Strictureplasty is a surgical technique developed to treat strictures, or narrowings, of the intestine—primarily in patients with Crohn’s disease—without removing any part of the bowel. This bowel-sparing approach has revolutionized the surgical management of intestinal strictures, offering patients relief from obstructive symptoms while preserving as much healthy bowel tissue as possible. Here, we explore the history, indications, types, techniques, outcomes, and future directions of strictureplasty.
Introduction to Strictureplasty
Strictures, or narrowed segments of the intestine, can result from chronic inflammation, scarring, and fibrosis, most commonly due to Crohn’s disease but also from tuberculosis, radiation enteritis, or ischemia. Traditionally, the surgical answer was resection—cutting out the affected segment. However, multiple resections can lead to short bowel syndrome, a condition where not enough bowel remains to absorb nutrients adequately. Strictureplasty, first described in the 1970s, provides an alternative by widening the narrowed segment and maintaining intestinal continuity.
Indications for Strictureplasty
The main indication for strictureplasty is the presence of symptomatic, obstructive, or multiple strictures in the small intestine due to Crohn’s disease, especially when patients have already undergone multiple resections or when the remaining bowel length is limited. Specific situations where strictureplasty is considered include:
- Multiple strictures in the small bowel
- Short strictures (less than 10 cm) not amenable to endoscopic dilation
- Recurrent strictures in previously resected patients
- Risk of short bowel syndrome if additional resections are performed
- Pediatric patients, where bowel preservation is crucial for growth
It is generally not recommended for strictures complicated by cancer, perforation, abscess, severe active infection, or massive hemorrhage.
Contraindications and Limitations
While strictureplasty is highly beneficial for many patients, it is not suited for every stricture. Contraindications include:
- Presence of malignancy in the stricture
- Involvement of the colon (due to risk of bacterial contamination)
- Strictures longer than 20 cm (relative contraindication)
- Extensive inflammation or perforation at the site
- Severe malnutrition or active sepsis
Each case must be individualized, weighing the benefits of bowel preservation against patient safety.
Types of Strictureplasty
Strictureplasty techniques are classified according to the length of the stricture and the complexity of the procedure:
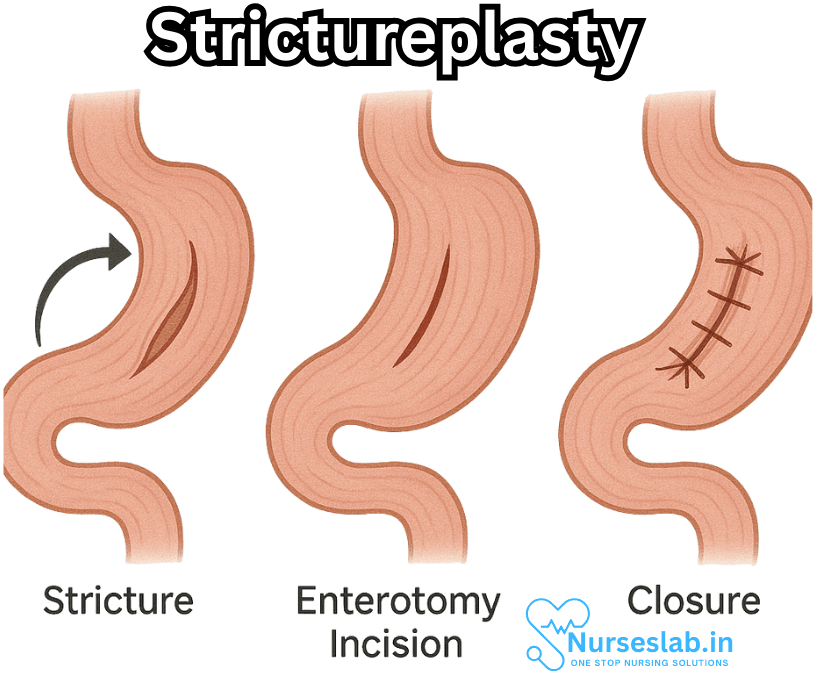
1. Heineke-Mikulicz Strictureplasty
Indication: Short strictures (up to 10 cm)
Technique: The most common and simplest technique. A longitudinal incision is made along the length of the stricture and then closed transversely. This widens the lumen without removing any tissue.
