Introduction
Sacral Nerve Stimulation (SNS), also known as sacral neuromodulation, is an advanced and evolving therapeutic technique that has revolutionized the management of certain urinary and bowel disorders. For individuals suffering from conditions like overactive bladder, urinary retention, or fecal incontinence—where conventional treatments fail to provide relief—SNS offers a beacon of hope. This document delves into the science behind SNS, its applications, the procedure, outcomes, risks, and its impact on patient lives.
Understanding the Sacral Nerves
The sacral nerves are a group of nerves located in the lower back (sacrum) that play a pivotal role in regulating the muscles and functions of the pelvic organs, including the bladder, bowel, and sphincters. These nerves transmit signals between the brain and these organs, controlling voluntary and involuntary actions such as urination and defecation. Dysfunction in the neural pathways—due to injury, disease, or unknown causes—can result in loss of control, urgency, frequency, and incontinence.
What is Sacral Nerve Stimulation?
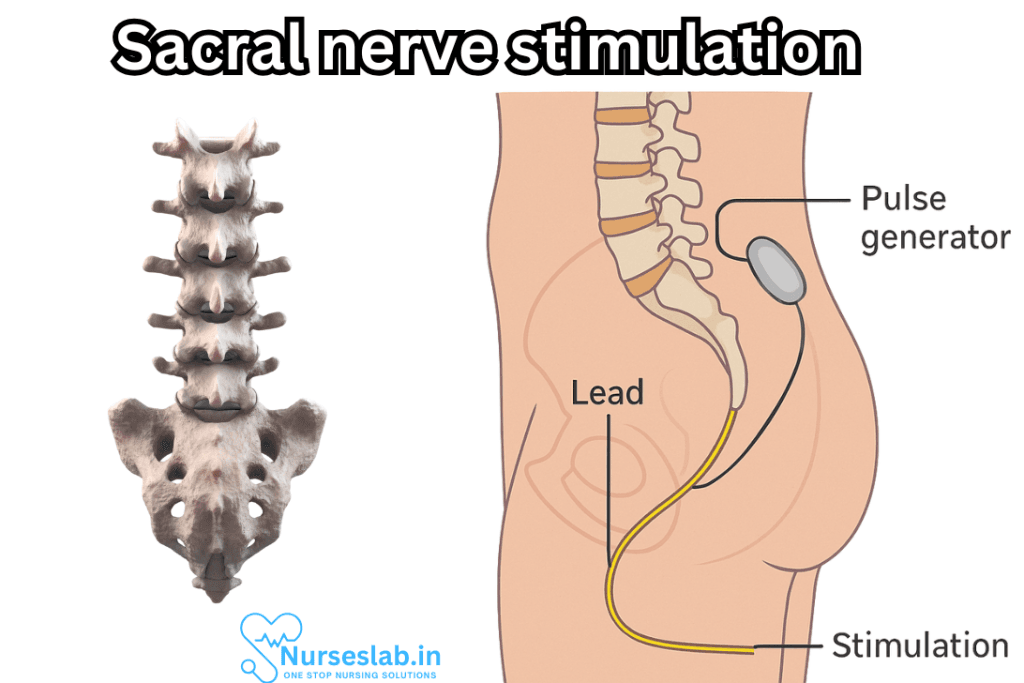
Sacral Nerve Stimulation is a minimally invasive, reversible therapy that involves electrical stimulation of the sacral nerves, primarily the S3 nerve root, to modulate neural pathways controlling the bladder and bowel. By delivering gentle electrical impulses via a small, implanted device, SNS restores normal communication between the nervous system and the pelvic organs. The therapy is akin to a “pacemaker” for the bladder and bowel, helping to re-establish balance and control.
Indications and Applications
SNS is indicated for patients whose symptoms are refractory to conservative and pharmacological treatments. The most common applications include:
- Overactive Bladder (OAB): Characterized by urgency, frequency, and urge incontinence.
- Non-obstructive Urinary Retention: Difficulty emptying the bladder without a physical blockage.
- Fecal Incontinence: Involuntary loss of stool or the inability to control bowel movements.
- Chronic Pelvic Pain: In select cases where pelvic pain is associated with dysfunction of the pelvic organs.
SNS is not typically recommended for patients with anatomical abnormalities of the urinary tract, active infections, or certain neurological disorders.
