Vaginoplasty is a surgical procedure designed to construct or reconstruct the vagina. It is performed for a variety of medical, reconstructive, and gender-affirming reasons. Over the years, vaginoplasty has evolved to encompass a range of techniques, each tailored to meet the individual needs of patients.
Introduction to Vaginoplasty
Vaginoplasty is a term that encompasses several surgical techniques intended to create or restore vaginal anatomy. While the procedure can be performed for medical or reconstructive reasons—such as following trauma, cancer, or congenital conditions—it is also a vital part of gender-affirming care for transgender women. The complexity, scope, and goals of vaginoplasty vary depending on the indication for surgery.
Historical Context
The origins of vaginoplasty date back to the early nineteenth century, when surgeons first attempted to address congenital absence of the vagina or injuries resulting from trauma or disease. Over time, advancements in surgical technique, anesthesia, and post-operative care have enabled safer and more effective outcomes. In recent decades, the development of gender-affirming approaches has made vaginoplasty a cornerstone in transgender healthcare.
Indications for Vaginoplasty
Vaginoplasty may be undertaken for several reasons, including:
- Congenital anomalies: Some individuals are born with conditions such as Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome or vaginal agenesis, which result in the absence or underdevelopment of the vagina. Vaginoplasty offers the possibility of constructing functional anatomy.
- Trauma or injury: Trauma, accidents, or surgical complications may necessitate reconstruction of the vaginal canal.
- Oncological reasons: Cancerous growths in the pelvic region may require surgical removal of tissue, including parts of the vagina, followed by reconstructive procedures.
- Gender-affirming surgery: For transgender women, vaginoplasty can create female genital anatomy as part of a broader transition process.
- Aesthetic or functional concerns: Some individuals may seek vaginoplasty for reasons such as vaginal tightening or to address symptoms of pelvic floor dysfunction.
Surgical Techniques
The approach to vaginoplasty depends on the underlying reason for surgery. Here are the most common techniques:
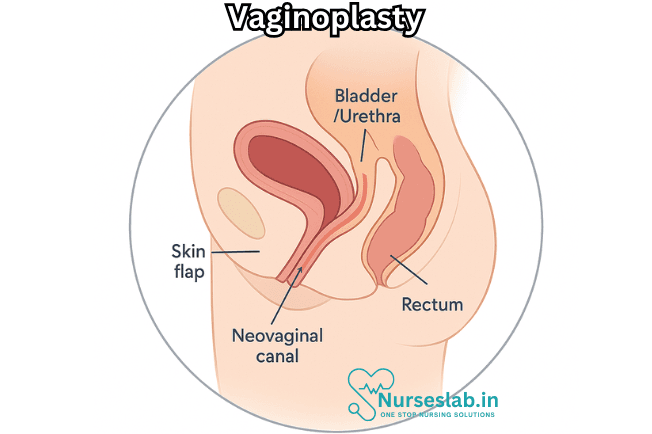
1. Penile Inversion Vaginoplasty
Most commonly employed in gender-affirming surgery for transgender women, penile inversion vaginoplasty uses the skin of the penis to create a vaginal canal. The glans and other tissue are modified to form the neoclitoris, while the labia are constructed from scrotal or other skin grafts.
2. Sigmoid Colon Vaginoplasty
For patients lacking sufficient penile or scrotal tissue, or when deeper vaginal canals are desired, a segment of the sigmoid colon may be used. This technique is also common in reconstructive cases following cancer or congenital anomalies.
3. Skin Graft Vaginoplasty
Split-thickness or full-thickness skin grafts from other parts of the body are used to line the neovaginal canal. This approach may be used when local tissue is insufficient.
4. Vecchietti Procedure
Often used for congenital vaginal agenesis, the Vecchietti procedure uses progressive dilation to create a neovagina, sometimes aided by laparoscopy.
5. Other Approaches
In select cases, tissue-engineered grafts, buccal mucosa, or gracilis muscle flaps may be employed to optimize outcomes.