Advantages: Simplicity, speed, and effectiveness for short segments.
2. Finney Strictureplasty
Indication: Intermediate-length strictures (typically 10 to 20 cm)
Technique: The segment of bowel is folded onto itself in a U-shape, and a side-to-side opening is made and sewn together, creating a wider channel.
3. Michelassi Strictureplasty
Indication: Long strictures (greater than 20 cm)
Technique: An advanced, complex procedure. The diseased segment is divided almost completely, then the bowel ends are laid side-by-side and sutured, forming a new, wider lumen.
Other Variations
Other techniques such as the Jaboulay and the Kono-S procedure are sometimes used in specific circumstances or for specialized patient populations.
Surgical Technique and Principles
Regardless of specific technique, several key principles guide strictureplasty:
- Careful identification of the involved bowel segment
- Gentle handling to minimize trauma and preserve blood supply
- Meticulous closure to prevent leaks or fistulas
- Maintenance of luminal patency
- Use of absorbable suture material
The procedure is often performed through open surgery but can also be done laparoscopically in select centers.
Advantages of Strictureplasty
Strictureplasty offers several significant benefits over resection, particularly in patients with extensive or recurrent disease:
- Bowel Preservation: No loss of bowel length, reducing risk of short bowel syndrome
- Repeatable: Can be performed multiple times, even in the same patient or segment
- Low Morbidity: Lower risk of surgical complications associated with bowel loss
- Speed: Short operative times for simple techniques
- Reduced Hospital Stays: Quicker recovery and return to normal activities
Complications and Risks
As with any surgical procedure, strictureplasty carries certain risks, including:
- Infection or abscess formation
- Anastomotic leak or fistula
- Bleeding
- Recurrent stricture at the same or new site
- Impaired bowel motility
- Rarely, the development of carcinoma at the site of the strictureplasty
Close postoperative monitoring is essential, and patients should be educated about warning signs and the need for prompt medical attention if symptoms recur.
Outcomes and Prognosis
Multiple studies have shown strictureplasty to be highly effective in relieving obstructive symptoms and preserving bowel length. Long-term outcomes are generally excellent, with low rates of recurrence at the site of the strictureplasty. About 70-90% of patients remain symptom-free for years after surgery.
However, Crohn’s disease is a lifelong relapsing condition, and new strictures can develop elsewhere. The need for subsequent interventions is not uncommon, but the fact that strictureplasty can be repeated makes it a valuable tool in the long-term management of these patients.
Patient Recovery and Follow-Up
Recovery from strictureplasty is usually rapid, especially as bowel continuity is maintained. Patients typically resume oral intake within a few days and are discharged within a week. Follow-up includes:
- Assessment for wound healing and early complications
- Nutritional support and monitoring
- Monitoring for signs of recurrence
- Regular imaging (e.g., MRI, CT, or ultrasound) as appropriate
Dietary counseling and medication adjustments (such as immunosuppressants or biologics for Crohn’s disease) may be required.
Strictureplasty in Special Populations
Strictureplasty is particularly valuable in children, who may otherwise face severe growth and nutritional impairment from extensive bowel resections. It is also used in patients with previous surgeries, where little bowel remains, and in those with multiple or complex strictures.
Future Directions and Innovations
Ongoing research aims to refine strictureplasty techniques, improve laparoscopic and robotic approaches, and minimize complications further. Advances in pre- and post-operative medical management of Crohn’s disease are also expected to reduce the need for surgical intervention over time.50% of people who’ve had a strictureplasty will need another surgery.
