Introduction
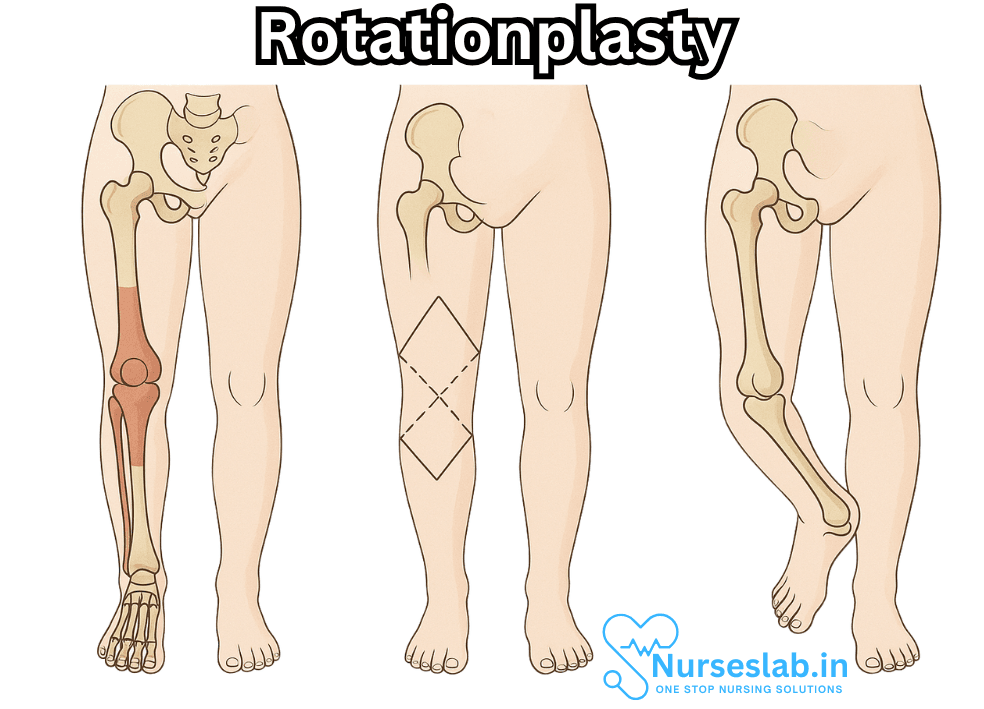
Rotationplasty is a remarkable and unconventional orthopedic surgical technique that transforms the lives of patients—most commonly children and adolescents—facing debilitating conditions or tumors in the lower limb. Instead of amputation, rotationplasty offers a functional alternative that preserves limb length and maximizes mobility. This procedure, which may appear unusual at first glance, involves removing a diseased section of the limb and rotating the remaining portion, allowing the ankle to function as a substitute knee joint. While rotationplasty is most widely recognized as a treatment for bone cancers such as osteosarcoma, its applications extend to other rare conditions as well.
The Historical Evolution of Rotationplasty
The origins of rotationplasty date back to the early 20th century, with the Austrian surgeon Dr. Van Nes first describing the procedure as a solution for congenital femoral deficiencies. Over time, rotationplasty evolved, finding a prominent role in limb-sparing surgeries for pediatric patients with malignant bone tumors. Its use gradually expanded internationally, becoming a specialized but invaluable technique within orthopedic oncology.
The Surgical Technique
Rotationplasty requires meticulous planning and execution. The operation typically involves the following steps:
- Preoperative Assessment: Surgeons assess tumor size, location, and involvement of neurovascular structures. Advanced imaging techniques, such as MRI and CT scans, help map out the precise region for resection and ensure the viability of the remaining limb.
- Resection of the Diseased Segment: The affected portion—often the distal femur and adjacent knee joint—is surgically removed. Great care is taken to preserve blood vessels and nerves to maintain function in the remaining limb.
