Introduction
Myringotomy is a surgical procedure involving the creation of a small incision in the tympanic membrane, commonly known as the eardrum. The primary purpose of this intervention is to relieve pressure caused by the excessive accumulation of fluid or pus in the middle ear, or to allow for the drainage of these substances. Myringotomy is most often performed in conjunction with the insertion of a tympanostomy tube (commonly referred to as “ear tubes”), although the incision can also be left to heal naturally.
Anatomical Overview
To understand myringotomy, it is essential to have a basic knowledge of ear anatomy. The ear is divided into three regions: the outer ear, the middle ear, and the inner ear. The tympanic membrane separates the external auditory canal from the middle ear and plays a crucial role in sound transmission by vibrating in response to sound waves. The middle ear contains the ossicles (malleus, incus, stapes), which transmit vibrations to the inner ear, and is connected to the nasopharynx via the Eustachian tube, which helps equalize pressure.
Indications for Myringotomy
Myringotomy is recommended for a variety of medical conditions involving the ear, most notably:
- Otitis Media with Effusion (OME): This refers to the accumulation of non-infected fluid within the middle ear, often resulting in hearing loss or a sensation of fullness.
- Acute Otitis Media (AOM): This is an infection of the middle ear that may cause pain, fever, and, if left untreated, can lead to complications such as mastoiditis or hearing loss. Myringotomy may be necessary if the infection is severe or unresponsive to antibiotics.
- Recurrent Ear Infections: Children and adults who experience frequent middle ear infections may benefit from myringotomy with tube placement to allow continual drainage and ventilation of the middle ear.
- Barotrauma: This refers to ear injury caused by changes in pressure—common among divers, pilots, or individuals exposed to sudden altitude changes. Myringotomy can relieve pressure and prevent further damage.
- Chronic Eustachian Tube Dysfunction: When the Eustachian tube fails to ventilate the middle ear properly, leading to chronic fluid buildup, a myringotomy may be indicated.
- Complications of Middle Ear Disease: Conditions like mastoiditis or facial nerve paralysis may require urgent intervention, including myringotomy, to drain pus and reduce pressure.
Contraindications
Although myringotomy is generally considered a safe procedure, certain contraindications must be taken into account:
- Uncorrected bleeding disorders or coagulopathies
- Active infection of the external auditory canal (otitis externa)
- Unwillingness or inability to comply with post-operative care
- Absence of clear clinical indications for the procedure
The Myringotomy Procedure
Preoperative Preparation
Before performing a myringotomy, the patient undergoes a thorough auditory examination, including otoscopy, tympanometry, and sometimes audiometry. In children, general anesthesia is often used, while adults may receive local anesthesia. The external auditory canal is cleaned and sterilized to minimize infection risk.
Technique
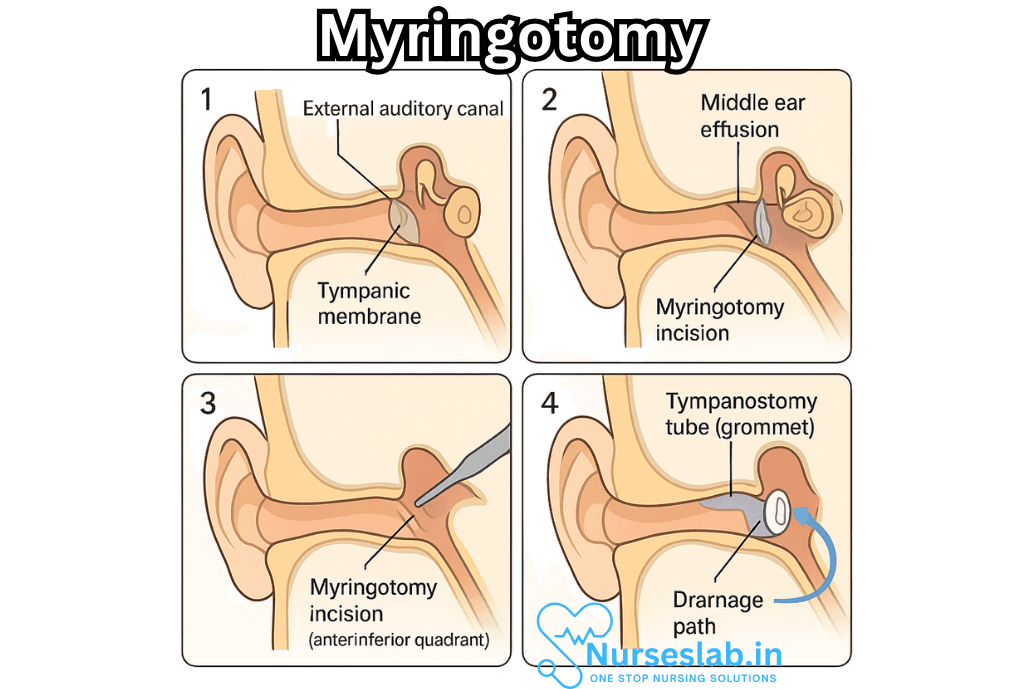
The procedure is typically performed as follows:
