Introduction
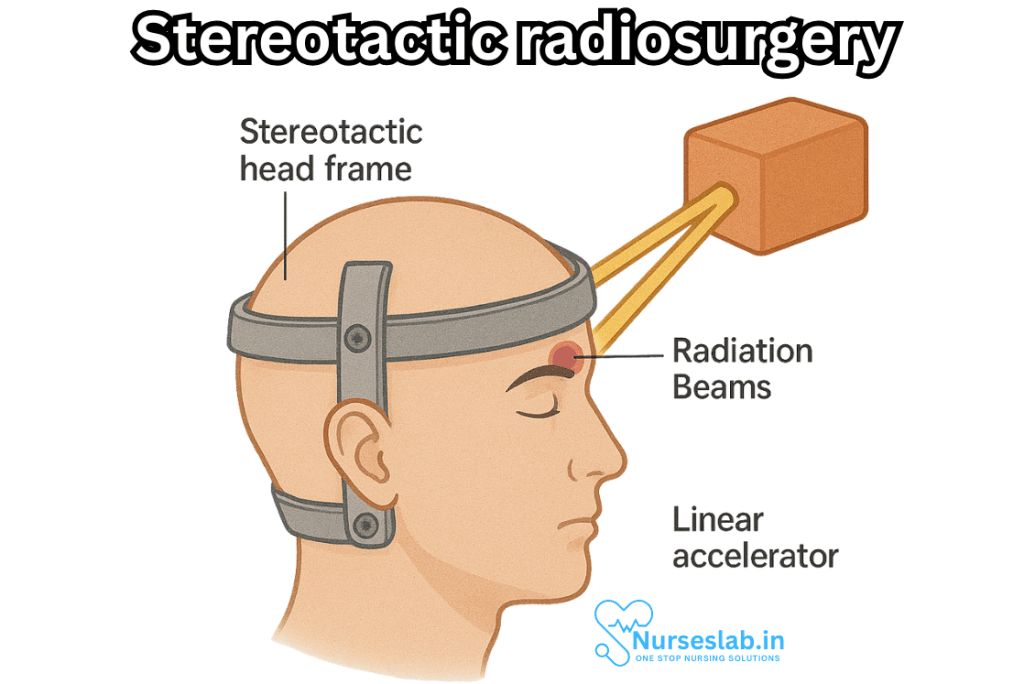
Stereotactic radiosurgery (SRS) stands as a pillar of innovation in contemporary neurosurgery and oncology, blending advanced imaging technologies and focused radiation therapy to treat a spectrum of conditions with accuracy once inconceivable. Despite the term “surgery,” SRS is a non-invasive procedure that forgoes the scalpel in favor of highly targeted radiation beams, delivering potent doses to specific areas within the brain or body. This technique offers patients new hope for conditions previously deemed inoperable or high-risk for traditional surgery.
Historical Context
The roots of stereotactic radiosurgery trace back to 1951, when Swedish neurosurgeon Lars Leksell conceptualized and created the first stereotactic frame and the Gamma Knife, revolutionizing the treatment landscape for intracranial lesions. The introduction of SRS marked a paradigm shift, allowing for precise targeting of tumors and disorders within the brain without the need for open surgery. Over the decades, the field evolved, integrating sophisticated imaging modalities and expanding its application from brain lesions to extracranial sites such as the spine and lungs.
Principles of Stereotactic Radiosurgery
SRS relies on three foundational principles:
- Precision: Using stereotactic guidance—meaning spatial localization within a three-dimensional coordinate system—SRS pinpoints lesions with millimeter-level accuracy.
- High-dose radiation: Delivers a concentrated dose of radiation in one or a few sessions, minimizing exposure to surrounding healthy tissue.
- Non-invasiveness: Unlike conventional surgery, SRS does not require incisions or general anesthesia, reducing recovery time and risk of infection.
Technologies Used in SRS
Several systems enable the delivery of SRS:
- Gamma Knife: Specialized for brain lesions, uses cobalt-60 sources to emit focused gamma rays.
- Linear Accelerator (LINAC): Versatile machine capable of treating both cranial and extracranial lesions, utilizing X-rays shaped to the target’s contours.