- Rotation and Reattachment: The lower limb is rotated 180 degrees so that the ankle faces backward. The rotated limb is then reattached to the upper thigh or femur, effectively positioning the ankle where the knee used to be.
- Soft Tissue Reconstruction: Muscles and tendons are adjusted and reattached to ensure stability and optimize movement.
- Postoperative Care and Rehabilitation: Patients undergo extensive rehabilitation, learning to use their newly configured limb. A custom prosthetic device is fitted, with the foot now functioning as the knee joint within the prosthesis.
Indications for Rotationplasty
Rotationplasty is primarily indicated for:
- Osteosarcoma and Ewing’s Sarcoma: Two of the most common malignant bone tumors in children and adolescents, often located around the knee.
- Congenital Limb Deficiencies: Such as proximal femoral focal deficiency (PFFD), where the upper thigh bone is underdeveloped or absent.
- Revision Procedures: In rare cases, rotationplasty may be used after failed limb-sparing or reconstructive surgeries.
Functional Advantages
At the heart of rotationplasty is the preservation of limb function. Unlike above-the-knee amputation, rotationplasty allows the patient to retain voluntary control over their “new knee”—the rotated ankle. This offers several advantages:
- Enhanced Mobility: The patient can walk, run, jump, and participate in sports more easily than with a traditional amputation.
- Improved Proprioception: The patient retains sensation in the foot (now functioning as the “knee”), which aids in balance and movement.
- Durability: The procedure is especially suited for children, as the limb continues to grow, and the mechanics of the rotated ankle adapt to the demands of daily life.
Challenges and Complications
Rotationplasty is not without its challenges, both medical and psychological. Complications can include:
- Wound Healing Issues: As with any major limb surgery, there is a risk of delayed healing, infection, and tissue breakdown.
- Vascular and Neurological Problems: Careful preservation of blood vessels and nerves is critical; injury during surgery can lead to loss of function or sensation.
- Prosthetic Fitting Difficulties: Customizing the prosthesis to accommodate the reversed limb requires specialized expertise and ongoing adjustments.
- Psychosocial Impact: The appearance of the limb after rotationplasty is markedly different—some patients and families need significant support to adjust to the cosmetic outcome and social reactions.
Rehabilitation and Life After Rotationplasty
Rehabilitation plays a pivotal role in the success of rotationplasty. After surgery, patients embark on a comprehensive physical therapy program tailored to their unique needs. The process includes:
- Muscle Strengthening: Building strength in the muscles of the hip, thigh, and rotated limb to support movement and stability.
- Gait Training: Learning to walk with the new limb configuration and prosthesis, focusing on alignment and balance.
- Adaptation to Daily Life: Therapists work closely with patients to ensure they regain independence in daily activities, including climbing stairs and participating in recreational sports.
Notably, many individuals who undergo rotationplasty report high levels of satisfaction with their mobility and quality of life. They often return to active lifestyles, with some achieving notable success in competitive athletics.
Psychological Considerations and Support
The psychological journey following rotationplasty is as vital as the physical rehabilitation. Patients—particularly children and adolescents—may experience a range of emotions, from relief at avoiding amputation to anxiety about their limb’s appearance. Support from family, peer groups, and mental health professionals is essential. Many hospitals provide counseling services to help patients build self-confidence and adapt to the changes.
Aesthetic and Social Perspectives
The visual result of rotationplasty—a backward-facing foot—is striking and can provoke curiosity or misunderstanding among peers. Education and advocacy are important tools for patients and families to foster acceptance and understanding in schools and communities. Over time, most individuals develop a sense of pride in their unique journey, becoming ambassadors for resilience and innovation in medicine.
Notable Cases and Public Awareness
Rotationplasty has garnered public attention through documentaries, medical campaigns, and the stories of inspirational patients. Notably, some athletes and public figures who have undergone the procedure have used their platforms to encourage others facing similar medical challenges. Their stories provide hope and demonstrate the possibilities for life after rotationplasty.