Nursing Care of the Patient Undergoing Strictureplasty
As more patients with inflammatory bowel disease (IBD) undergo strictureplasty, the role of skilled nursing care throughout the perioperative period becomes increasingly pivotal. This document outlines the essential nursing responsibilities and holistic care principles for patients before, during, and after strictureplasty.
Preoperative Nursing Care
Assessment
- Comprehensive History and Physical Exam: Assess for comorbidities, nutritional status, medication use (especially immunosuppressants, steroids, and anticoagulants), allergy history, and previous abdominal surgeries.
- Baseline Laboratory Tests: Ensure completion of complete blood counts, electrolytes, coagulation profiles, and inflammatory markers. Blood type and cross-matching may be required.
- Preoperative Imaging: Confirm that relevant imaging studies (CT, MRI, or small bowel series) are available for surgical planning.
- Infection Screening: Assess for active infections and manage as appropriate. Screen for tuberculosis in those on biologic therapies.
Education and Preparation
- Procedure Explanation: Provide clear, jargon-free information about the rationale for strictureplasty, what to expect during surgery, and potential risks and benefits.
- Consent Process: Ensure informed consent is obtained, addressing all patient questions and concerns.
- Bowel Preparation: Educate the patient about any required bowel cleansing regimens, dietary restrictions, and instructions for fasting prior to surgery.
- Nutritional Optimization: Collaborate with dietitians to address malnutrition or deficiencies; patients may need supplements, enteral, or parenteral support before surgery.
- Preoperative Medications: Clarify which medications to continue or withhold. Patients on steroids may need stress-dose corticosteroids perioperatively.
- Pain Management Planning: Discuss postoperative pain expectations and available analgesic options.
- Psychological Support: Assess for anxiety or fears regarding surgery, and provide resources or referrals for counselling if needed.
Coordination and Logistics
- Verify surgical and anesthesia consents and preoperative checklists.
- Confirm NPO status and intravenous access.
- Ensure all preoperative antibiotics and venous thromboembolism (VTE) prophylaxis measures are initiated as per protocol.
Intraoperative Nursing Responsibilities
- Patient Advocacy: Maintain safety and dignity throughout positioning and surgical prep.
- Time-Out Procedure: Participate in surgical safety checks to confirm patient identity, procedure, and site.
- Aseptic Technique: Scrub nurses must vigilantly adhere to sterile technique to prevent surgical site infections.
- Fluid and Blood Management: Monitor estimated blood loss and fluid replacement; be alert for signs of hypovolemia or anaphylaxis.
- Documentation: Accurately record surgical events, specimen collection, and intraoperative medications.
- Collaboration: Communicate patient needs to the surgical and anesthesia teams promptly.
Immediate Postoperative Nursing Care
Assessment and Monitoring
- Vital Signs: Monitor for hemodynamic stability, including temperature, heart rate, blood pressure, respiratory rate, and oxygen saturation. Be vigilant for signs of bleeding, hypovolemia, or sepsis.
- Pain and Comfort: Assess pain frequently using standardized scales and administer analgesia as prescribed, balancing adequate control with avoidance of oversedation.
- Neurological Status: Monitor level of consciousness, especially after general anesthesia.
- Abdominal Assessment: Check for distension, tenderness, and signs of peritonitis or bowel obstruction. Listen for return of bowel sounds, which may be delayed postoperatively.
- Surgical Site: Inspect for signs of infection, bleeding, or wound dehiscence. Maintain dressing integrity and document drainage characteristics.
- Drain and Tube Care: Manage nasogastric tubes, surgical drains, and urinary catheters per protocol.
- Fluid Balance: Record input and output meticulously, including urine, drains, and emesis. Assess for fluid overload or deficit.
- Laboratory Monitoring: Track postoperative hemoglobin, white cell count, electrolytes, and markers of infection or inflammation.
Complication Surveillance
- Early Complications: Monitor for bleeding, anastomotic leak, intra-abdominal abscess, wound infection, and ileus.
- Late Complications: Watch for bowel obstruction, recurrent strictures, or fistula formation in the ensuing weeks.