Preoperative Preparation
Preparing for vaginoplasty involves careful evaluation and planning. Patients undergo a thorough medical history and physical exam. For those seeking gender-affirming surgery, psychosocial assessment and hormone therapy are typically part of the process. In all cases, imaging, laboratory tests, and consultations with multidisciplinary teams ensure readiness for surgery and optimal recovery.
The Surgical Procedure
Vaginoplasty is usually performed under general anesthesia. The duration of surgery varies with technique, complexity, and patient factors. Common steps include:
- Incision and preparation of donor tissue
- Creation or expansion of the vaginal canal
- Construction of the vaginal introitus and labia
- Formation or preservation of clitoral structures (for gender-affirming surgery)
- Closure and placement of drains or stents as needed
The procedure is often accompanied by cystoscopy or other intraoperative imaging to ensure proper anatomical relationships and identify any complications.
Postoperative Care and Recovery
After surgery, patients typically remain in hospital for several days to monitor for complications such as bleeding, infection, or issues with graft viability. Catheters, packing, and drains may be used temporarily. Pain management, antibiotics, and wound care are standard.
Recovery involves regular follow-up visits, wound checks, and instructions on dilation (if required) to maintain vaginal depth and width. Physical therapy, psychological support, and sexual health counseling may be offered to optimize outcomes. Most patients return to light activities within weeks, but full healing and return to normal function may take several months.
Risks and Complications
As with any surgery, vaginoplasty carries risks. Complications may include:
- Bleeding and infection
- Wound healing problems
- Fistula formation (abnormal openings between the vagina and adjacent structures)
- Stenosis (narrowing of the vaginal canal)
- Granulation tissue or scarring
- Loss of sensation or sexual function
- Difficulty with urination or bowel function
- Need for revision surgery
Most complications can be managed with prompt intervention, but some may require additional surgery or long-term care.
Outcomes and Satisfaction
Most patients report high levels of satisfaction following vaginoplasty, especially when the procedure is performed by experienced surgeons and accompanied by comprehensive pre- and postoperative care. Functional outcomes—including ability to engage in sexual activity, sensation, and overall quality of life—are generally favorable. For transgender patients, vaginoplasty can offer profound improvements in psychological well-being, body image, and social confidence.
Long-Term Follow-Up
Long-term follow-up is essential to monitor healing, maintain vaginal depth and width, and address any concerns related to sexual function, urinary or bowel health, and overall satisfaction. Dilatation, hygiene education, and sexual health counseling are provided as needed.
Psychological and Social Considerations
Vaginoplasty is not only a physical transformation but also a significant psychological and social milestone. Patients may benefit from support groups, counseling, and community resources to help navigate the changes in identity, relationships, and self-image. In many cases, the procedure is life-changing, contributing to increased self-esteem and personal fulfillment.
Nursing Care of Patients Undergoing Vaginoplasty
The nursing care of a patient undergoing vaginoplasty is holistic, encompassing physical, psychological, and educational support before, during, and after the procedure.
Preoperative Nursing Care
Preoperative care is crucial to prepare the patient physically and emotionally for surgery and to minimize postoperative complications.
Patient Assessment
- Comprehensive Evaluation: Obtain a thorough medical, surgical, and psychosocial history. Pay special attention to comorbidities (e.g., diabetes, hypertension), allergies, current medications, and history of previous surgeries.
- Psychosocial Support: Assess the patient’s psychological readiness and provide access to counseling services. For transgender patients, ensure that the necessary mental health assessments and documentation are in place as per WPATH or local guidelines.
- Informed Consent: Confirm that the patient understands the procedure, potential risks, complications, and the expected postoperative course.
- Preoperative Instructions: Educate the patient on preoperative fasting, medication management (including hormone therapy), and bowel preparations if required.