Recent Advances and Future Directions
Modern rotationplasty continues to benefit from advances in surgical technique, imaging, and prosthetic design. Researchers are exploring improvements in nerve preservation, muscle reconstruction, and prosthetic integration to further enhance outcomes. Emerging technologies, such as robotics and 3D printing, hold promise for customizing prosthetics and streamlining rehabilitation.
Nursing Care of Patients with Rotationplasty
The role of nurses in managing rotationplasty patients is critical from the preoperative phase through long-term follow-up, addressing holistic patient needs and promoting optimal outcomes.
1. Preoperative Nursing Care
1.1 Patient and Family Education
- Explaining the Procedure: Nurses must ensure the patient and their family understand the complexities of rotationplasty, including the anatomical changes, expected outcomes, and rehabilitation process. Visual aids, videos, and models can enhance comprehension.
- Setting Realistic Expectations: Discuss potential functional outcomes, cosmetic appearance, and the long-term rehabilitation journey to help patients develop a realistic outlook.
- Psychological Preparation: Address emotional and psychological concerns, particularly regarding body image, loss of limb, and adaptation to the new limb structure. Referral to counseling or support groups is often beneficial.
1.2 Preoperative Assessments
- Physical Assessment: Baseline evaluation of the patient’s physical status, including range of motion, muscle strength, neurovascular status, and skin integrity of the affected limb.
- Laboratory and Diagnostic Work: Ensure all preoperative investigations, such as imaging and blood tests, are complete and abnormalities are reported to the surgical team.
- Prehabilitation: Collaborate with physiotherapists to start strengthening exercises and mobility training, if feasible, to prepare for postoperative rehabilitation.
2. Immediate Postoperative Nursing Care
2.1 Monitoring and Assessment
- Vital Signs and Hemodynamic Stability: Monitor for signs of hypovolemia, shock, or infection, following hospital protocols for frequency and documentation.
- Neurovascular Checks: Assess color, temperature, capillary refill, pulses, and sensation in the rotated limb regularly to detect vascular compromise or compartment syndrome promptly.
- Pain Management: Individualized pain control plans often involve multimodal analgesia, including opioids, NSAIDs, and regional anesthesia. Assess pain regularly and adjust medications as needed.
2.2 Wound and Limb Care
- Wound Monitoring: Inspect surgical incisions for signs of infection, dehiscence, hematoma, or delayed healing. Keep the site clean and dry, following aseptic dressing change protocols.
- Drain and Catheter Management: Care for surgical drains and urinary catheters as required, monitoring for output and infection.
- Positioning: Support the limb in a functional position, prevent pressure injuries, and encourage early gentle movement as allowed by the surgical team.
2.3 Prevention of Complications
- Infection Prevention: Encourage hand hygiene, monitor for fever, and educate the patient on infection signs.
- Deep Vein Thrombosis (DVT) Prophylaxis: Use compression stockings, pharmacologic agents, and early mobilization as ordered.
- Pressure Injury Prevention: Reposition the patient regularly and assess skin integrity frequently.
3. Rehabilitation and Functional Training
3.1 Early Mobilization
- Collaboration with Physical Therapy: Nurses work with therapists to initiate mobility exercises and gait training, often starting within days of surgery as appropriate.
- Patient Motivation: Encourage active participation, celebrate milestones, and address fears related to movement and falls.
3.2 Prosthetic Fitting and Training
- Stump Shaping and Skin Care: Teach proper limb bandaging and skin inspection techniques to prepare for prosthesis.
- Prosthetic Education: Guide the patient and caregivers in donning, doffing, and caring for the prosthetic limb. Practice safe ambulation and activities of daily living (ADLs).
3.3 Occupational Therapy and Daily Living Skills
- ADL Training: Foster independence in self-care, hygiene, dressing, and household tasks, adapting techniques as needed for the new limb orientation.
- Home and School Reintegration: Prepare for transition to home, school, or work environments by identifying barriers and coordinating resources.