- CyberKnife: A robotic system that allows for real-time tracking of tumors, adapting to patient movement and delivering radiation with unparalleled flexibility.
Each technology offers unique advantages, tailored to lesion location, size, and patient-specific factors.
The SRS Procedure
The process of stereotactic radiosurgery is meticulously orchestrated and typically follows these steps:
1. Patient Preparation and Immobilization
For cranial procedures, patients may wear a rigid head frame or a custom-fitted mask to prevent movement. For extracranial sites, body frames and markers are used. This immobilization is crucial for precise targeting.
2. Imaging and Treatment Planning
High-resolution MRI, CT, and sometimes PET scans are performed to delineate the tumor or abnormal tissue. Advanced software integrates these images to build a 3D map, allowing radiation oncologists, physicists, and neurosurgeons to plan optimal beam trajectories and doses.
3. Radiation Delivery
Patients are positioned in the treatment suite, and the selected SRS machine delivers radiation from multiple angles, converging beams at the target. The process may last from a few minutes to several hours, depending on the system and complexity of the treatment plan.
4. Post-Treatment Care
SRS is typically an outpatient procedure. Patients can often return home the same day, with minimal recovery time. Follow-up imaging is scheduled to monitor treatment response and detect any delayed side effects.
Clinical Applications of SRS
SRS is indicated for a diverse array of conditions, including:
1. Intracranial Tumors
- Metastatic Brain Tumors: SRS is frequently used to treat metastases from cancers such as lung, breast, and melanoma, especially when surgical removal is not feasible.
- Primary Brain Tumors: Includes meningiomas, gliomas, and acoustic neuromas. SRS can offer control with fewer cognitive side effects compared to whole-brain radiotherapy.
- Pituitary Adenomas: Small, benign tumors of the pituitary gland are often accessible to SRS, sparing critical nearby structures.
2. Vascular Malformations
- Arteriovenous Malformations (AVMs): SRS induces gradual closure of abnormal blood vessels over months to years, reducing the risk of hemorrhage.
3. Functional Disorders
- Trigeminal Neuralgia: SRS targets the trigeminal nerve root entry zone, providing pain relief for patients resistant to medical therapy.
- Movement Disorders: Select cases of epilepsy and essential tremor may benefit from precisely targeted radiosurgical ablation.
4. Extracranial Lesions
As stereotactic body radiotherapy (SBRT), the principles of SRS have been extended to treat tumors in the spine, lung, liver, prostate, and pancreas.
Advantages and Limitations
Advantages:
- Minimally invasive, no incisions
- Outpatient procedure with rapid return to normal activities
- Potentially lower risk of complications such as infection, bleeding, and cognitive impairment
- Can treat surgically inaccessible or multiple lesions
- Often used when prior radiation limits additional therapy options
Limitations and Risks:
- Delayed response; some tumors or AVMs may take months or years to shrink or occlude
- Possible radiation injury to surrounding tissues, leading to edema, necrosis, or neurocognitive changes
- Not suitable for very large tumors or diffuse disease
- Rare risk of secondary malignancy due to radiation exposure
Outcomes and Patient Experience
High rates of tumor control are observed in many SRS-treated conditions, especially small brain metastases, benign tumors, and AVMs. Quality of life is often preserved, with a lower incidence of post-treatment fatigue and cognitive decline compared to conventional therapies. Complications, when they occur, are usually transient but require vigilance and coordinated follow-up care.
Patients typically report satisfaction with the convenience and minimal disruption to daily life. Support from a multidisciplinary team—including neurosurgeons, radiation oncologists, medical physicists, and nurses—ensures a comprehensive approach from evaluation through long-term monitoring.
Current Research and Future Directions
Ongoing research in stereotactic radiosurgery is focused on refining targeting algorithms, reducing side effects, and expanding indications. Innovations include:
- Integration of artificial intelligence in treatment planning
- Adaptive radiotherapy systems that respond to real-time changes in tumor position
- Combining SRS with immunotherapy or targeted molecular agents for synergistic effects
- Exploring the role of SRS in pediatric tumors and rare conditions
Clinical trials continue to assess the safety and efficacy of SRS for new applications and to determine long-term outcomes in diverse patient populations.