- The patient is positioned with the affected ear facing upward. Sterile drapes are applied.
- Using an operating microscope, the surgeon visualizes the tympanic membrane.
- A fine scalpel, myringotomy knife, or laser is used to make a small incision (usually in the anterior-inferior quadrant) of the eardrum.
- Fluid or pus from the middle ear is aspirated or allowed to drain spontaneously.
- If indicated, a tympanostomy tube is inserted into the incision to maintain patency and facilitate ongoing drainage and ventilation.
- The procedure typically takes less than 15 minutes and can be performed in an outpatient setting.
Types of Tympanostomy Tubes
Tympanostomy tubes are small cylinders typically made from silicone, fluoroplastic, or metal. There are several types:
- Short-term tubes: Designed to remain in place for 6–12 months; they usually fall out on their own.
- Long-term tubes: Have flanges to keep them in position for longer periods (up to several years) and may require removal by a physician.
Postoperative Care
Care after a myringotomy is generally straightforward:
- The patient is observed briefly for complications such as bleeding or dizziness. Most can resume normal activities within a day, though swimming or getting water in the ear may be restricted.
- Pain is usually mild and managed with acetaminophen or ibuprofen.
- If a tympanostomy tube is placed, instructions are provided regarding ear protection and signs of infection (e.g., drainage, fever, or persistent pain).
- Follow-up appointments ensure healing and tube function; the tubes are monitored until they fall out or are removed.
- Antibiotic ear drops may be prescribed if infection is suspected or confirmed.
Potential Complications
Myringotomy is considered safe, but like all surgical procedures, it carries risks:
- Perforation of the Tympanic Membrane: The incision typically heals within a few weeks after the tube falls out, but occasionally a persistent perforation may require surgical repair (tympanoplasty).
- Infection: Otorrhea (ear drainage) may occur post-procedure; this is usually managed with topical antibiotics.
- Sclerosis or Scarring: The formation of scar tissue (tympanosclerosis) may be observed but usually does not affect hearing.
- Tube Blockage or Displacement: Tubes may become blocked with debris or fall out prematurely, necessitating replacement if clinically indicated.
- Hearing Loss: Rarely, temporary or permanent hearing changes can occur.
Benefits of Myringotomy
The advantages of myringotomy include:
- Immediate relief of symptoms (pain, pressure, and hearing loss)
- Reduction in the recurrence of ear infections
- Prevention of complications associated with chronic middle ear fluid, such as speech and language delays in children
- Facilitation of the healing of the middle ear
- Improvement in the quality of life for patients with chronic ear problems
Myringotomy in Pediatric Practice
Myringotomy is one of the most commonly performed surgeries in children, particularly those with recurrent otitis media or persistent effusion that impacts hearing and speech development. Ear tube placement has been shown to significantly reduce the number of infections and to improve hearing outcomes in affected children.