Comfort and Psychosocial Support
- Provide reassurance and frequent orientation to reduce anxiety.
- Support early ambulation as tolerated to reduce risk of VTE and promote recovery.
- Encourage presence of family or support persons as appropriate, and facilitate communication with the healthcare team.
Ongoing Postoperative Care and Discharge Planning
Gastrointestinal Function and Nutrition
- Advance diet as tolerated, beginning with clear fluids and progressing to a low-residue diet per surgical and dietary recommendations.
- Assess for nausea, vomiting, and tolerance of oral intake.
- Monitor for signs of malabsorption or nutritional deficiencies, especially in patients with extensive bowel disease.
- Educate about the importance of hydration and balanced nutrition in healing.
Wound and Infection Care
- Teach the patient and caregivers how to care for incisions, recognize signs of infection, and report concerns promptly.
- Schedule follow-up wound assessments and suture or staple removal as needed.
- Review any restrictions on lifting, activity, or bathing as wounds heal.
Medication and Pain Management
- Ensure understanding of all prescribed medications, including antibiotics, pain relievers, or resumption of IBD therapies.
- Reinforce adherence to pain management regimens and safe use of opioids or adjunct medications.
Patient and Family Education
- Provide clear written and verbal instructions regarding postoperative care, warning signs of complications, and when to seek medical attention.
- Discuss the importance of maintaining regular follow-up and attending outpatient appointments for ongoing disease management and surgical review.
- Offer educational resources or support groups for patients with IBD and those who undergo bowel surgery.
Psycho-Social Considerations
- Recognize the emotional impact of chronic disease and surgery; screen for depression, anxiety, or adjustment difficulties.
- Provide or refer for counselling or mental health services as needed.
- Support social reintegration, return to work or school, and adaptation to lifestyle changes post-surgery.
Interdisciplinary Collaboration
Optimal outcomes for patients undergoing strictureplasty result from cohesive teamwork. Nurses coordinate with surgeons, gastroenterologists, dietitians, pharmacists, social workers, and physical therapists to ensure a comprehensive plan of care. Regular interdisciplinary rounds, case discussions, and shared documentation help address complex needs and streamline care transitions.
Promoting Quality of Life Post-Strictureplasty
By combining clinical expertise, technical proficiency, and compassionate patient education, nurses play a crucial role in supporting recovery and restoring independence after strictureplasty. Addressing not only the physical but also the emotional, nutritional, and psychosocial domains of health, nurses help patients achieve optimal outcomes and an improved quality of life.
REFERENCES
- Crohn’s and Colitis Foundation (U.S.). Strictureplasty. https://www.crohnscolitisfoundation.org/patientsandcaregivers/what-is-crohns-disease/treatment/surgery/strictureplasty
- Hoilat GJ, Rentea RM. Crohn Disease Stricturoplasty. https://pubmed.ncbi.nlm.nih.gov/32809432/. 2023 Jul 25. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan.
- Hesham W, Kann BR. Strictureplasty. Clin Colon Rectal Surg. 2013 Jun;26(2):80-3. doi: 10.1055/s-0033-1348045. PMID: 24436654; PMCID: PMC3709977.
- Ambe R, Campbell L, Cagir B. A comprehensive review of strictureplasty techniques in Crohn’s disease: types, indications, comparisons, and safety. J Gastrointest Surg. 2012 Jan;16(1):209-17. doi: 10.1007/s11605-011-1651-2. Epub 2011 Sep 10. PMID: 21909847.
- Mustafa W Aman, Strictureplasty Technique, Updated: Feb 08, 2023 , https://emedicine.medscape.com/article/1893397-technique?form=fpf
- Strong SA. Strictureplasty in Complex Crohn’s Disease: Beyond the Basics. https://pubmed.ncbi.nlm.nih.gov/31308832/. Clin Colon Rectal Surg. 2019 Jul;32(4):243-248.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