- Baseline Vitals and Labs: Record baseline vital signs, and ensure all required laboratory tests (CBC, electrolytes, coagulation profile, etc.) and imaging are completed.
Patient Education
- Discuss the surgical process, expected recovery timeline, and hospital stay duration.
- Explain perioperative procedures such as catheterization, use of drains, and pain management.
- Introduce the importance of postoperative care, including dilation routines, hygiene, and activity restrictions.
- Provide written educational materials to reinforce teaching.
Immediate Postoperative Nursing Care
The first 24–48 hours following vaginoplasty are critical. Close monitoring and prompt intervention help identify and manage complications early.
Monitoring and Assessment
- Vital Signs: Monitor temperature, blood pressure, heart rate, respiratory rate, and oxygen saturation at regular intervals.
- Pain Assessment: Assess pain using standard scales and provide analgesia as prescribed. Monitor for signs of uncontrolled pain, which can indicate complications.
- Surgical Site Observation: Inspect the surgical site for excessive bleeding, hematoma, swelling, or infection. Note the color, temperature, and integrity of the skin and mucosa.
- Catheter and Drain Care: Maintain patency of urinary catheters and surgical drains. Monitor urine output and drain contents for volume, color, and signs of infection.
- Neurovascular Checks: Assess sensation and movement in the lower extremities, especially if regional anesthesia was used.
Prevention and Management of Complications
- Hemorrhage: Monitor for signs of active bleeding, hypotension, or tachycardia. Notify the surgical team immediately if significant bleeding occurs.
- Infection: Maintain strict aseptic technique during dressing changes and catheter care. Monitor for fever, redness, discharge, or odor at the surgical site. Educate the patient on signs of infection.
- Venous Thromboembolism (VTE): Encourage early mobilization as tolerated. Apply sequential compression devices (SCDs) or anti-embolism stockings if prescribed. Administer prophylactic anticoagulants as ordered.
- Urinary Retention or Injury: Monitor catheter output closely. Be alert for signs of urinary tract infection or urinary retention after catheter removal.
- Wound Dehiscence or Necrosis: Inspect the surgical site for any breakdown or discoloration of tissue. Follow up immediately on any abnormal findings.
Pain and Comfort Management
- Administer prescribed analgesics, considering both opioid and non-opioid options.
- Encourage non-pharmacological pain relief methods such as positioning, relaxation techniques, and cold packs if appropriate.
- Provide emotional support and reassurance, acknowledging the significance of the procedure for the patient’s well-being.
Ongoing Postoperative Nursing Care
Continued care focuses on recovery, functional adaptation, and long-term well-being.
Wound Care
- Perform regular dressing changes using aseptic technique.
- Assess for healthy wound healing: pink, moist tissue without excessive discharge or odor.
- Monitor for granulation tissue and early signs of infection or delayed healing.
- Educate the patient on proper perineal hygiene, emphasizing gentle cleansing and patting dry.
Urinary Catheter Management
- Catheters are typically left in place for 5–7 days postoperatively. Monitor for patency, infection, or trauma.
- Educate the patient on catheter care and signs of urinary infection or retention after removal.
- Encourage a gradual return to normal voiding patterns once the catheter is removed.
Dilation and Neovaginal Care
- Teach the patient the correct technique for vaginal dilation, a critical aspect of postoperative care to prevent stenosis (narrowing of the neovagina).
- Educate on frequency, duration, and hygiene of dilation tools. Initially, dilation may be required several times daily, gradually reducing over months as healing progresses.
- Encourage the use of lubricants and gentle handling to avoid trauma.
- Emphasize the importance of long-term adherence to dilation protocols.
Mobility and Activity
- Encourage early, gentle ambulation to reduce the risk of VTE and promote bowel function.
- Advise restrictions on strenuous activity, heavy lifting, and sexual activity until cleared by the surgical team (often 6–12 weeks).
- Assist with ADLs (activities of daily living) as needed, especially in the early postoperative period.