Myringotomy in Adults
While less common in adults, myringotomy may be recommended for those with underlying risk factors such as chronic sinus problems, nasopharyngeal tumors, or anatomical differences that predispose to Eustachian tube dysfunction.
Alternatives to Myringotomy
Alternative treatments to myringotomy include watchful waiting, oral or topical antibiotics, autoinflation, or treatment of underlying allergic or sinus conditions. The decision to proceed with surgery is based on the severity of symptoms, frequency of infections, and impact on quality of life.
Nursing Care of the Patient Undergoing Myringotomy
Myringotomy is most commonly performed in children with recurrent otitis media but may also be indicated in adults for chronic middle ear effusions or barotrauma. As nurses play a pivotal role throughout the perioperative process, their responsibilities span patient education, emotional support, technical care, monitoring, and holistic support.
Preoperative Nursing Care
Patient Assessment and Preparation
- Comprehensive Assessment: Obtain a detailed health history focusing on episodes of ear infections, hearing loss, allergies, current medications (including anticoagulants or steroids), and prior surgical experiences.
- Physical Examination: Assess for current infection, fever, upper respiratory symptoms, and the general condition of the eardrum. Document findings and notify the surgeon of any contraindications (e.g., acute infection may postpone elective myringotomy).
- Laboratory Investigations: Ensure required blood tests or coagulation profiles are up-to-date, especially in patients with known bleeding disorders.
Psychological Preparation
- Education: Explain the procedure, including its purpose, technique, and expected outcomes, using age-appropriate language and visual aids, particularly for children.
- Consent: Ensure informed consent is obtained from the patient (or guardian), answering all questions honestly and sensitively.
- Anxiety Reduction: Provide emotional reassurance, encourage expression of fears, and involve family members/caregivers in the preparatory process.
Preoperative Instructions
- NPO Guidelines: Advise on fasting requirements if general anaesthesia is planned, including clear instructions about when the last meal or drink is permitted.
- Medication Management: Clarify which routine medications should be continued or withheld on the day of surgery (as per physician’s orders).
- Physical Preparation: Ensure the external ear is clean, and if requested, assist with preoperative antiseptic cleaning. Remove jewellery and ensure the patient is dressed appropriately for theatre.
Intraoperative Nursing Care
Assisting in the Operating Room
- Sterile Technique: Maintain strict aseptic technique during the preparation of the surgical field and handling of instruments.
- Patient Positioning: Assist with correct positioning of the patient (usually supine with the head turned to the side) to provide optimal access to the ear.
- Monitoring: Observe vital signs carefully, especially if general anaesthesia is used. Be prepared to assist with airway management in paediatric cases.
- Instrument Handling: Ensure all necessary instruments (microsurgical blades, suction, grommets if indicated) are available and functioning.
- Specimen Collection: If middle ear fluid is aspirated for culture, handle specimens carefully and label them accurately for laboratory analysis.
Postoperative Nursing Care
Immediate Postoperative Period
- Recovery Monitoring: Monitor the patient closely for return of consciousness, stable vital signs, and airway patency, especially in children after anaesthesia.
- Pain and Discomfort: Assess for pain, irritability, or nausea. Administer prescribed analgesics or antiemetics as needed. Use non-pharmacological comfort measures such as distraction for younger children.
- Bleeding and Discharge: Inspect the ear for excessive bleeding, persistent drainage, or foul-smelling discharge, and report abnormal findings to the physician promptly.
- Dizziness or Vertigo: Educate patients to report feelings of dizziness or imbalance, as these may occur briefly after the procedure.
Ongoing Care and Patient Education
- Ear Protection: Instruct patients and caregivers to keep the operated ear dry. Recommend using earplugs or a waterproof barrier during bathing and to avoid swimming unless specifically allowed by the surgeon.