4. Psychological and Social Support
4.1 Addressing Body Image and Self-esteem
- Body Image Counseling: Patients may experience distress related to the altered appearance of their limb. Offer emotional support, refer to mental health professionals, and encourage participation in peer support networks.
- Promoting Resilience: Reinforce the patient’s strengths and progress, encouraging goal setting and a positive outlook for the future.
4.2 Family and Community Involvement
- Family Education: Engage family members in care routines, rehabilitation, and emotional support strategies.
- Community Resources: Connect patients and families with community organizations, adaptive sports programs, and advocacy groups for individuals with limb differences.
5. Long-term Nursing Care and Follow-up
5.1 Monitoring for Late Complications
- Orthopedic and Functional Assessments: Monitor for prosthetic fit issues, limb length discrepancies, and joint contractures. Refer for adjustments as needed.
- Infection Surveillance: Chronic wound care may be necessary for some patients. Educate on long-term skin and soft tissue monitoring.
- Growth and Developmental Considerations: For pediatric patients, monitor for changes in limb growth and alignment, collaborating with orthopedic specialists.
5.2 Health Maintenance and Quality of Life
- Physical Fitness: Encourage ongoing exercise, recreational activities, and participation in sports suited to the individual’s abilities and interests.
- Mental Health: Continue to assess for signs of depression, anxiety, or social withdrawal, facilitating access to counseling services as needed.
- Education and Vocational Planning: Support return to school or work, advocating for necessary accommodations and assistive technologies.
6. Patient and Family Education
Education must be continuous and tailored to the patient’s developmental stage, learning preferences, and cultural background. Key teaching points include:
- Limb and Prosthesis Care: Daily skin checks, cleaning, and maintenance routines.
- Warning Signs: When to seek medical attention for infection, prosthetic issues, or decreased limb function.
- Lifestyle Adaptation: Tips for safe physical activity, transportation, and travel.
- Peer Support: Value of connecting with others who have undergone rotationplasty or similar procedures.
7. Ethical and Cultural Considerations
Nursing care must be patient-centered, respecting diverse values and preferences:
- Informed Consent: Ensure ongoing dialogue about risks, benefits, and alternatives throughout care.
- Respecting Cultural Beliefs: Adapt care practices to honor cultural and spiritual values related to illness, body image, and healing.
- Advocacy: Stand as an advocate for the patient’s rights, dignity, and autonomy in all healthcare settings.
REFERENCES
- Bernthal NM, Monument MJ, Randall RL, Jones KB. Rotationplasty: Beauty is in the Eye of the Beholder. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4234076/. Oper Tech Orthop. 2014 Jun 1;24(2):103-110.
- Fuchs B, Sim FH. Rotationplasty about the knee: surgical technique and anatomical considerations. Clin Anat. 2004 May;17(4):345-53. doi: 10.1002/ca.10211. PMID: 15108342.
- Gaillard J, Fouasson-Chailloux A, Eveno D, Bokobza G, et al. Rotationplasty Salvage Procedure as an Effective Alternative to Femoral Amputation in an Adult With a History of Osteosarcoma: A Case Report and Review. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8776644/. Front Surg. 2022 Jan 7;8:820019.
- Gupta SK, Alassaf N, Harrop AR, Kiefer GN. Principles of rotationplasty. J Am Acad Orthop Surg. 2012 Oct;20(10):657-67. doi: 10.5435/JAAOS-20-10-657. PMID: 23027695.
- Nicholas M. Bernthal, Michael J. Monument, R. Lor Randall, Kevin B. Jones, Rotationplasty: Beauty is in the Eye of the Beholder, Operative Techniques in Orthopaedics, Volume 24, Issue 2, 2014, Pages 103-110, ISSN 1048-6666, https://www.sciencedirect.com/science/article/pii/S1048666614000020
- OncoLink. Surgical Procedures: Rotationplasty. https://www.oncolink.org/cancers/sarcomas/sarcoma-bone/rotationplasty. Reviewed 11/8/2022.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