The SNS Procedure: Step by Step
The SNS procedure is usually completed in two stages:
1. Evaluation (Test or Trial Phase)
During this phase, a temporary lead (thin wire) is placed near the sacral nerve through a minor, outpatient procedure under local anesthesia. The lead is connected to an external stimulator worn on a belt or harness. Over a period ranging from several days to a few weeks, the patient’s symptoms are closely monitored to determine if significant improvement—often defined as at least 50% reduction in symptom severity—is achieved. The trial phase helps identify suitable candidates for permanent implantation.
2. Permanent Implantation
If the trial phase is successful, a permanent neurostimulator (similar to a small pacemaker) is implanted beneath the skin, typically in the upper buttock or lower back. The lead is connected to the device, which delivers controlled electrical pulses. The device settings can be adjusted externally by healthcare professionals to optimize therapy for individual needs.
How Does SNS Work?
While the precise mechanism of action of SNS remains under investigation, it is believed that electrical stimulation “resets” or modulates the activity of the sacral nerves, thereby normalizing pelvic organ function. This neuromodulation can suppress abnormal signals (such as those leading to urgency or incontinence) and restore voluntary control. The therapy is dynamic—settings can be fine-tuned over time based on the patient’s response.
Benefits of Sacral Nerve Stimulation
SNS offers a range of potential benefits for eligible patients:
- Significant reduction or resolution of incontinence episodes
- Decreased urinary urgency and frequency
- Restored ability to sense bladder or bowel fullness
- Improved quality of life and increased independence
- Reversibility—device can be turned off or removed if necessary
Potential Risks and Complications
Like any medical procedure, SNS carries certain risks:
- Surgical site pain, infection, or bleeding
- Lead migration or breakage
- Device malfunction or battery issues
- Unpleasant stimulation sensations
- Allergic reaction to implanted materials
Most adverse effects are mild or can be managed by adjusting device settings or, if needed, removing the device.
Living with Sacral Nerve Stimulation
Patients with an SNS device can resume most daily activities, including work, exercise, and travel. Some precautions may be necessary—such as avoiding certain MRI machines or security systems that interfere with the device. Periodic follow-up is essential to monitor device function and symptom control. Battery life ranges from 5 to 10 years, depending on usage, after which a minor surgical procedure is required for replacement.
Efficacy and Patient Outcomes
Clinical studies have demonstrated that SNS can lead to substantial and sustained improvement in symptoms for a significant proportion of patients. Long-term data indicate that:
- 70-80% of patients experience at least a 50% reduction in urinary or fecal incontinence symptoms
- Improvements are often maintained over several years
- Many patients reduce or discontinue medications previously required for symptom management
- High satisfaction rates owing to increased confidence, freedom, and social participation
Who Is a Candidate?
Appropriate candidates for SNS are typically adults with chronic symptoms who have not responded to behavioral therapies, medications, or other less invasive interventions. Candidates undergo thorough evaluation—including urodynamic testing, symptom diaries, and psychological assessment—to ensure the best possible outcomes.
Future Directions and Innovations
Ongoing research seeks to refine SNS technology and expand its applications. Innovations in device miniaturization, wireless communication, and battery life are on the horizon. Some studies explore the role of SNS in other conditions, such as chronic constipation or neurogenic bladder due to spinal cord injury. As the understanding of neuromodulation deepens, SNS may become increasingly versatile and accessible.
Nursing Care of Patients with Sacral Nerve Stimulation
Nursing professionals play a pivotal role in guiding patients through preparation, the perioperative period, and long-term management, ensuring safety, comfort, and optimal function.
Preoperative Nursing Assessment and Preparation
- Patient Education: Explain the purpose, expected outcomes, and possible risks of SNS therapy. Encourage questions and address anxieties to foster informed decision-making.
- Baseline Assessments: Document urinary and bowel function, pain levels, psychological status, and any comorbid conditions. This provides a foundation for postoperative comparison.
- Medication Review: Assess for anticoagulant or antiplatelet use and collaborate with the multidisciplinary team regarding perioperative management.
- Skin Integrity: Examine the sacral area and anticipated implant site for signs of infection, ulceration, or other pathology.
- Preoperative Instructions: Review fasting protocols and preoperative hygiene. Advise on cessation of smoking and maintaining good nutrition to enhance healing.
Immediate Postoperative Nursing Care
- Vital Signs and Neurovascular Monitoring: Regularly assess vital signs, paying close attention to changes that may indicate bleeding or infection. Monitor lower limb sensation and movement.
- Incision Care: Inspect the surgical site for excessive exudate, erythema, swelling, or signs of wound dehiscence. Maintain aseptic technique during dressing changes.
