decades, laser lithotripsy has become a cornerstone of urological practice, offering patients a safer, more effective alternative to traditional surgical approaches.
What is Laser Lithotripsy?
Laser lithotripsy is a medical procedure that uses concentrated laser energy to break up stones within the urinary tract. The word “lithotripsy” originates from the Greek words “lithos,” meaning stone, and “tripsis,” meaning crushing. Unlike extracorporeal shock wave lithotripsy (ESWL), which uses external shock waves, laser lithotripsy delivers energy directly to the stone via a fiber-optic cable, typically during a procedure called ureteroscopy.
Types of Stones Treated
Laser lithotripsy is most commonly used to treat:
- Kidney stones (renal calculi)
- Ureteral stones (stones located in the ureter)
- Bladder stones (less commonly)
These stones may be composed of various substances, such as calcium oxalate, uric acid, cystine, or struvite.
History and Evolution
The first forms of lithotripsy were mechanical and date back to the early 20th century, but the use of lasers in stone fragmentation became prevalent in the late 1980s and early 1990s. The Holmium:YAG (yttrium-aluminum-garnet) laser, introduced in the 1990s, is now regarded as the gold standard due to its safety, effectiveness, and versatility.
Advancements in Laser Technology
The development of finer, more flexible ureteroscopes and thinner, more efficient laser fibers has greatly expanded the possibilities of this technique. Recently, thulium fiber lasers have also emerged, offering potential advantages in terms of speed, precision, and reduced retropulsion of stone fragments.
Mechanism of Action
Laser lithotripsy works by delivering high-energy laser pulses directly to the surface of a urinary stone. The energy is absorbed by the stone, causing it to fragment into tiny pieces. These fragments can either be removed with specialized tools or pass naturally through the urinary tract.
The Holmium:YAG Laser
This laser operates at a wavelength of 2100 nm and is highly absorbed by water and biological tissues, making it ideal for use in the urinary system. The energy is transmitted through a flexible fiber, allowing the urologist to navigate the complex anatomy of the urinary tract.
Effect on Stones
Holmium lasers can fragment all known stone types, regardless of their hardness or composition. The laser’s precision minimizes collateral damage to surrounding tissue.
Indications and Patient Selection
Laser lithotripsy is indicated for patients with stones that:
- Are too large to pass spontaneously (typically >6-7 mm)
- Are causing obstruction, pain, infection, or bleeding
- Cannot be treated effectively by ESWL (e.g., hard stones, stones in challenging locations)
- Have failed previous treatments
It is suitable for patients of all ages, including children, although specific considerations apply for pediatric cases.
The Laser Lithotripsy Procedure
Preparation
Patients are typically evaluated with imaging studies such as CT scans, ultrasounds, or X-rays to determine the size, location, and number of stones. Preoperative blood and urine tests assess for infection or bleeding risks. Patients are often advised to stop certain medications, such as blood thinners, before the procedure.
Step-by-Step Overview
- Anesthesia: General or spinal anesthesia is usually administered.
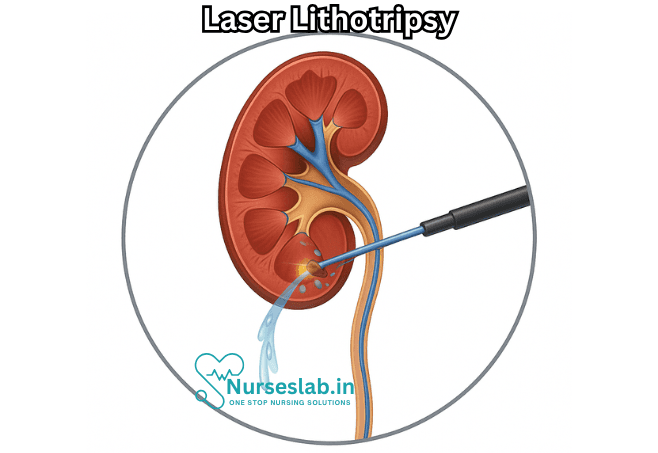
- Ureteroscopy: A thin, flexible or rigid tube (ureteroscope) is inserted through the urethra and bladder into the ureter or kidney.
- Stone Visualization: The stone is directly visualized via a video camera.
- Laser Fragmentation: A laser fiber is advanced through the ureteroscope. Pulses of laser energy are applied to the stone, fragmenting it into smaller pieces.
- Fragment Removal: Tiny fragments may be extracted with a basket device or allowed to pass naturally.
- Stent Placement: In some cases, a temporary ureteral stent is inserted to facilitate healing and urine flow.
Duration and Recovery
The procedure usually takes between 30 minutes and two hours, depending on the size and number of stones. Most patients can return home the same day or after a short hospital stay. Recovery is typically fast, with most returning to normal activities within a week.
Benefits of Laser Lithotripsy
- Minimally Invasive: No incisions are required, reducing pain and risk of infection.