Ethical Considerations
As with any advanced medical technology, SRS presents ethical challenges, including access to care, cost, and informed consent. Ensuring equitable availability requires investment in training, infrastructure, and patient education. Rigorous multidisciplinary evaluation is essential to avoid overtreatment and to tailor therapy to individual patient needs.ks that your healthcare provider will explain. They depend largely on the specific site that needs to be treated.
Nursing Care of Patients Undergoing Stereotactic Radiosurgery
As this treatment modality becomes increasingly common, nurses play a vital role in the preparation, care, and recovery of patients undergoing SRS, providing targeted support, education, and monitoring to ensure safety and comfort.
Nursing Responsibilities: Pre-procedure Phase
Patient Assessment
Nurses conduct a comprehensive assessment, including medical history, neurological status, allergies, and prior experiences with radiation therapy. Baseline vital signs and laboratory results are reviewed to identify any contraindications or risks.
Patient Education
Education is central to reducing anxiety and improving cooperation. Nurses should explain:
- The purpose and process of SRS
- Expected benefits and potential risks/side effects
- The need for immobilization during imaging and treatment
- Likely absence of surgical incision or general anesthesia
- Possible requirement for a stereotactic frame (for some systems), which may be temporarily uncomfortable but is essential for accuracy
- Pre-procedure instructions, such as fasting if sedation is used, and medication management
Providing written and verbal information tailored to the patient’s comprehension level is recommended, and family members or caregivers should be included in the discussion.
Psycho-emotional Support
Patients may feel apprehensive about the diagnosis, treatment, or the unfamiliar technology. Nurses offer reassurance, attentive listening, and referrals to counseling services or support groups as needed.
Physical Preparation
- Ensure the patient has removed any metal objects (jewelry, hairpins, hearing aids, dentures) prior to imaging.
- If a frame is to be applied, assist the physician in positioning and securing it to the patient’s head. Monitor for discomfort and provide analgesia or local anesthesia as prescribed.
- Obtain intravenous access if contrast agents or sedation will be administered.
Intra-procedure Nursing Care
Patient Positioning and Monitoring
Proper immobilization is crucial for the accuracy of SRS. Nurses assist in positioning the patient on the treatment table, confirming comfort and alignment. Throughout the procedure, they monitor for signs of anxiety, claustrophobia, or pain, and communicate with the patient via intercom systems in the treatment suite.
Safety and Infection Control
Aseptic technique is mandatory during frame application or intravenous access. Equipment is checked for proper function, and emergency protocols are reviewed in case of an unexpected reaction.
Patient Support
- Offer reassurance and maintain communication throughout the procedure.
- Monitor for signs of distress, allergic reactions to contrast, or changes in neurological status.
- Document procedure details and any patient-reported symptoms.
Post-procedure Nursing Care
Immediate Post-procedure Assessment
Upon completion, nurses perform a thorough assessment, including:
- Vital signs monitoring (every 15-30 minutes for the first hour or as per institutional protocol)
- Neurological checks to identify early complications such as seizures, headache, or confusion
- Inspection of frame sites for bleeding, swelling, or infection
- Observation for nausea, vomiting, dizziness, or other side effects
Pain and Symptom Management
Patients may experience mild headache, scalp tenderness (especially after frame removal), or fatigue. Nurses provide prescribed analgesics, antiemetics, and comfort measures such as a cool compress.
Patient Education and Discharge Planning
Before discharge, nurses reinforce key instructions:
- Signs and symptoms requiring immediate medical attention (severe headache, persistent vomiting, focal neurological deficits, signs of infection)
- Wound care for frame pin sites, if applicable
- Medication schedule, including corticosteroids or anticonvulsants if prescribed
- Expected side effects: mild fatigue, headache, temporary hair loss, and scalp sensitivity are common and usually self-limited
- Activity restrictions: most patients may resume normal activities within a day, but should avoid strenuous exercise for a short period
- Follow-up appointments for imaging and clinical review
Written discharge instructions and contact information for the treating team are provided.