- Pain Management: Administer prescribed analgesics, considering both pharmacological and non-pharmacological methods. Assess pain using validated scales.
- Urinary Retention: Assess for difficulty voiding and bladder distension. Assist with catheter care if required and advocate for early removal when appropriate to reduce infection risk.
- Mobility and Fall Prevention: Support safe mobilisation, especially in the initial hours after surgery. Educate about gradual increase in activity and avoiding positions that may strain the implant site.
- Device Function Verification: Collaborate with the surgical and technical team to confirm correct device operation. Educate the patient to recognise indicators of malfunction (such as lack of symptom improvement or abnormal sensations).
Late Complications and Ongoing Surveillance
- Wound Dehiscence: Educate the patient to monitor for gaping or breakdown of the incision site. Early intervention reduces risk of further complications.
- Scarring and Body Image Concerns: Address concerns compassionately and refer to support services if desired.
- Implant Issues: Watch for implant migration, extrusion, or chronic discomfort. Educate regarding the need for prompt medical review if these occur.
- Infection Prevention: Teach signs of infection—such as fever, increased redness, or discharge—and when to seek medical attention.
- Device Troubleshooting: Instruct patients on the use of device controllers, charging protocols if applicable, and what to do if the device malfunctions.
Long-Term Follow-Up and Health Maintenance
- Continued Surveillance: Monitor long-term wound healing, scarring, and function during follow-up visits. Document any changes in symptoms or device efficacy.
- Psychological Well-being: Assess for ongoing mental health support needs, especially as chronic symptoms can impact quality of life. Facilitate access to resources such as counselling or support groups.
- Sexual and Urological Function: Support discussions around sexual health, sensation, and urinary function. Refer to specialists as needed for any concerns.
- Health Promotion: Encourage healthy lifestyle choices, such as regular exercise and smoking cessation, to optimise healing and overall health.
- Education and Empowerment: Equip patients with comprehensive information about living with an SNS device, including travel, security screening, and compatibility with other medical procedures.
Patient Teaching and Self-Management
- Device Care: Advise patients to avoid strenuous activities or direct trauma to the implant site. Reinforce importance of routine device checks and follow-up appointments.
- Symptom Monitoring: Instruct patients to keep symptom diaries, noting any changes in urinary or bowel habits, pain, or general well-being.
- Emergency Preparedness: Provide clear instructions on whom to contact in case of device failure, unexpected symptoms, or signs of infection.
Interprofessional Collaboration
- Team Approach: Work closely with urologists, colorectal surgeons, physiotherapists, and mental health professionals to address complex needs.
- Communication: Ensure all relevant changes or concerns are documented and communicated promptly to the care team.
Psychosocial Support and Quality of Life
- Individualised Care: Recognise the unique challenges and concerns for each patient. Provide reassurance, promote autonomy, and respect patient preferences.
- Support Networks: Encourage engagement with peer support groups or online communities for shared experiences and advice.
REFERENCES
- Brusciano L, Brillantino A, Pellino G, et.al. Sacral nerve modulation for patients with fecal incontinence: long-term outcome and effects on sexual function. https://pubmed.ncbi.nlm.nih.gov/37442886/. Updates Surg. 2023 Aug;75(5):1187-1195.
- Feloney MP, Stauss K, Leslie SW. Sacral Neuromodulation. https://www.ncbi.nlm.nih.gov/books/NBK567751/. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Updated 4/18/024.
- De Wachter S, et al. (2020). New technologies and applications in sacral neuromodulation: An update.
https://link.springer.com/article/10.1007/s12325-019-01205-z - Feloney MP, Stauss K, Leslie SW. Sacral Neuromodulation. [Updated 2024 Apr 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK567751/
- Sukhu T, Kennelly MJ, Kurpad R. Sacral neuromodulation in overactive bladder: a review and current perspectives. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5087764/ Res Rep Urol. 2016 Oct 26;8:193-199.
- Wang X, Chen JD. Therapeutic potential and mechanisms of sacral nerve stimulation for gastrointestinal diseases. https://pubmed.ncbi.nlm.nih.gov/37408571/. J Transl Int Med. 2023 Jul 5;11(2):115-127.
- Harvie HS, et al. (2020). Cost-effectiveness of sacral neuromodulation versus onabotulinumtoxinA for refractory urgency urinary incontinence: Results of the ROSETTA randomized trial.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7204548/
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