- High Success Rate: Most stones can be completely fragmented in a single session.
- Versatility: Effective for virtually all stone types and locations.
- Shorter Recovery: Compared to open or percutaneous surgery, recovery time is minimal.
- Lower Complication Rates: The risk of serious complications is lower than with more invasive procedures.
Risks and Complications
Although generally safe, laser lithotripsy is not without risks. Possible complications include:
- Infection or sepsis
- Bleeding
- Injury to the urinary tract (ureteral perforation or stricture)
- Painful urination or hematuria (blood in urine)
- Migration of stone fragments
- Allergic reactions to anesthesia or contrast agents
Most complications can be managed conservatively, and serious events are rare.
Postoperative Care and Follow-Up
Patients may experience mild discomfort, frequent urination, or blood in the urine for a few days after the procedure. Drinking plenty of water helps flush out fragments and reduce irritation. Follow-up imaging may be ordered to ensure all fragments have cleared and to check for potential complications.
If a stent was placed, it is usually removed within one to two weeks. Patients should report any signs of infection (fever, chills, severe pain) promptly.
Comparisons with Other Stone Treatments
Extracorporeal Shock Wave Lithotripsy (ESWL)
ESWL is often used for smaller stones but may be less effective for hard stones or those in difficult locations. Laser lithotripsy provides direct visualization and a higher stone clearance rate for many patients.
Percutaneous Nephrolithotomy (PCNL)
PCNL is reserved for very large or complex stones and involves making a small incision in the back to access the kidney. While effective, it is more invasive than laser lithotripsy and has a longer recovery time.
Open Surgery
Once the standard of care, open surgery is now rarely performed due to the success of minimally invasive alternatives like laser lithotripsy.
Recent Advances and Future Directions
Laser lithotripsy continues to evolve with technological improvements, including:
- Miniaturization of ureteroscopes and laser fibers
- Introduction of thulium fiber lasers for improved efficiency
- Enhanced imaging and navigation techniques
- Robotic-assisted stone surgery
Research is ongoing to further reduce complications, improve stone clearance rates, and enhance patient comfort.
Patient Experiences and Outcomes
Most patients report high satisfaction with laser lithotripsy, citing minimal pain and quick return to daily life. Stone-free rates after a single procedure can exceed 90% for many stone types and locations.
Some factors that influence outcomes include:
- Stone size and composition
- Location within the urinary tract
- Patient anatomy and underlying health conditions
Nursing Care of Patients Undergoing Laser Lithotripsy
Laser lithotripsy offers several advantages, including high stone-free rates, minimal invasiveness, and a reduced risk of complications compared to open surgery. However, the procedure requires careful perioperative and postoperative nursing care to manage risks and promote recovery.
Preoperative Nursing Care
Comprehensive Assessment:
- Conduct a thorough assessment of the patient’s medical history, including previous urinary tract infections, bleeding disorders, allergies (especially to contrast dye or anesthesia), and comorbid conditions such as diabetes or hypertension. Review current medications to identify potential interactions or the need for cessation (e.g., anticoagulants).
Patient Education:
- Educate the patient and their family about the procedure, its purpose, expected outcomes, risks, and potential complications. Discuss alternatives and provide the opportunity for questions. Explain fasting requirements if general anesthesia is planned and review the importance of adhering to preoperative instructions.
Consent and Documentation:
- Ensure that informed consent is obtained and documented. Verify that all necessary preoperative tests (e.g., blood tests, coagulation profile, urinalysis, imaging studies) are completed and reviewed.
Preparation of the Patient:
- Assist the patient with hygiene measures, including shaving and cleansing the area as needed. Ensure the patient is wearing appropriate surgical attire. Establish intravenous access for administration of fluids, medications, and anesthesia.
Psychological Support:
- Address patient anxieties by providing reassurance, clarifying doubts, and offering emotional support. Anxiety can heighten the perception of pain and complicate recovery, so active listening and empathy are essential.
Intraoperative Nursing Care
Assisting with Positioning:
- Position the patient appropriately on the operating table, usually in the lithotomy or supine position, ensuring comfort and preventing nerve injury.
Monitoring Vital Signs:
- Continuously monitor heart rate, blood pressure, oxygen saturation, respiratory rate, and level of consciousness. Be vigilant for signs of adverse reactions to anesthesia or the procedure itself.
Maintaining Sterility:
- Ensure strict aseptic technique to reduce the risk of infection. Assist the surgical team in preparing and draping the patient.
Supporting the Surgical Team:
- Provide the necessary equipment and supplies, such as irrigation fluids, laser fibers, and baskets for stone retrieval. Anticipate the needs of the surgeon and be prepared to respond quickly to requests.
Patient Safety:
- Safeguard the patient from potential hazards, such as accidental burns from the laser or injury from instruments. Use protective eyewear for the team as required by laser safety protocols.