Long-term Nursing Care and Follow-up
Ongoing Assessment
Nurses play a key role in monitoring patients during follow-up visits. They assess for:
- Delayed side effects such as radiation necrosis, edema, or neurocognitive changes
- Psychological adjustment and quality of life
- Adherence to medication and follow-up schedule
- Any signs of tumor recurrence or progression
Coordination of Multidisciplinary Care
Nurses often coordinate with neurosurgeons, radiation oncologists, social workers, and rehabilitation therapists to address the diverse needs of SRS patients. They facilitate referrals, schedule appointments, and act as patient advocates.
Patient and Family Support
Ongoing education and support are provided to help patients and their families cope with the uncertainty and emotional burden of a neurological diagnosis. Support groups, counseling services, and educational materials may be recommended.
Potential Complications and Nursing Interventions
While SRS is generally safe, complications—though rare—may occur:
- Acute neurological changes: Prompt neurological assessment and notification of the medical team are essential if symptoms such as seizures, weakness, or altered mental status develop.
- Radiation-induced edema: Watch for increasing headache, confusion, or neurological decline; administer steroids as prescribed and monitor response.
- Frame-related complications: Inspect pin sites for signs of infection or bleeding; provide wound care and educate the patient on signs of infection.
- Delayed radiation effects: Monitor for late complications such as cognitive impairment or radiation necrosis, which may occur weeks to months post-treatment.
Special Considerations
Pediatric Patients
Caring for children undergoing SRS requires age-appropriate education, involvement of parents or guardians, and strategies to minimize anxiety (e.g., play therapy, sedatives if necessary).
Patients with Cognitive Impairment
For those with existing cognitive deficits, nurses adapt communication and assess for unique risks such as impaired cooperation or misunderstanding of instructions.
REFERENCES
- Chukwueke U, Cavaliere R, Schiff D, Wen P and Huntoon K. Nervous System Metastases. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff’s Neurology in Clinical Practice. 8th ed. Philadelphia, PA. Elsevier: 1145-1164.
- Mahajan UV, Desai A, Shost MD, et al. Stereotactic radiosurgery and resection for treatment of multiple brain metastases: a systematic review and analysis. https://pubmed.ncbi.nlm.nih.gov/36321293/. Neurosurg Focus. 2022 Nov;53(5):E9.
- Vestibular schwannoma (acoustic neuroma) and neurofibromatosis. National Institute on Deafness and Other Communication Disorders. https://www.nidcd.nih.gov/health/vestibular-schwannoma-acoustic-neuroma-and-neurofibromatosis.
- National Cancer Institute (U.S.). Types of Radiation Therapy. https://training.seer.cancer.gov/treatment/radiation/radiation-types.html. Updated 12/21/2023.
- Niranjan A, Raju SS, Kooshkabadi A, Monaco E 3rd, Flickinger JC, Lunsford LD. Stereotactic radiosurgery for essential tremor: Retrospective analysis of a 19-year experience. https://pubmed.ncbi.nlm.nih.gov/28319282/. Mov Disord. 2017 May;32(5):769-777.
- Vellayappan B, Lim-Fat MJ, Kotecha R, et al. A Systematic Review Informing the Management of Symptomatic Brain Radiation Necrosis After Stereotactic Radiosurgery and International Stereotactic Radiosurgery Society Recommendations. https://pubmed.ncbi.nlm.nih.gov/37482137/. Int J Radiat Oncol Biol Phys. 2024 Jan;118(1):14-28.
- Stereotactic radiosurgery. American Association of Neurological Surgeons. http://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Stereotactic-Radiosurgery.
- Vlachos N, Lampros MG, Filis P, Voulgaris S, Alexiou GA. Stereotactic radiosurgery versus whole-brain radiotherapy after resection of solitary brain metastasis: A systematic review and meta-analysis. https://pmc.ncbi.nlm.nih.gov/articles/PMC9942116/. World Neurosurg X. 2023 Feb;18:100170.
- Yu JS, Suh JH, Ma L and Sahgal A. Radiobiology of Radiotherapy and Radiosurgery. In: Winn HR, ed. Youmans and Winn Neurological Surgery. 8th ed. Philadelphia, PA, Elsevier: 2257-2268.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