- Signs of Complications: Educate about symptoms warranting immediate medical attention, such as persistent pain, fever, profuse bleeding, or purulent discharge.
- Follow-Up Visits: Stress the importance of attending scheduled follow-up appointments for hearing assessment and tube monitoring or removal if inserted.
- Medication Adherence: Reinforce completion of prescribed antibiotic or analgesic courses to prevent infection or recurrence.
- Activity Restrictions: Explain when normal activities, including school or work, can be resumed and what physical exertion or pressure changes to avoid temporarily.
Special Considerations
Pediatric Considerations
- Offer age-appropriate explanations and comfort items (toys, blankets).
- Allow parental presence during induction and recovery whenever possible.
- Monitor for separation anxiety and postoperative behavioural changes, providing emotional support as needed.
Adult and Elderly Considerations
- Assess for comorbidities that may impact healing (e.g., diabetes mellitus, immunosuppression).
- Monitor for potential hearing improvement or persistent deficit post-procedure and refer for audiology support if indicated.
Holistic and Culturally Sensitive Care
- Respect the patient’s cultural values, beliefs, and practices regarding surgical interventions and recovery.
- Provide interpreter services if required for non-native speakers to ensure understanding and informed consent.
- Offer information about community resources, support groups, or online forums for families managing recurrent ear problems.
Documentation and Communication
- Document all care activities, assessments, interventions, patient responses, and education provided in a timely and thorough manner.
- Report promptly to the treating provider any significant changes in condition, abnormal findings, or complications.
- Ensure informed consent forms, operative reports, and postoperative instructions are filed accurately in the patient’s records.
Legal and Ethical Considerations
- Uphold patient confidentiality at all times.
- Ensure that informed consent is properly obtained and documented.
- Respect patient autonomy in decisions regarding the use of ventilation tubes or further surgical interventions.
Transition Planning
- Coordinate the transition from inpatient to outpatient care, ensuring the patient and caregivers have clear verbal and written instructions for home management.
- Arrange for prompt follow-up care and audiology assessments as indicated.
REFERENCES
- Cole L, Nuttall T. Clinical Techniques: When and how to do a myringotomy – a practical guide. Vet Dermatol. 2021 Jun;32(3):302-e82. doi: 10.1111/vde.12966. Epub 2021 May 6. PMID: 33955092.
- American Academy of Otolaryngology-Head and Neck Surgery. Clinical Indicators: Myringotomy and Tympanostomy Tubes. https//www.entnet.org/resource/clinical-indicators-myringotomy-and-tympanostomy-tubes/). Last updated 4/22/2021.
- Merck Manual, Consumer Version. Myringotomy: Treating Secretory Otitis Media. https://www.merckmanuals.com/home/multimedia/table/myringotomy-treating-secretory-otitis-media.
- AskMayoExpert. Tympanostomy/pressure equalization (PE) tubes (child). Mayo Clinic; 2022.
- Merck Manual, Professional Version. Otitis Media (Serous). https://www.merckmanuals.com/professional/ear-nose-and-throat-disorders/middle-ear-and-tympanic-membrane-disorders/otitis-media-serous. Last reviewed 1/2024.
- Patel AA, Weber PC, Levi JR. The effect of tympanostomy tubes on otoacoustic emissions. https://pubmed.ncbi.nlm.nih.gov/38698162/. Eur Arch Otorhinolaryngol. 2024 Sep;281(9):4635-4639.
- Williams MP, Tudeen M, Orlando FA, Malaty J. Otology: Ear Infections. https://pubmed.ncbi.nlm.nih.gov/39018127/. FP Essent. 2024 Jul;542:23-28.
Stories are the threads that bind us; through them, we understand each other, grow, and heal.
JOHN NOORD
Connect with “Nurses Lab Editorial Team”
I hope you found this information helpful. Do you have any questions or comments? Kindly write in comments section. Subscribe the Blog with your email so you can stay updated on upcoming events and the latest articles.