Immediate Postoperative Nursing Care
Post-Anesthesia Observation:
- Transfer the patient to the recovery area and monitor for recovery from anesthesia. Assess airway patency, breathing, circulation, and level of consciousness regularly. Observe for signs of complications such as respiratory depression, hypotension, or allergic reactions.
Pain Management:
- Assess pain using appropriate scales and administer analgesics as prescribed. Encourage non-pharmacologic pain relief measures, such as relaxation techniques, if appropriate.
Monitoring for Complications:
- Vigilantly observe for signs of bleeding (hematuria), infection (fever, chills, dysuria), urinary retention, or ureteric injury (flank pain, decreased urine output). Report any abnormalities promptly to the physician.
Fluid Balance and Urine Output:
- Maintain strict intake and output records. Ensure that the patient’s urinary output is adequate and the color of urine is monitored for changes (e.g., blood-tinged urine may be normal initially but should decrease over time).
Bladder Irrigation and Catheter Care:
- If an indwelling catheter is present, provide proper care to prevent infection and blockages. Monitor for passage of stone fragments in urine and educate the patient on what to expect.
Mobility and Early Ambulation:
- Encourage early mobilization as tolerated to prevent complications such as deep vein thrombosis and promote normal bowel and bladder function.
Emotional Support:
- Offer reassurance and guidance, especially if the patient is experiencing anxiety related to the procedure outcome or discomfort.
Ongoing and Discharge Nursing Care
Patient Education for Home Care:
- Educate the patient about expected postoperative symptoms, such as mild hematuria, dysuria, or passage of stone fragments. Instruct on the importance of maintaining hydration to facilitate passage of residual debris.
Recognition of Warning Signs:
- Teach patients and caregivers to recognize danger signs warranting immediate medical attention, including persistent severe pain, heavy bleeding, fever, chills, or difficulty urinating.
Medication Adherence:
- Instruct patients on the proper use of prescribed medications, such as pain relievers, antibiotics, or alpha-blockers. Emphasize the importance of completing any antibiotic course to prevent infection.
Prevention of Recurrence:
- Advise on lifestyle measures to reduce recurrence risk, including dietary modifications (e.g., reduced intake of oxalate-rich foods for calcium oxalate stones), adequate hydration, and regular follow-up with a healthcare provider.
Follow-Up Appointments:
- Ensure that the patient understands the schedule and purpose of follow-up visits for imaging, assessment of stone clearance, and potential stent removal if one was placed.
Special Considerations
Pediatric and Geriatric Patients:
- Tailor communication, education, and care according to the patient’s age and cognitive abilities. Engage family members in education and care planning.
Managing Co-Morbidities:
- Pay special attention to patients with diabetes, hypertension, renal impairment, or bleeding disorders. Collaborate with multidisciplinary teams to address these conditions and prevent perioperative complications.
Psychosocial Aspects:
- Address psychological impacts, such as anxiety, embarrassment, or fear related to urinary symptoms or recurrence. Consider referral to counseling or support groups if needed.
Complications and Nursing Interventions
While laser lithotripsy is generally safe, complications can occur, requiring prompt nursing intervention. Common complications and responses include:
- Hematuria:
- Monitor urine color and volume; increase fluid intake if appropriate; notify the physician if bleeding is heavy or persistent.
- Infection:
- Monitor temperature and signs of sepsis; maintain sterile technique in catheter care; administer antibiotics as prescribed.
- Ureteric Injury:
- Watch for severe pain, decreased urine output, or signs of peritonitis; report immediately to the medical team.
- Urinary Retention:
- Assess bladder fullness; assist with catheterization if necessary; provide reassurance and monitor for post-void residual volume.
REFERENCES
- Cui Y, Cao W, Shen H, et al. Comparison of ESWL and ureteroscopic holmium laser lithotripsy in management of ureteral stones. https://pubmed.ncbi.nlm.nih.gov/24498344/ PLoS One. 2014 Feb 3;9(2):e87634.
- Gao B, Bobrowski A, Lee J. A scoping review of the clinical efficacy and safety of the novel thulium fiber laser: The rising star of laser lithotripsy. Can Urol Assoc J. 2021 Feb;15(2):56-66.
- Feng C, Wu Z, Jiang H, Ding Q, Gao P. Ureteroscopic Holmium:YAG laser lithotripsy is effective for ureteral steinstrasse post-SWL.., https://pubmed.ncbi.nlm.nih.gov/23323772/ Minim Invasive Ther Allied Technol. 2013 Sep;22(5):279-82.
- Tzelves L, Somani B, Berdempes M, Markopoulos T, Skolarikos A. Basic and advanced technological evolution of laser lithotripsy over the past decade: An educational review by the European Society of Urotechnology Section of the European Association of Urology. Turk J Urol. 2021 May;47(3):183-192.
- National Kidney Foundation (U.S.). Lithotripsy. https://www.kidney.org/atoz/content/lithotripsy.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