Nutrition and Bowel Care
- Promote adequate hydration and a balanced diet to support healing.
- Monitor bowel movements and manage constipation proactively, as immobility and pain medications can contribute to GI sluggishness.
- Advise on gentle use of stool softeners or laxatives if needed.
Psychosocial and Emotional Support
Nursing care extends beyond the physical aspects to include the psychological and emotional well-being of the patient.
- Offer ongoing emotional support and validation, recognizing the profound importance of the procedure for the patient’s identity and mental health.
- Facilitate access to counseling and peer support groups, especially for transgender patients who may experience unique social or familial challenges.
- Encourage open communication, allowing the patient to express fears, expectations, or concerns.
- Address issues of body image, sexual health, and self-esteem, providing referrals to specialized services as needed.
Patient Education and Discharge Planning
Thorough education and clear discharge planning are vital for successful long-term outcomes.
Discharge Instructions
- Review wound care, hygiene, and signs of infection or complications.
- Provide written and verbal instructions on the dilation schedule, technique, and importance of adherence.
- Discuss restrictions on activities, lifting, and sexual intercourse, emphasizing the need for follow-up before resuming normal activities.
- List emergency symptoms that require immediate attention (e.g., fever, severe pain, heavy bleeding, difficulty urinating).
- Provide contact information for the surgical team and support services.
Follow-Up Care
- Schedule regular follow-up appointments with the surgical and nursing teams to monitor healing and address complications early.
- Encourage ongoing communication and questions between the patient and healthcare providers.
- Facilitate transition to primary care and, if appropriate, gynecological care for routine screening and health maintenance.
Special Considerations
- Cultural Sensitivity: Approach care with respect for the patient’s gender identity, cultural background, and personal values.
- Confidentiality: Maintain strict confidentiality regarding the patient’s medical and surgical history.
- Coordination of Care: Work closely with a multidisciplinary team, including surgeons, social workers, psychologists, and other allied health professionals.
REFERENCES
- American Academy of Cosmetic Surgery. Vaginal Rejuvenation. https://www.cosmeticsurgery.org/page/VaginalRejuvenation
- Bertrand B, Perchenet AS, Casanova D. Histoire de la vaginoplastie : évolution technique et sociologique [The history of vaginoplasty: Technical and sociological advances]. Ann Chir Plast Esthet. 2023;68(5-6):389-396. doi:10.1016/j.anplas.2023.07.001
- American Society of Plastic Surgeons. Gender Confirmation Surgeries. https://www.plasticsurgery.org/reconstructive-procedures/gender-affirmation-surgeries.
- American Society of Plastic Surgeons. What is a vaginoplasty?https://www.plasticsurgery.org/cosmetic-procedures/aesthetic-genital-plastic-surgery/vaginoplasty
- International Society of Aesthetic Plastic Surgery. Vaginal Tightening: Vaginoplasty and Perineoplasty. https://www.isaps.org/discover/patients-home/procedures/body-procedures/vaginal-tightening-vaginoplasty-and-perineoplasty/.
- Kachhawa G, Kriplani A. Management of Reproductive Tract Anomalies. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5425643/. J Obstet Gynaecol India. 2017 Jun;67(3):162-167.
- Li JS, Crane CN, Santucci RA. Vaginoplasty tips and tricks. https://pubmed.ncbi.nlm.nih.gov/32840336/. Int Braz J Urol. 2021 Mar-Apr;47(2):263-273.
- Dural Ö, Poyrazoğlu Ş. Conservative management of vaginal hypoplasia. J Clin Res Pediatr Endocrinol. 2020;12(Suppl 1):50-52. doi:10.4274/jcrpe.galenos.2020.2019.S0222
- Downing J, Holt SK, Cunetta M, Gore JL, Dy GW. Spending and out-of-pocket costs for genital gender-affirming surgery in the US. JAMA Surg. 2022;157(9):799-806. doi:10.1001/jamasurg.2022.2606
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





